Sacral cornu (S5)
• Thoracic spinous processes—angled caudally (in relation to vertebral bodies)
• Lumbar spinous processes—angled horizontally
• “S-shape of spinal column”: Thoracic kyphosis (convex) at T4; lumbar lordosis (concave) at L3
• Midline approach—order of tissues encountered: Skin → subcutaneous tissue → supraspinous & interspinous ligaments → ligamentum flavum → epidural space → dura mater → subdural space → arachnoid mater → subarachnoid space (= intrathecal space) containing CSF
• Paramedian approach (needle insertion 1–2 cm lateral to midline): Bypasses supraspinous & interspinous ligaments and spinous processes; consider for narrowed intervertebral spaces, calcified ligaments, thoracic epidural (sharply angled, overlapping spinous processes, narrowed intervertebral spaces)
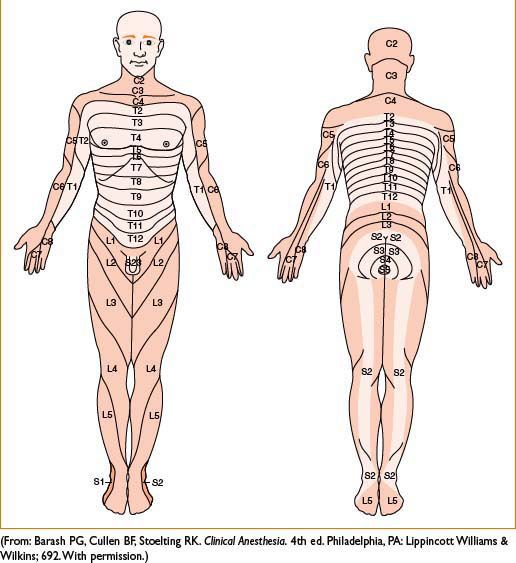
Figure 6-1. Dermatome map.
Physiologic Effects
• Neurologic: Order of nerve blockade
Small sympathetic C fibers → small sensory (Aδ) fibers (pain & temp) → large sensory (Aβ) fibers (proprioception & touch) → large motor fibers (Aα)
Blockade of preganglionic sympathetic fibers exceeds sensory block (spinal > epidural), often by up to two dermatomes, with degree of blockade determined by block height
• Cardiovascular
Sympathectomy (spinal > epidural) → loss of vascular tone → hypotension & reflex tachycardia (occasionally upper body vasoconstrictor with baroreceptor activation can cause paradoxical bradycardia)
Supra-T4 levels block cardioaccelerator fibers (T1–T4) → paradoxical bradycardia → decreased CO & further hypotension
Large volumes of local anesthetic used for epidurals → higher systemic absorption → direct cardiac depressant effects
• Pulmonary
Impaired cough reflex, high blockade ↓ use of accessory resp. muscles (intercostals, abdominals) → use caution in pts with limited pulmonary reserve
Unchanged: Inspi fx (unless respiratory centers [C3–C5] blocked), TV, MV, Vd
PFT changes: ↓ or unchanged VC, ↓ ERV, ↓ expiratory flow rate
• GI
Sympathectomy → hyperperistalsis (unopposed parasympathetics) → N/V (prevented by tx of hypotension [fluids, vasoconstrictors], atropine if high thoracic block)
• GU
Sacral blockade → atonic bladder (consider catheterization); renal blood flow usually maintained
• Neuroendocrine
Avoid surgical stress response (incr. catecholamines, vasopressin, GH, renin, angiotensin, cortisol, glucose, ADH, TSH) with adequate sensory blockade, nearly complete w surgery below umbilicus (possible cardioprotective effect of thoracic epidural/analg. in pts with cardiovasc/cardiac disease)
Contraindications to Placing a Neuraxial Block
• Absolute (per NYSORA)
Patient refusal/infection at site of needle puncture, bleeding diathesis (severe hypovolemia [uncorrected]), ↑ ICP, true allergy to amide and ester LA
• Relative (per NYSORA)
Severe anatomic abnormalities or prior back surgery, uncooperative pt, neurologic disease (multiple sclerosis), infection distal to needle insertion site, and bacteremia (consider with prior antibiotic prophylaxis), severe cardiac disease (aortic/mitral stenosis), abnormal coagulation (endogenous or iatrogenic), anesthetized pt (cervical, thoracic)
Patient Positioning for Block Placement
• Goal for optimal positioning: Widen intervertebral spaces
