• Infant chest wall deforms easily → because of cartilaginous structure
• Accessory muscles provide limited support (poor anatomic rib configuration)
• Infantile diaphragm contains 20–25% of fatigue-resistant type I muscle fibers → paradoxical chest wall movement when there is ↑ inspiratory effort
• ↑ work of breathing → deterioration into resp failure, esp in premature infant
• FRC similar in both infants & adults per kg
• Owing to limited elastic recoil, infant closing capacity may near/exceed FRC:
Leads to air trapping → when small airways close at end-expiration
Cause of age-related changes in PaO2
• ↑ tracheal compliance in infants; can lead to dynamic tracheal collapse
• Changes in PaO2, PaCO2, & pH control ventilation → act on chemoreceptors
• Degree of response directly related to gestational & postnatal age
• Hypoxia stimulates newborn resp effort; high conc of O2 may depress it
• Nonspecific factors (blood glucose, Hct, temp) also affect infant breathing
Cardiovascular
• Infant/neonatal myocardium contains less contractile tissue than adult heart
• Neonatal ventricle less compliant during diastole & generates less tension
• Infant ventricle cannot adequately ↑ stroke volume when metabolic needs ↑
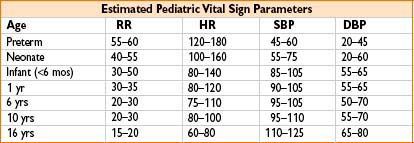
• Cardiac output proportional to changes in heart rate
• Bradycardia → ↓ cardiac output; factors contributing to bradycardia (hypoxia, hypercarbia, surgical manipulation) should be corrected
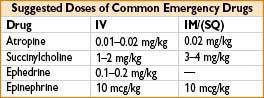
• Consider empiric anticholinergic admin (atropine) to offset laryngoscopy-induced bradycardia
Renal
• Kidneys very active in utero & produce copious amounts of urine (contribute to maintenance of amniotic fluid volume)
• At birth GFR = 15–20% of adult levels; reaches 50% within 2 wks & 100% by 1 yr (low GFR means infants cannot excrete excessive fluid loads/renal cleared drugs)
• Ability to excrete organic acids poorly developed in neonates (causes observed “physiologic acidemia” of newborn)
• Concentrating ability poor & newborns can conc urine only to 600–800 mOsm/kg
Hepatic
• Gluconeogenesis & protein synthesis begin at 12 wks’ gestation (liver structure near term similar to adults; functional development lags)
• Preterm & small for gestational age infants usually have diminished glycogen stores
→ Prone to hypoglycemic episodes after delivery
→ Treat hypoglycemia promptly (D10 at 4 mL/kg/hr)
• Albumin levels in preterm infants are often low and affect drug binding & availability
• Physiologic jaundice: Due to RBC breakdown & ↑ enterohepatic circ of bilirubin
→ As opposed to pathologic jaundice (encephalopathy from kernicterus)
Gastrointestinal
• Esophageal tone ↓ in many newborns; reaches adult level ≈6 wks
→ Projectile vomiting after feeding = classic sign of pyloric stenosis
• Meconium (water, pancreatic secretions + intestinal epithelial cells)
• Usually passed a few hours following delivery
• Premature infants often have delayed evacuation
• May also indicate GI dz (meconium ileus/intestinal atresia)
Hematopoietic
• Neonatal estimated blood volume = 85–90 mL/kg at term, gradually ↓ with age
• HbF: Most prevalent after birth, greater O2 affinity than HbA (adult)
• “Physiologic anemia of infancy” due to HbF (replaced with HbA by 3 mos)
• Hg levels rise to 12–13 g/dL by age 2; in adults, they reach 14 for females & 15.5 for males
• Vit K–dependent coag factors ≈40% adult levels (2° to immature liver synthesis)
• Prolonged PT normally seen in both preterm & full-term infants
Neurologic
• Brain growth phases: (1) Neuronal cell division (15–20 wks’ gestation) & (2) glial cell division (25 wks–2 yrs); myelination continues into 3rd yr
• Malnutrition, disruption of blood–brain barrier, & trauma may affect development
• Developmental milestones represent average rate of neurologic maturation
