Anesthesia for Cardiac Surgery
Management of anesthesia for cardiac surgery requires a thorough understanding of normal and altered cardiac physiology; knowledge of the pharmacology of anesthetic, vasoactive, and cardioactive drugs; and familiarity with the physiologic derangements associated with cardiopulmonary bypass (CPB) and specific surgical procedures (Skubas N, Lichtman AD, Sharma A, Thomas SJ. Anesthesia for cardiac surgery. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Ortega R, Stock MC, eds. Clinical Anesthesia. Philadelphia: Lippincott Williams & Wilkins; 2013:1076–1111).
I. Coronary Artery Disease (Cad)
Prevention or treatment of myocardial ischemia during coronary artery bypass graft (CABG) surgery decreases the incidence of perioperative myocardial infarction (MI). Optimizing oxygen delivery to the myocardium is equally important for hemodynamic management.
Myocardial Oxygen Demand. The principal determinants of myocardial oxygen demand are wall tension and contractility. Interventions that prevent or promptly treat ventricular distention and decrease myocardial oxygen consumption decrease myocardial oxygen demand.
Myocardial Oxygen Supply. Increases in myocardial oxygen requirements can only be met by increasing coronary blood flow.
Coronary Blood Flow (Table 38-1)
The left ventricular subendocardium is most vulnerable to ischemia because myocardial oxygen requirements are high, and predictable perfusion can occur only during diastole. The time available for diastole decreases with an increasing heart rate.
A low ventricular filling pressure is desirable for improving perfusion (higher pressure gradient) and decreasing myocardial oxygen requirements (decreased ventricular volume and wall tension).
It is common during anesthesia for patients to exhibit signs of myocardial ischemia without any change in
blood pressure, heart rate, or ventricular filling pressure.
Table 38-1 Determinants of Coronary Blood Flow
Perfusion pressure
Vascular tone
Time available for perfusion (heart rate)
Severity of intraluminal obstructions
Presence of collateral circulation
Hemodynamic Goals
Although the precise relationship between intraoperative myocardial ischemia and postoperative MI remains controversial, there is consensus that a primary goal of a successful anesthetic is the prevention of myocardial ischemia.
Combinations of anesthetics, sedatives, muscle relaxants, and vasoactive drugs are selected to decrease myocardial oxygen requirements and thus prevent or decrease the likelihood of myocardial ischemia.
Pharmacologic agents that may benefit patients with CAD include statins and angiotensin-converting enzyme (ACE) inhibitors (stabilize atherosclerotic plaques) and volatile anesthetics (anesthetic preconditioning).
Monitoring for Ischemia. The ideal monitoring technique for detecting myocardial ischemia is not yet available (Table 38-2).
Selection of Anesthesia. There is no one ideal anesthetic for patients with CAD. The choice of anesthetic depends
primarily on the extent of pre-existing myocardial dysfunction and the pharmacologic properties of the specific drugs. Myocardial depression and associated decreases in myocardial oxygen requirements are only harmful in a patient whose heart cannot be further depressed without precipitating congestive heart failure.
Table 38-2 Monitoring for Myocardial Ischemia
Electrocardiogram (ST segment analysis of leads V5 and II)
Heart rate and blood pressure (rate-pressure product is not a sensitive predictor of myocardial ischemia)
Pulmonary artery catheter (V waves reflect ischemia-induced papillary muscle dysfunction but are probably not a sensitive indicator of myocardial ischemia)
TEE (regional wall motion abnormalities are the most sensitive indicator of myocardial ischemia)
TEE = transesophageal echocardiography.
Early tracheal extubation is popular for both on- and off-pump cardiac procedures. Volatile anesthetics in combination with low-dose opioids or total intravenous (IV) anesthesia with short-acting drugs (midazolam, alfentanil, propofol) have been used to facilitate the likelihood of early tracheal extubation. Neuraxial opioids placed before induction of anesthesia decrease postoperative pain and facilitate early tracheal extubation.
Opioids lack myocardial depressant effects and are useful in patients with severe myocardial dysfunction. In critically ill patients, opioids such as fentanyl (50–100 μg/kg IV) can be administered as the sole anesthetic. In patients with good left ventricular function, opioids may be inadequate to depress sympathetic nervous system activity, requiring the addition of a volatile anesthetic or vasoactive drug.
Inhalation anesthetics have the advantages of dose dependency; easily reversible, titratable myocardial depression; amnesia; and reliable suppression of sympathetic nervous system responses to surgical stress and CPB. Disadvantages include myocardial depression, systemic hypotension, and lack of postoperative analgesia.
Combinations of opioids and volatile anesthetics may produce the advantages of each with minimal undesirable side effects. It is likely that any volatile anesthetic could be used as a balanced technique.
Isoflurane is a coronary vasodilator (more so than other volatile anesthetics), but this effect is clinically insignificant in doses below 1 minimum alveolar concentration (MAC). There is no evidence of an increased incidence of myocardial ischemia or worsened outcome.