→ Knees flexed toward abdomen, chin flexed to chest, shoulders relaxed
• Sitting position—easier to identify midline, can create saddle block if using hyperbaric solutions
• Lateral decubitus position—use if patient unable to sit
→ Can preferentially block 1 side (if using hypo- or hyperbaric solutions)
• Prone jackknife position—good for perirectal surgery (if using hypobaric solution)
Complications of Neuraxial Anesthesia
Common to both spinal and epidural anesthesia
• Backache
• Pruritus
• Hypotension
• Urinary retention
• Nerve injury
• Infection
• Hematoma
• Hypoventilation
Other spinal complications
• Transient neurologic symptoms (TNS)—more common with ambulatory procedures, lithotomy position, lidocaine spinals. Symptoms: Delayed onset of pain and/or dysaesthesia in lower back, buttocks, posterior thighs (can last up to 7 d)
• Cauda equina syndrome—occurs with repeated admin of conc. local anesthetic. Symptoms: Bowel/bladder dysfunction and/or neurologic impairment; seek immediate neurosurgical consult
• Postspinal headache—(see postdural puncture headache later)
• High/total spinal—supracervical blockade can cause cardiovascular collapse, apnea, loss of consciousness; supportive treatment/intubation may be necessary
Other epidural complications
• Postdural puncture headache (PDPH)—from inadvertent dural puncture (wet tap); usually self-limited (<7 d). Initial management: Hydration, caffeine (500 mg), NSAIDs, abdominal binders. Persistent or intolerable PDPH (>24 hrs): Epidural blood patches >90% effective
• Spinal cord injury—can occur if wet tap occurs at level above where spinal cord ends
• Local anesthetic toxicity—dizziness, tinnitus, CNS excitation, seizures, cardiac arrest can occur from systemic absorption or intravascular injection of local anesthetic. Treatment is supportive. Consider 20% intralipid emulsions for refractory cardiac arrest
SPINAL ANESTHESIA
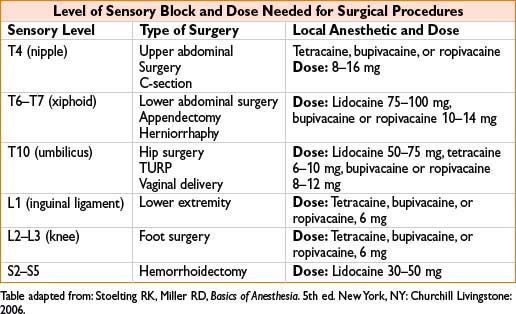
• Rapid & reliable onset of lower body anesthesia by injecting local anesthetic into the intrathecal space
• Blocks spinal cord fibers and nerve rootlets
• Usually single-shot, although continuous catheters can be used
• Consider prior intravascular volume loading (500–1000 mL fluid) to reduce effects of rapid sympathectomy
• Needles:
• Small gauge (>24 G), pencil point needles (Sprotte, Whitacre) reduce risk of PDPH
→ Often require introducer (19 G) to penetrate superficial tissues
• Large gauge (<22 G), cutting (Quincke, Greene) needles
→ Used in difficult spinals to penetrate fibrotic, calcified ligaments
• Introduce needle (midline or paramedian technique) at L2–L5 interspaces until dural “pop” felt or if CSF flows freely when stylet removed
• Taylor approach: Spinal performed at L5–S1 by inserting needle 1 cm medial & caudal to ipsilateral posterior superior iliac spine & directing it cephalomedially toward the midline

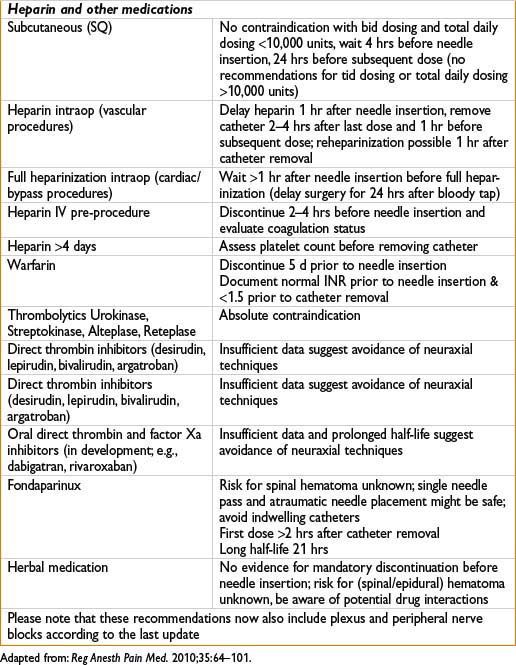
• Duration of spinal anesthesia:
• Dependent on type & dose of local anesthetic used
• Duration can be prolonged with vasoconstrictors (phenylephrine/epinephrine)
Continuous Spinal Anesthesia (CSA)
• “Titratable spinal anesthesia” combining benefit of single-shot spinal (rapid onset) and epidural anesthesia (continuous technique)
(maintain level and duration of block during surgery, titrate effect to pts response)
• Lower doses of LA for continuous technique can be used
• Useful in patients with severe systemic disease (e.g., severe aortic/mitral stenosis)
• Technique same as for single epidural anesthesia with intentional piercing of the dura mater and insertion of epidural catheter into intrathecal space (smaller gauge catheter, usually 22 G used to decrease possibility of PDPH, microcatheters <24 G withdrawn from market)
• Controversy about increased risk of cauda equina syndrome (most reports on combination with microcatheters and use of hypobaric lidocaine)
• After confirmation of intrathecal catheter placement by aspiration of CSF slowly bolus with usual intrathecal dose for spinal anesthesia
• Mark catheter meticulously as spinal catheter to avoid wrong medication dosing
• Continuous management possible with intermittent bolus dosing and titration to effect or low-dose continuous infusion
• Spinal catheters are usually not left in place postoperatively
EPIDURAL ANESTHESIA
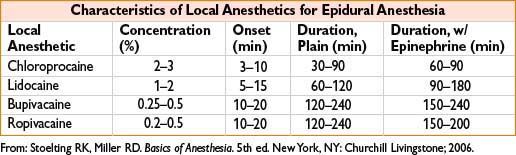
• Slower onset, more controlled segmental spread of anesthesia using larger quantities of medication (roughly 10× more than spinal doses) injected into epidural space
• Usually a continuous catheter technique; can target select dermatomes (unlike spinal)
• Thoracic epidurals → thoracic & upper abdominal surgeries
• Lumbar epidurals → labor analgesia, lower abdominal, pelvic, lower extremity surgeries
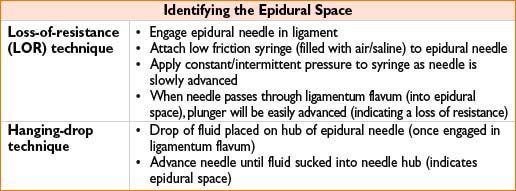
• Catheter placement & epidural space verification:
• Thread epidural catheter 3–5 cm into epidural space
• Aspirate catheter to assess for intravascular/intrathecal insertion (look for blood/CSF)
• Consider epidural test dose (3 mL of 1.5% lidocaine with epinephrine 1:200,000)
→ shows if catheter intrathecal (dense spinal) or intravascular (tachycardia, tinnitus)
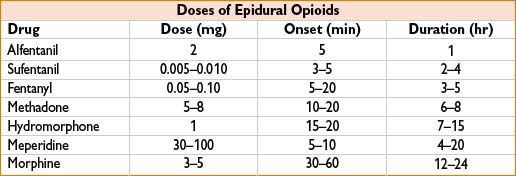
• Medications
• Surgical anesthesia: High local anesthetic conc. (2% lidocaine, 0.5% bupivacaine)
• Postop pain/labor analgesia: Dilute local anesthetic conc. + opioid (0.1% bupivacaine + 0.005% fentanyl)
(combination provides synergy, and reduces side effects [motor block, pruritis])
• Adjuvants can supplement block (clonidine, epinephrine, phenylephrine)
• Factors affecting quality of epidural block
• Volume injected, vasoconstrictors, site of injection, & parturients
• Sodium bicarbonate can hasten block onset (↑ nonionized local → easier neuronal diffusion)
1 mEq for each 10 mL lidocaine/chloroprocaine
0.1 mEq for each 10 mL of bupivacaine (to avoid precipitation)
• Patient position has no effect (unlike spinal anesthesia)
• Management
• Continuous, bolus, or patient controlled epidural analgesia (PCEA) techniques
• Continuous infusion rate depends on pt characteristics & type of solution used (continuous infusions often run at 4–10 mL/hr with a bolus dose every 5–15 min)
• Epidural troubleshooting
• One-sided block—provide medication bolus, pull back or replace catheter
• Patchy block assess for possible subdural block, replace catheter if necessary
• Inability to thread catheter—verify epidural space with LOR, then advance needle 1 mm & retry
• Inability to remove catheter—change pt position (flexing, extending, rotating spine); try carefully again later, NEVER pull using excessive force!
COMBINED SPINAL–EPIDURAL (CSE) TECHNIQUE
• Advantages
• Combines a rapid-onset block (spinal) with ability to provide continuous management (epidural)
• Equipment
• Epidural tray with specifically designed Tuohy needle (has back hole for spinal needle insertion); alternatively, can use regular Tuohy needle with appropriately sized spinal needle
• Dose of spinal medication
• Surgical anesthesia: Normal dose (see table above)
• Labor analgesia: Low-dose opioid + local anesthetic (fentanyl 25 mcg + bupivacaine 2.5 mg)
• Technique
• Proceed as if placing an epidural
• Place spinal needle through epidural needle past dura (once epidural space identified)
• Once CSF is obtained, inject medication, remove spinal needle, & thread epidural catheter
• Disadvantages
• Inability to test dose epidural catheter (no reassurance if epidural will work after spinal wears off)
• Slightly ↑ incidence of pruritus, respiratory depression, or transient fetal bradycardia
CAUDAL ANESTHESIA
• Epidural anesthesia performed at sacral level close to where dural sac ends
• Indications
• Commonly used in children for low superficial abdominal, perineal, or sacral anesthesia
• Can be used for 2nd stage of labor, perineal, or sacral anesthesia in adults
• More difficult in adults due to obscure anatomic landmarks
• Anatomy
• Sacral hiatus—posterior opening to sacral canal at S5 level (entrance identified by sacral cornua). Sacral hiatus can also be identified as third point of an equilateral triangle using posterior superior iliac spines (PSIS) as the two other points
• Sacrococcygeal membrane—equivalent of ligamentum flavum (overlies entrance to sacral hiatus, can calcify in adults)
• Positioning: Lateral or prone
• Technique
• Insert needle between sacral cornu at 45-degree angle until slight ↓ in resistance encountered (signifying penetration of sacrococcygeal membrane)
• Redirect needle parallel to sacrum & insert another 1–1.5 cm
• Syringe should be aspirated for CSF/blood & test dose should be given
• Catheter may be threaded (similar to an epidural)
• Medications
• Pediatric dose: 0.5–1 mL/kg of 0.125–0.25% bupivacaine +/- epinephrine
• Adult dose: 15–20 mL of local anesthetic
• Complications: Similar to those for epidural anesthesia
PERIPHERAL NERVE BLOCKS
Introduction
• Peripheral nerve blocks rely on local anesthetics injected around specific nerves/nerve bundles to prevent sensory transmission back to spinal cord/CNS
• Uses include surgical anesthesia +/- general anesthesia, postoperative analgesia or acute/chronic pain management
Preparation and Materials
1. Standard patient monitors (SpO2, ECG, blood pressure cuff)
2. Sedative medications & oxygen
3. Sterile tray and gloves
4. Block needle—short, B-bevel (blunt), beaded-tip, or insulated needle
5. Infusion catheter and appropriately sized block needle (if performing continuous nerve block)
6. Local anesthetic (LA)
7. Method of nerve localization (i.e., nerve stimulator, ultrasound machine, etc.)
8. Emergency airway equipment and intubation medications

• Contraindications—similar to those for neuraxial blockade
• Complications common to all nerve blocks:
• Nerve injury, local anesthetic toxicity, infection, hematomas
• Sterile technique should be used for any block to reduce risk of infection
• Aspirate from syringe every 5–10 mL for blood/CSF to avoid intravascular/intrathecal injection of local anesthetic
Ultrasound Basics
• Ultrasound (US) imaging based on transducer emitting sound waves into tissue and receiving sound reflected or scattered back to receiver
• Ultrasound-waves are high-frequency sound waves above 20 kHz
• Frequencies useful in regional anesthesia are in the 4–17 MHz range
• Tissues with different acoustic impedance interact with incident sound waves, causing attenuation, reflection, refraction, and scattering
• The greater the echogenicity of tissue, the brighter it is on sonogram
• Structures with high water content (e.g., blood vessels) appear hypoechoic (dark or black) because the ultrasound waves are transmitted through these structures easily with little reflection
• Structures with low water content (e.g., bone, tendons) appear hyperechoic (bright) because transmission of ultrasound waves is blocked, and the strong signal returned to transducer gives these structures a white appearance
• Structures of intermediate density and acoustic impedance appear gray on the screen and are called isoechoic
Transducer selection
• Frequency determines the depth of tissue penetration
• Deep structures (>4 cm) require low-frequency transducers (3–7 MHz range): Good penetration, lower axial resolution
• Superficial structures (0.5–4 cm) require high-frequency transducers (10–15 MHz range); decreased penetration, high axial resolution
Imaging Plane
• Short axis (transverse/axial): Cylindrical structures are depicted in cross-section, producing a circular image
• Long-axis imaging: Shows object longitudinally, depicts course of cylindrical objects as linear (limited use in ultrasound-guided regional anesthesia but can help confirm catheter placement for continuous nerve block techniques along a selected nerve)
• In-plane (IP) technique (most commonly used): Needle introduced within plane of imaging shows needle as echogenic line. Only portion of needle within this very thin scan plane can be seen; possibility to advance needle further than intended when tip strays from scan plane
• Out-of-plane (OOP) technique: Needle is introduced from outside plane of imaging and crosses scan plane, needle tip or shaft shown as echogenic dot
• Oblique-plane technique: Object viewed in short axis, needle introduced within plane of imaging
Sonographic Appearance of Nerves
• Nerve fascicles appear hypoechoic, surrounded by hyperechoic epineurium (honeycomb appearance in short axis)
• Nerves change shape and echotexture along their course (e.g., proximal nerves, such as roots and trunks of brachial plexus, appear hypoechoic monofascicular but become hyperechoic and polyfascicular in periphery)
• Can appear round, oval, or triangular and may mimic other structures (e.g., vessels, tendons, fascia, muscle)
General Considerations for Quality Improvement and Safety
• Adequate knowledge of anatomy and equipment
• Avoid air trapping between the transducer and the sterile cover; will result in shadowing due to poor impedance of air for US waves
• Patient positioning and monitoring as for conventional block techniques
• Surface anatomy landmarks used in conventional, non–image-guided techniques can be used to guide initial placement of US transducer; further adjustments made according to US image
• Avoid close proximity to bones (e.g., clavicle) since this can produce artifacts and compromise image quality
• Advance needle only under real-time imaging and never if tip is not visualized
• Nerve stimulation can confirm needle position but does not appear to improve block success rate
• Injection of the LA should be made incrementally, often in multiple sites, with continuous assessment of LA distribution
• Circumferential spread around nerves produces rapid and complete conduction block
• Injections should be made slowly with frequent aspiration and maintenance of low injection pressures (<20 psi) to avoid intravascular and intraneural injections
• If LA distribution cannot be visualized after test dose of 1–2 mL injection should be stopped. Aspirate and reassess needle tip placement to rule out intravascular injection
• Remove air bubbles from syringe or tubing; air is highly echogenic and can markedly degrade image quality after inadvertent injection
• Bicarbonate-containing solutions also may obscure imaging because of their carbon dioxide content
SUPERFICIAL AND DEEP CERVICAL PLEXUS BLOCKS
• Anatomy
• C1–C4 ventral rami (which divide into superficial & deep branches)
• Superficial branch → four main nerves (provides cutaneous sensation of neck from jaw line to T2)
• Deep branch → ansa cervicalis = loop formed by C1–C3 nerves (provide sensory & motor function to deeper structures of neck, including phrenic nerve, strap, & prevertebral muscles)
• Indications
• Neck surgery including lymph node dissection, tracheostomy, carotid endarterectomy, thyroid surgery
• Superficial cervical plexus block
• Insert block needle at midpoint of posterior border of sternocleidomastoid
• Inject 15–20 mL local anesthetic in a fan-like manner in cranial & caudal direction
• Complications: Trapezius muscle paralysis can occur from blockade of CN XI
• Deep cervical plexus block
• Draw a line from mastoid process to transverse process of C6 (Chassaignac’s tubercle)
• Draw a second parallel line that is 1 cm inferior to it & mark off points that are 2, 4, & 6 cm from mastoid process, which correspond to C2, C3, & C4 transverse processes
• At each point insert block needle at a slightly caudal angle until transverse process is met
• Withdraw needle slightly once bone is contacted and inject 5 mL; repeat at other levels
• Alternatively, can make one injection at C4 with caudal pressure held to facilitate cephalad spread
• Complications/side effects: Horner’s syndrome, phrenic & superior laryngeal nerve block, seizure, intrathecal/epidural/intravascular injection (e.g., vertebral artery)
INTERCOSTAL NERVE BLOCKS
• Anatomy
• Intercostal nerves arise from ventral rami of T1–T11
• Each nerve sends off 5 branches, including gray and white communicantes, dorsal, lateral, and anterior cutaneous branches
• Nerves run along inferior aspect of ribs in groove with intercostal artery & vein (from superior to inferior intercostal vein, artery, nerve)
• Anterior & lateral cutaneous branches readily blocked at posterior angle of rib just lateral to sacrospinalis muscle group
• Block can be performed at midaxillary line (may miss lateral cutaneous branch)
• Indications
• Does not provide adequate anesthesia for surgery (except for very superficial chest wall procedures)
• Provides supplementary analgesia for rib fractures, thoracic procedures, mastectomy, upper abdominal procedures
• Technique
• Positioning: Prone, sitting, or lateral decubitus
• Palpate inferior edge of rib to be blocked at its posterior angle (6–8 cm lateral to midline)
• Insert needle at angle 20° cephalad until needle contacts inferior portion of rib
• Redirect slightly until needle slides underneath rib
• Advance needle another 3 mm (a fascial pop can sometimes be felt)
• After negative aspiration, inject 3–5 mL of local anesthetic
• Complications
• Pneumothorax—patients with limited pulmonary reserve are a relative contraindication
• Local anesthetic toxicity—risk greatly rises as number of levels blocked increases
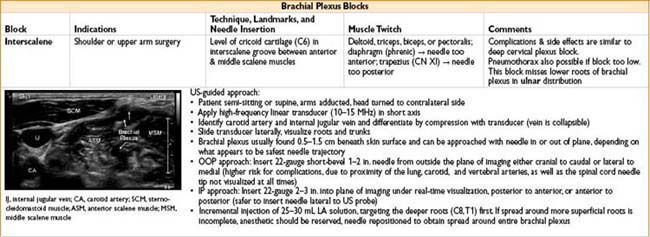
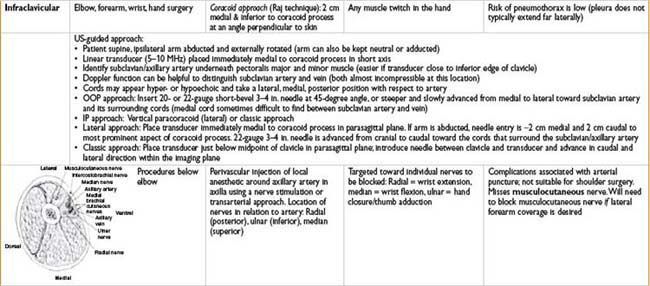
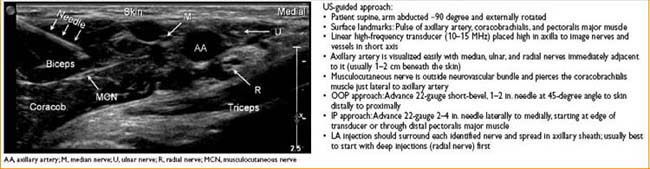
BRACHIAL PLEXUS BLOCKS
• Brachial plexus: Nerve roots from C5–T1: Trunks → Divisions → Cords → Branches
Brachial plexus
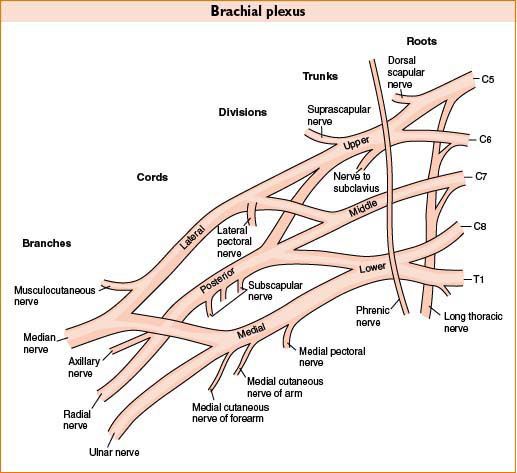
• Can block brachial plexus by injecting 25–40 mL of local anesthetic in certain areas along its path (see table below, Brachial Plexus Blocks)
• Can also perform individual nerve blocks for selective blockade or as rescue blocks (inject 3–5 mL local anesthetic)
• Radial
• Elbow: Needle inserted lateral to biceps tendon until it makes contact with lateral epicondyle, withdraw ∼0.5 cm before injecting LA
• Wrist: Local anesthetic injected in ring subcutaneously starting from radial artery pulsation anteriorly to extensor carpi radialis posteriorly at level of radial styloid as well as injection of 2–3 mL LA lateral to radial artery
• Muscle twitch/innervation: Extensor muscles of forearm → wrist extension
• Median
• Elbow: Needle inserted medial to brachial artery pulsation 1–2 cm proximal to elbow crease
• Wrist: Needle inserted between palmaris longus & flexor carpi radialis tendon until piercing the deep fascia
• Muscle twitch/innervation: Forearm flexors, 1st/2nd hand lumbricals and thenar eminence → wrist flexion, thumb opposition
• Ulnar
• Elbow: Needle inserted in ulnar groove just proximal to medial epicondyle; slightly withdraw before injecting
• Wrist: Needle inserted between flexor carpi ulnaris tendon & ulnar artery at level of styloid process
• Muscle twitch/innervation: Majority intrinsic hand muscles → hand flexion
• Musculocutaneous
• Inject local anesthetic into substance of coracobrachialis
• Muscle twitch/innervation: Coracobrachialis, brachialis and biceps brachii → elbow flexion/supination
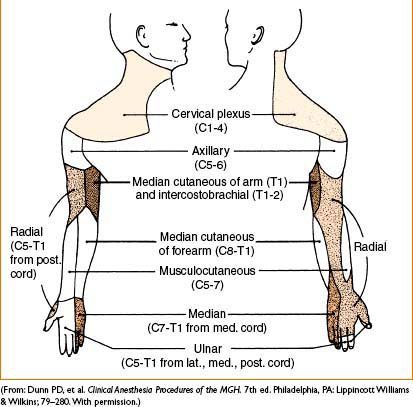
Figure 6-2. Cutaneous innervation of the upper extremity.