• Deviations from norm do not necessarily indicate significant problems
• Premature infant’s developmental delay may be considered normal (depending on degree of prematurity)
Temperature Regulation
• Infants lose heat rapidly 2° to: ↑ surface area:wt ratio, lack of adipose/SQ tissues
• Infants rely on nonshivering thermogenesis
• Cathecholamine-mediated increase in brown fat metabolic activity
→ Catecholamines also cause: Pulm & peripheral vasoconstriction, ↑ O2 use, hypoxia, acidemia
• Effective methods for limiting heat loss include
• ↑ ambient room temp, cover infant with thermal insulator, use of heat lamp
PHARMACOLOGY
Body Fluid Composition
• TBW in infants ≈85%, ≈60% by 1 yr of age; extracellular water (ECW) dec faster than intracellular water (ICW)
• Fat, muscle, organ wt are age dependent, affect pharmacodynamics/kinetics
• Infants have greater ECW than adults → volume of distribution for drugs is expanded
• Drugs with limited tissue uptake may require higher wt-based dosing
Organ System Maturity
• Enzyme systems involved in biotransformation relatively immature
• Drugs may have prolonged elimination half-lives
Protein Binding
• Often only unbound drug is clinically active (many drugs are protein bound)
• Albumin is the major binding protein for acidic drugs (benzos & barbiturates)
• Neonatal albumin quantitatively & qualitatively deficient → dec binding capacity
Receptors
• Age-related variations in response to drugs may be 2° to receptor sensitivities
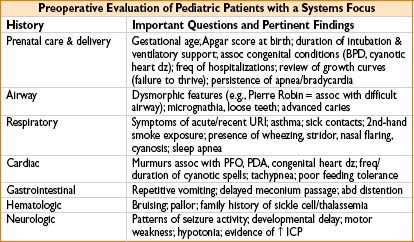
PREOPERATIVE EVALUATION
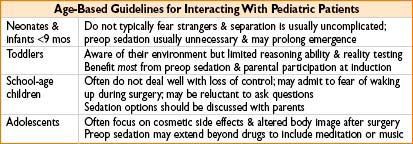
Psychological Assessment
• Use clear, simple language to discuss potential risks (avoid disclosing info in a child’s presence that may ↑ anxiety)
• Psychological goals of the preoperative interview
• Identify specific causes of anxiety & evaluate potential benefit of preop sedation
• Address potential risks pertinent to procedure
• Describe reasonable expectations for postop discomfort, side effects
• Reassure both parents & patient
• Child-life specialists can facilitate pt education & relieve anxiety
• Comfort objects may accompany pt into OR
• Parental presence may be useful; perceived legal risks are largely exaggerated

OR EQUIPMENT AND SETUP
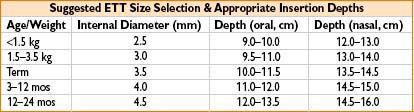
• Oral ETT size ≈ (age/4) + 4; depth ≈ (ETT internal diameter × 3)
Intravenous Fluids
• Fluid replacement: Based on NPO deficit, ongoing maintenance requirement, blood loss, & potential for surgically induced fluid shifts (3rd spacing)
• Lactated Ringer’s often appropriate
• Normal saline advised for pts with renal dysfx, mitochondrial myopathy, or neurosurgical procedures
• Dextrose soln for neonates (limited glycogen stores) & diabetes who got hypoglycemic meds
• “Buretrol” or other metered device often used for children <6 mos
• Allows careful control of fluid admin
• Older children may receive IV fluids through a 60 drop/mL gravity infusion set
• Remove all air bubbles (risk of PFO) from IV tubing & injection ports
Emergency Drugs
• All emergency drugs should have 1.5 in. 22 gauge needle for emergency IM injection
ANESTHESIA TECHNIQUES
Induction

Maintenance
• Volatile agents or TIVA-based techniques can be used
• Drug selection guided by coexistent dz & surgery duration
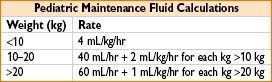
• “4–2–1 rule” can guide fluid replacement
• Neonates & infants require additional care to avoid fluid overload (metered devices) & provide glucose supplementation (D5NS)
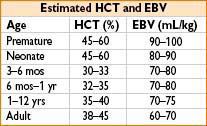
• EBV should always be calculated to guide fluid when surgery has high EBL
• While children tolerate lower Hcts, they also have ↑ metabolic rates & O2 needs
CLINICAL CONDITIONS
Respiratory
Apnea of Prematurity
• Newborns <34 wks’ gestational age → inc risk for perioperative resp complications
• Immature response to hypoxia & hypercarbia → central apnea
• GA may exacerbate; regional may ↓ incidence of postop spells (does not eliminate); other contributing factors include hypoglycemia, hypothermia, anemia
• Therapies: Positioning (avoid mechanical airway obstruction), resp stimulants (methylxanthine/caffeine 10 mg/kg) in high-risk pts, appropriate monitoring
• Usually premature newborns <60 wks’ postconception → need continuous cardiorespiratory monitoring for 24 hrs postop (no outpatient procedures)
Prematurity—Perioperative Concerns
• ↑ risk of hypothermia
• Unable to regulate glucose control
• ↑ risk of postop apnea (esp if <50 wks’ postconceptual age)
• Retinopathy of prematurity (esp if. <44 wks’ postconceptual age)
• Pulmonary dysfunction
Meconium Aspiration
• Presence of thick, meconium-stained amniotic fluid during concerning aspiration → may result in profound resp distress & hypoxemia
• Suction nares & oral cavity immediately after delivery
• Transfer newborn to a radiant warmer & intubate
• Apply suction & withdraw ETT; repeated until only trace meconium seen
• PPV should not be used initially
• Can spread meconium distally into bronchial tree
• If bradycardia/cyanosis develop → gentle PPV with 100% O2 pressure
Bronchopulmonary Dysplasia (BPD)
• Lung dz of newborn; problematic to accurately define as presentation has varied
• Initially described lung injury from aggressive mech ventilation & high FiO2
• Develop smooth muscle hypertrophy, airway inflammation, pulm HTN
• Exogenous surfactant, steroids, & gentler vent modes → improved survival (overall dz incidence has not decreased)
• Babies <30 wks’ gestational age →
• Present with immature lung parenchyma & dysfunctional alveoli
• Pulm dysfx will be persistent to varying degrees (may affect later management)
• Airway hyperreactivity & resp infections common
• Supportive care in the OR → gentle ventilation, limit barotrauma, β2-agonists
• Consider need for postop ICU admission
Congenital Diaphragmatic Hernia (CDH)
• Diaphragmatic defect → presents at birth with cyanosis, resp distress, scaphoid abd
• Get herniation of abd contents → result in lung & pulm vessel hypoplasia
• Not simply lung compression & atelectasis
• Surgical correction → postponed several days to optimize pt cardiopulmonary status
• Severe defects often require more support (ECMO or nitric oxide)
• Anesthetic management
• Intubation (awake, inhalation, or RSI) should minimize gastric distention
• Maintenance usually volatile + narcotic (avoid N2O → risk of pneumothorax)
• A-line + CVP for blood sampling/fluid resuscitation; temp maintenance important
• Maintain low pulm vascular resistance → avoid hypoxia & hypercarbia
• Contralateral pneumothorax → sudden cardiovascular collapse & ↓ lung compliance
• Postop: Transfer to NICU intubated & paralyzed
Asthma
• Triad of airway inflammation, reversible flow defects, airway hyperreactivity
• Signs & symptoms: Wheezing, dyspnea, chest tightness, coughing
• Preop interview: Freq of episodes, current meds, hospital admissions, steroid use
• Severe bronchospasm → can restrict airflow so much that wheezing disappears
• Anesthetic management: Supplemental O2, bronchodilators, anticholinergics
• Epinephrine may be required to treat severe episodes of bronchospasm
• Avoid ETT use (may precipitate bronchospasm) for noninvasive procedures
Upper Respiratory Tract Infections (URIs)
• Children have ≈6–8 URIs/yr; most caused by rhinovirus
• Croup, influenza, strep pharyngitis & allergic rhinitis → may mimic URIs
• URIs ↑ airway reactivity for 4–6 wks following onset of symptoms
• Potential complications from GA → laryngospasm, bronchospasm, & desat
• Risk factors for resp events: Hx of prematurity, coexistent reactive airway dz, 2nd-hand smoke exposure, ETT, nasal congestion/secretions, airway surgery