Desflurane and sevoflurane possess hemodynamic profiles similar to isoflurane but have the advantage of faster recovery. A sudden increase in the inspired concentration of desflurane may result in increased heart rate, systemic blood pressure, and plasma epinephrine concentration.
Intravenous Sedative–Hypnotics. An alternative adjuvant anesthetic to the low-dose opioid technique is a titratable infusion of a short-acting sedative (propofol, midazolam, dexmedetomidine) that can be continued after surgery and after discontinuation affords a predictable and fairly rapid awakening.
Treatment of Ischemia. Anesthetics or vasoactive drugs that enable the heart to return to a slower rate, smaller size, and well-perfused state are frequently essential during anesthesia (Table 38-3).
Nitrates. Nitroglycerin is the drug of choice for the treatment of coronary vasospasm. As a venodilator, this drug decreases venous return and decreases ventricular filling pressures and thus wall tension.
Vasoconstrictors. Phenylephrine increases myocardial oxygen requirements, but this increase is offset by improvements in oxygen delivery produced by the increased coronary perfusion pressure.
β-blockers. β-blockade improves myocardial oxygen balance by preventing or treating tachycardia and by decreasing contractility. Atenolol improves long-term survival in patients with heart disease undergoing noncardiac surgery.
Table 38-3 Treatment of Intraoperative Myocardial Ischemia
Event Associated with Ischemia
Treatment*
Increased blood pressure and pulmonary wedge pressure
Increase anesthetic depth
Nitroglycerin (0.5–3.0 μg/kg/min IV)
Sodium nitroprusside (0.5–3.0 μg/kg/min IV)
Increased heart rate
β-Antagonists
Calcium channel blockers
Decreased blood pressure
Decrease anesthetic depth
Phenylephrine
Decreased blood pressure and increased pulmonary capillary wedge pressure
Phenylephrine
Nitroglycerin
Inotrope
Normal hemodynamics
Nitroglycerin
Calcium channel blocker
* The goal is to return the heart to a slow, small, perfused state.
IV = intravenous.
Table 38-4 Guidelines for Coronary Artery Bypass Graft Surgery
Volatile agent–based anesthetic (facilitate early tracheal intubation)
Adequate perioperative analgesia
Anesthesia care by an experience anesthesiologist (TEE-trained)
Utilization of intraoperative TEE
- Evaluation of acute, persistent and life-threatening hemodynamic changes
- Monitoring of ventricular function and regional wall motion abnormalities
Management that augments coronary perfusion pressure (reduce risk of perioperative myocardial ischemia and infarction)
Administration of β-blockers (reduce the risk of atrial fibrillation and cardiac mortality)
Administration of ACE inhibitors or angiotensin receptor blockers preoperatively
Selective use of a pulmonary artery catheter
Multimodal approach for management of perioperative bleeding and transfusion
- Lysine analogues
- Point-of-care testing
- Discontinuation of antiplatelet medications for at least 5 days preoperatively
ACE = angiotensin-converting enzyme; TEE = transesophageal echocardiography.
- Evaluation of acute, persistent and life-threatening hemodynamic changes
Calcium channel blockers are useful in slowing the ventricular response in atrial fibrillation and flutter, as coronary vasodilators, and in the treatment of perioperative hypertension (clevidipine better than sodium nitroprusside [SNP] or trinitroglycerin [TNG]).
Guidelines for Coronary Artery Bypass Graft Surgery (Table 38-4)
II. Valvular Heart Disease
Valvular heart disease is characterized by pressure or volume overload of the atria or ventricles. Transesophageal echocardiography (TEE) has become a commonly used monitor in the perioperative management of patients undergoing cardiac surgery.
Aortic Stenosis
The normal aortic valve is composed of three semilunar cusps attached to the wall of the aorta. The normal annular diameter is 1.9 to 2.3 cm with an aortic valve
area of 2 to 4 cm2. The normal diameter of the left ventricular outflow tract is 2.2 cm.
Pathophysiology (Fig. 38-1). Chronic obstruction to left ventricular ejection results in concentric ventricular hypertrophy, which makes the heart susceptible to myocardial ischemia even in the absence of CAD. Because the ventricle is stiff, atrial contraction is critical for ventricular filling and stroke volume.
Anesthetic Considerations. Maintenance of adequate ventricular volume and sinus rhythm is crucial. If hypotension develops, it must be treated early to prevent the catastrophic cycle of hypotension-induced ischemia, subsequent ventricular dysfunction, and worsening hypotension. Bradycardia is a common cause of hypotension in patients with aortic stenosis.
Hypertrophic cardiomyopathy is a genetically determined disease characterized by development of a hypertrophic intraventricular septum, resulting in left ventricular outflow
obstruction (resembling aortic stenosis). Outflow obstruction is increased by increases in myocardial contractility or heart rate or decreases in preload or afterload. Anesthetic management is based on maintenance of left ventricular filling and controlled myocardial depression.