DIGITAL NERVE BLOCK (UPPER EXTREMITY)
• Anatomy: median & ulnar nerves → common digital nerves (located on bilateral ventrolateral aspect of each finger)
• Indications: Finger surgery (e.g., trauma, distal amputation)
• Two techniques:
1. Block of volar & dorsal digital nerves
→ Pronate hand, insert needle at dorsolateral aspect of base of finger
→ Aim anteriorly toward base of phalanx
→ Advance until contact made with phalanx
→ Withdraw needle from bone contact
→ Aspirate, then inject 2–3 mL of local (plain)
→ Repeat on each side of base of finger
2. Transthecal digital block
→ Supinate hand
→ Insert needle at 45-degree angle into flexor tendon sheath, at level of distal palmar crease
→ Aspirate, then inject 2–3 mL of local (plain) while applying proximal pressure
• Local anesthetics: Any plain local anesthetic (no epinephrine)
• Complications: Intravascular injection, hematoma, digit ischemia, nerve injury, infection
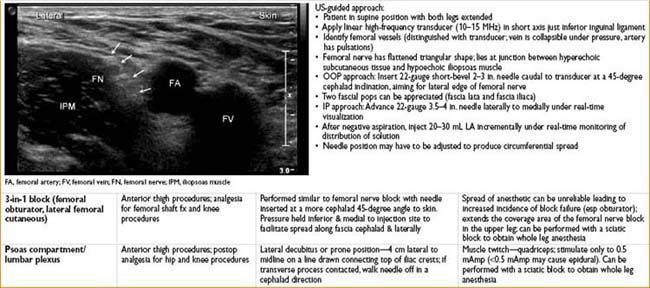
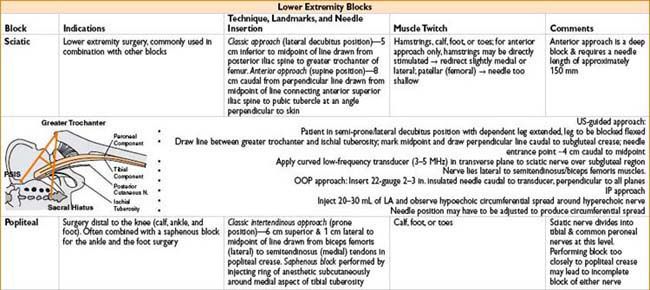
LOWER EXTREMITY BLOCKS
• Lower extremity innervated by lumbar (L1–L4) & sacral plexuses (L4–S3)
• Lumbar plexus: Gives rise to the iliohypogastric, ilioinguinal, genitofemoral, femoral, obturator, & lateral femoral cutaneous nerves
• With the exception of the femoral nerve, individual nerve blocks are commonly performed by infiltration without nerve stimulation
• The psoas compartment/lumbar plexus block achieves blockade of the entire lumbar plexus. Complications from block can include epidural, subdural, or intrathecal injection, retroperitoneal hematoma, and/or visceral injury
• The 3-in-1 block relies on spread of a large volume of local anesthetic (30–40 mL) to achieve blockade of the femoral, obturator, and lateral femoral cutaneous nerves
• Sacral plexus: Gives rise to sciatic nerve
• Sciatic nerve divides into tibial & common peroneal nerve at popliteal fossa
• Tibial nerve gives rise to posterior tibial nerve & contributes to sural nerve
• Common peroneal divides deep into the superficial & deep peroneal nerves, contributes to sural nerve
• Combination blocks
• The 3-in-1 + sciatic or lumbar plexus + sciatic blocks can provide anesthesia to essentially the entire lower extremity (3-in-1 + sciatic may miss the most proximal and medial portion of the upper leg)
• The knee joint is innervated by multiple nerves (femoral [anterior], obturator [medial], lat femoral cutaneous [lateral], and sciatic [posterior]) → a combination block would be needed to provide complete anesthesia for surgery
• Advantages over neuraxial blockade: unilateral limb anesthesia, ↓ risk of sympathectomy (hypotension, urinary retention), & avoidance of neuraxial hematomas in pts on anticoagulation
• Disadvantage: Since anesthesia to the entire lower extremity usually requires >1 block, neuraxial anesthesia is a practical alternative
Lower Extremity Blocks
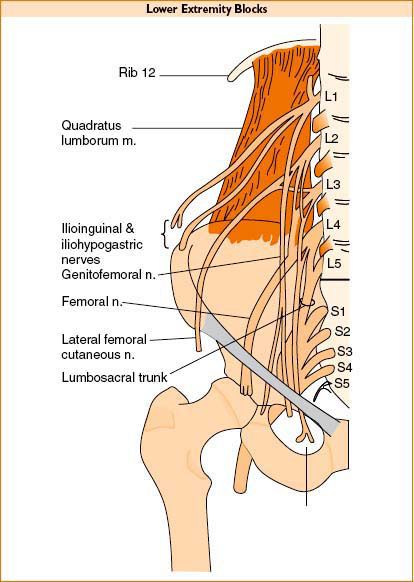
Figure 6-3. Cutaneous innervation of the lower extremity.



TRANSVERSE ABDOMINIS PLAIN BLOCK (TAP-BLOCK)
Anatomy
• Innervation of anterior abdominal wall from spinal nerves T7–L1 (including intercostal nerves T7–11, subcostal nerve T12 and iliohypogastric and ilioinguinal nerves L1)
• Anterior divisions of T7–11 enter abdominal wall between internal oblique and transversus abdominis muscle, supply and perforate rectus abdominis and end as anterior cutaneous branches; give of the lateral cutaneous branches halfway in their course which further divide into anterior and posterior branches that supply the external oblique as well as latissimus dorsi muscle
• Anterior branch of T12 communicates with the iliohypogastric nerve; its lateral cutaneous branch perforates internal and external oblique muscles, descends over iliac crest and supplies sensation to front part of gluteal region
• The iliohypogastric nerve (L1) divides between the internal oblique and transversus abdominis near the iliac crest into lateral and anterior cutaneous branches, the former supplying part of the skin of the gluteal region while the latter supplies the hypogastric region
• The ilioinguinal nerve (L1) communicates with the iliohypogastric nerve between the internal oblique & transversus abdominis near the anterior part of the iliac crest. It supplies the upper & medial part of the thigh & part of the skin covering the genitalia
Indications
• Abdominal field block for treatment of acute and chronic pain
• Lower abdominal surgery including appendectomy, hernia repair, caesarean section, abdominal hysterectomy, and prostatectomy. Efficacy in laparoscopic surgery has also been demonstrated
• Bilateral blocks can be used for midline incisions or laparoscopic surgery (do not exceed recommended safe doses of LA)
• Technically unchallenging but performed with blind end points making the success unpredictable
• US guided TAP blocks have been described to better localize structures and deposit LA with improved accuracy
• Controversy in literature regarding spread and level of block achieved with a single TAP injection esp. cephalad to T10
• It is reasonable to expect a good analgesic effect in the region between T10 and L1 following a single posterior injection. Augmentation with a subcostal injection will help attain a higher block up to T7
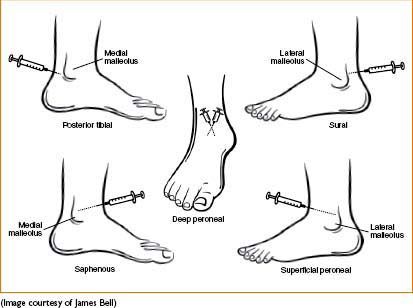
Figure 6-4. Innervation of the foot/ankle for ankle block.
Technique
• Goal: Deposit LA in plane between the internal oblique and transversus abdominis muscles targeting spinal nerves in this plane (conduction block of innervation to abdominal skin, muscles, and parietal peritoneum)
Conventional
• Point of entry is the lumbar triangle of Petit between the lower costal margin and the iliac crest (borders: Anteriorly external oblique, posteriorly latissimus dorsi muscle, inferiorly iliac crest)
• This technique relies on feeling double pops as the needle traverses the external oblique and internal oblique muscles. A blunt needle will make loss of resistance more appreciable
US-guided
• With patient in supine position a high-frequency ultrasound probe (10–5 MHz) is placed in a transverse plane to lateral abdominal wall in midaxillary line, between the lower costal margin and the iliac crest
• IP technique: Advance needle into plane between internal oblique and transverse abdominis muscle. 2 mL saline can be used to confirm needle position after which 20 mL LA is injected
• For prolonged analgesia beyond duration of a single shot of LA, a catheter can be introduced into the transversus abdominis plane
• After opening up the plane with 2 mL saline, catheter is introduced around 3 cm beyond the needle tip; position verified by injecting LA bolus (20 mL); infusion of dilute LA is started at a rate of 7–10 mL/hr
• Subcostal TAP is modification of original technique in which US probe is placed just beneath and parallel to costal margin. The needle is introduced from lateral side of rectus muscle in an IP technique and 10 mL LA injected into transversus abdominis plane to extend analgesia provided by posterior TAP block above umbilicus
Complications
• Few reported with blind technique (including intraperitoneal, intrahepatic injection, bowel hematoma and transient femoral nerve palsy, intravascular injections, and local anesthetic toxicity especially with bilateral injections)
• No reported complications to date with US-guided techniques
INTRAVENOUS REGIONAL ANESTHESIA (BIER BLOCK)
• Indications
• Short procedures on extremities less than 1–1.5 hrs (e.g., carpal tunnel release)
• Materials
• Double tourniquet
• Esmarch bandage
• Small (22–24)-gauge IV in arm to be blocked (to be removed following the block)
• Additional IV access on nonoperative arm (for administration of other meds)
• 40–50 mL of plain 0.5% lidocaine
• Technique
• Elevate arm above body & exsanguinate arm (distal → proximal) using an Esmarch bandage
• Inflate proximal cuff 100 mm Hg higher than systolic BP (or roughly 300 mm Hg)
• Remove bandage, inject 40–50 mL of plain 0.5% lidocaine through the small-gauge IV & remove IV
• Encourage surgeons to start operating as soon as possible
• If tourniquet pain occurs, inflate distal cuff & then release proximal cuff; this will provide additional 20–30 min of anesthesia. Inform surgeons of limited time left
• Complications /problems
• Local anesthetic toxicity can occur if tourniquet is faulty/deflated too early
• If surgery finishes in <20 min, keep tourniquet up for another 10 min; alternatively, release & reinflate tourniquet after 10 sec
• Be prepared to conduct a general anesthetic/MAC in the event surgery is prolonged or block insufficient
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