• Not practical to cancel all children with recent URI; reschedule elective surgery if:
• Purulent nasal discharge, productive cough, fever >100°F
• No change in functional status (appetite, activity), likely to tolerate brief proc
• LMA acceptable technique to avoid unnecessary airway manipulation
• Consider deep extubations (spontaneously breathing under ≥2 MAC of sevo) to minimize airway irritation during emergence
Secondary Smoke Exposure
• 2nd-hand smoke leads to inc risk of adverse resp events under GA → laryngo-/bronchospasm, breath holding, airway obstruction, ↑ oral secretions
Cardiac
Patent Foramen Ovale (PFO)
• Intracardiac shunt → permits fetal circulation in utero (interatrial communication)
• Usually closes during delivery, soon after infant’s 1st breath
• Pulm vascular resistance falls & L atrial pressures exceed R → closes flap
• Conditions which ↑ R-sided atrial pressures may reopen this conduit → hypoxia
• Paradoxical air embolism: Can occur in pts with PFO → if precautions are not taken
Atrial & Ventricular Septal Defects (ASD/VSD)
• ASD & VSD → result left-to-right shunts, do not present with systemic hypoxemia unless defects large & volume overload severe
• Small defects usually asymptomatic & hemodynamically stable
• Over time, shunt flow may → lead to R-heart volume overload & CHF
• Corrective procedures usually timed according to disease severity
• Anesthetic management
• Avoid hypoxia & hypercarbia (increased pulm vascular resistance)
• Conditions which ↑ R-sided heart pressure above L-side may provoke shunt reversal & critical hypoxemia
Neurologic
Duchenne Muscular Dystrophy
Associated with malignant hyperthermia, trigger-free anesthetic techniques should be employed
Metabolic
Mitochondrial Disease (MD)
• Diverse group of enzyme complex defects that adversely affect energy metabolism
• Incidence 1:5,000 with variable age of onset & presentation
• Abnl ATP production affects brain, heart, & muscle; can lead to:
Seizures, spasticity & developmental delay, hypotonia, cardiomyopathy, arrhythmias, chronic GI dysmotility, delayed growth
• No proven assoc between MD & malignant hyperthermia
• Pts may be sensitive to propofol, but no clear guidelines regarding its use
• Be aware of potential for metabolic acidosis
• Normal saline generally recommended for maintenance fluids
• Lactate admin may cause worsening of symptoms
• Fluid requirements may be elevated
• Children may also require glucose supplementation & serial monitoring
Gastrointestinal
Pyloric Stenosis
• Obstruction of pyloric lumen usually age 5 wks → persistent, bile-free projectile vomiting
• Condition = medical (not surgical) emergency
• Infant may be severely dehydrated & have concurrent electrolyte abnl
• Emesis is H+ ion rich, causes hypokalemic, hypochloremic metabolic alkalosis
• Must correct before surgical repair
• ↑ risk for aspiration
• Need gastric decompression (NG) immediately before induction
• Rapid-sequence IV induction with succinylcholine or
• Awake, oral ETT intubation may require help to physically restrain infant
• Procedure = usually brief, long-acting muscle relaxation unnecessary
Tracheoesophageal Fistula (TEF)
• Most common presentation (85%) = Type C (proximal esoph atresia w/distal fistula)
• Symptoms: Coughing, excessive drooling, & cyanotic episodes
• Failure to pass soft-tipped suction catheter into stomach = diagnostic
• Presence of blind esophageal pouch confirmed by x-ray
• Preop assessment: Focused on resp support, aspiration precautions, & identification of other congenital abnl (echo to rule out endocardial cushion defects)
• Anesthesia management: A-line usually placed
• Position pt on 30° wedge to avoid passive aspiration of gastric fluid
• Induction techniques: Should minimize aspiration risk (awake intubation, RSI)
• Avoid PPV prior to intubation
• May cause significant gastric distention, diaphragmatic elevation, & hypoxia
• Prophylactic gastrostomy may prevent accumulation of gastric air
• Deliberate R-sided mainstem intubation → limit transmission of air across fistula
• Pass ETT distal to fistula, then withdraw until bilateral breath sounds obtained
• Lung isolation indirectly achieved by surgical compression of nondependent lung
• May be poorly tolerated (V./Q. mismatch); consider intermittent lung reinflation
• Hypotension may occur → mediastinal structures distortion & ↓ venous return
• Extubate stable pts (with good pain control) to avoid pressure on tracheal suture line
• If pt remains intubated, only suction with a premeasured catheter that does not extend beyond distal tip of ETT
Gastroschisis & Omphalocele
• Involve defects of anterior abdominal wall with herniation of visceral components
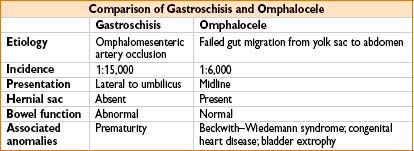
• Cover exposed viscera to avoid evaporative heat loss & limit infection
• Large fluid shifts occur; fluids should be aggressively replaced
• Serial electrolyte & glucose monitoring important (place A-line/CVP)
• Anesthetic technique
• Awake intubation or RSI; avoid N2O
• Defect closure may → ↑ intra-abdominal pressures which may cause → ↑ peak airway press, ↓ venous return, hypotension, lower extremity ischemia
• Postop: Usually require mech vent support
Necrotizing Enterocolitis
• Etiology multifactorial: Pts usually present with bowel distention & bloody feces
• Preterm infants <2 wks’ gestational age → highest risk
• Intestinal hypoperfusion & ischemia → weakened intestinal wall → may perforate
• Anesthesia management: Place A-line & CVP
• Resuscitation should include crystalloid & blood products
• Monitor urine output, avoid N2O
• DIC, thrombocytopenia may occur
• Pts often return for reexploration
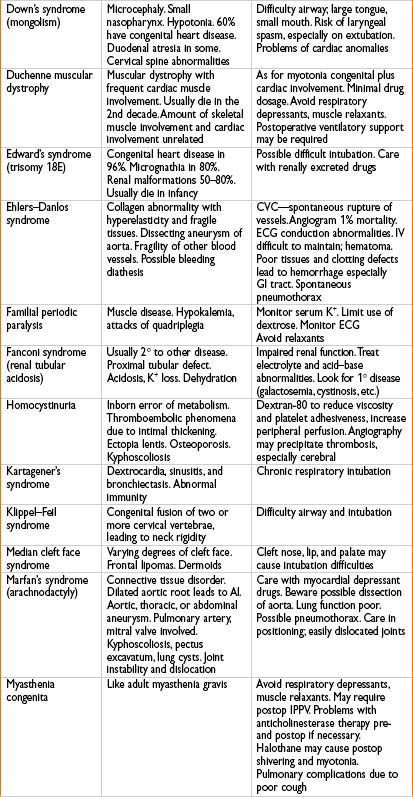
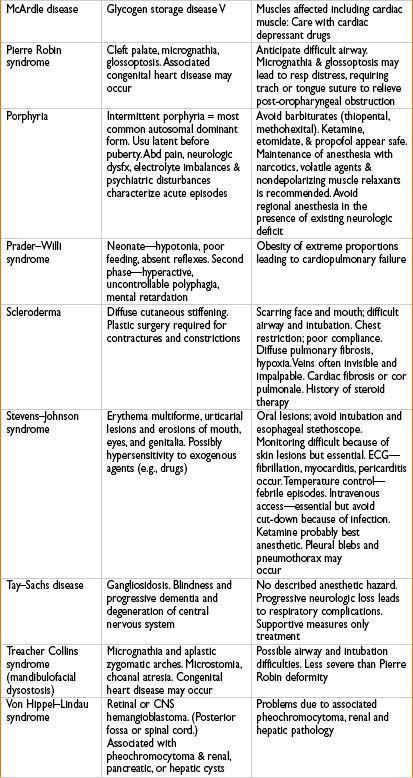
Pediatric Congenital Syndromes


NEONATAL & PEDIATRIC RESUSCITATION
Figure 26-2. Neonatal resuscitation algorithm.

Neonatal Resuscitation Algorithm
Note: The following summary is not to be a substitute for completion of the Neonatal Resuscitation course as administered by a certified instructor.
• ∼10% of newborns require direct assistance to achieve cardiopulmonary stability during transition to extrauterine life. <1% require extensive efforts
• Term neonates with adequate breathing/crying and tone should be dried and kept warm. All others require rapid assessment and the following sequential interventions
• Dry and keep warm, position, airway check, stimulate to breathe
• Ambu-bag ventilation, oximetry monitoring, possible intubation
• Chest compressions
• Medications and volume expansion
New recommendations since 2010:
• Initial evaluation now followed by simultaneous assessment of heart and respirations. Oximetry monitoring should be used early
• For full-term babies, resuscitation should begin with air rather than 100% FiO2
• Supplemental oxygen should be blended with air and delivered concentration guided by oximetry
• Current evidence neither supports nor contradicts the routine endotracheal suctioning of infants born in the presence of meconium-stained amniotic fluid
• Neonatal chest compression–ventilation ratio should remain 3:1, higher ratio to be applied if neonatal arrest due to cardiac etiology
• Therapeutic hypothermia may be considered for term/near-term infants with evolving hypoxic-ischemic encephalopathy
• It is appropriate to consider cessation of resuscitation efforts if no detectable heart rate for 10 min
• Delay cord clamping for at least 1 min in babies NOT requiring resuscitation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