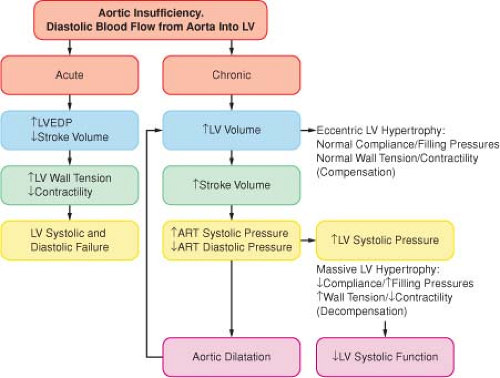
Figure 38-2. The pathophysiology of aortic insufficiency. ART = arterial; LV = left ventricle; LVEDP = left ventricular end-diastolic pressure.
Aortic Insufficiency
Pathophysiology (Fig. 38-2). Chronic volume overload of the left ventricle evokes eccentric hypertrophy but only minimal changes in filling pressures.
Anesthetic Considerations. Maintenance of adequate ventricular volume in the presence of mild vasodilation and increases in heart rate is most likely to optimize forward left ventricular stroke volume. An incompetent aortic valve may prevent the delivery of cardioplegia to the coronary system to produce diastolic arrest of the heart. (The alternative is injecting cardioplegia directly into the coronary ostia or into the coronary sinus.)
Mitral Stenosis
Pathophysiology (Fig. 38-3). Increased left atrial pressure and volume overload are inevitable consequences of the narrowed mitral orifice. Persistent increases in left atrial pressure are reflected back through the pulmonary
circulation, leading to right ventricular hypertrophy and perivascular edema in the lungs.

Figure 38-3. The pathophysiology of mitral stenosis. AF = atrial fibrillation; LA = left atrium; LV = left ventricle; PA = pulmonary artery; RV = right ventricle.
Anesthetic Considerations. Avoiding tachycardia is crucial for preventing inadequate left ventricular filling with concomitant hypotension. Continued preoperative administration of digitalis and β-antagonists, selection of anesthetics with minimal propensity to increase heart rate, and achievement of an anesthetic depth sufficient to suppress sympathetic nervous system responses are recommended.
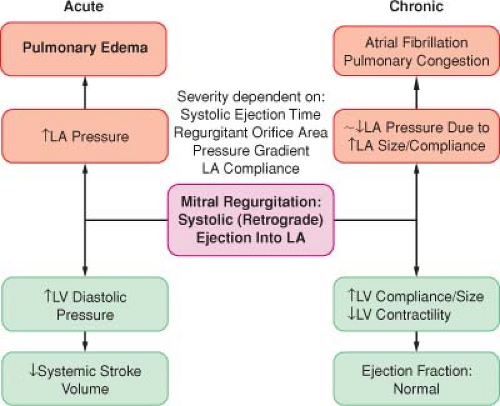
Mitral Regurgitation
Pathophysiology (Fig. 38-4). Chronic volume overload of the left atrium is the cardinal feature of mitral regurgitation.
Anesthetic Considerations. Selection of anesthetics that promote vasodilation and increase the heart rate is useful.
III. Aortic Diseases
Aortic dissection is characterized by rapid development of an intimal flap separating the true and false lumens. Severe
chest pain (dissection of the ascending aorta) or back pain (descending aorta dissections) is the most common presenting symptom. A variety of diagnostic techniques (contrast-enhanced computed tomography, TEE, magnetic resonance imaging) are accurate in the diagnosis of acute aortic dissection. Surgery is the definitive treatment for ascending aortic dissections.
Anesthetic Considerations. Acute aortic dissection is a surgical and anesthetic emergency necessitating IV access and invasive monitoring, including TEE.
Aortic Aneurysm. Thoracic aneurysms may involve one or more aortic segment (aortic root, ascending aorta, arch, descending aorta). The surgical replacement of an aortic arch aneurysm requires circulatory arrest and introduces the risk of global cerebral ischemia. Surgical replacement of the descending aorta is associated with postoperative paraplegia secondary to interruption of spinal cord blood supply.
Anesthetic Considerations. The anesthetic technique is focused on preservation of cardiac function (descending
thoracic aortic aneurysm) and neurologic integrity (aortic arch or descending thoracic aneurysms). Drainage of cerebrospinal fluid improves spinal cord perfusion pressure. Left heart bypass (left atrium to femoral artery) provides nonpulsatile retrograde aortic perfusion.
IV. Cardiopulmonary Bypass
Incorporates a circuit to oxygenate venous blood and return it to the patient’s arterial circulation (Table 38-5 and Fig. 38-5).
Blood Conservation in Cardiac Surgery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree