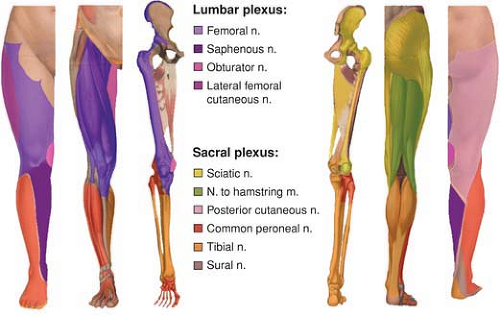
Anatomy of the Lumbar and Sacral Plexus
Laura Clark
Although knowledge of classic anatomic descriptions is essential to perform peripheral nerve blocks, it is important to recognize that variations are frequent and that “normal anatomy” is found in only 50% to 70% of cases.
A. Lumbar Plexus (Fig. 11-1)
Overview
The lumbar plexus is an anastomotic complex formed by the anterior roots from L1 to L3 and the greater part of L4. It has a triangular form, with its base resting against the lumbar vertebrae and veretrebral transverse process and its apex formed by the union of the third roots with the ascendant rami of the fourth. There is frequent anastomosis between the upper part of the plexus with the subcostal nerve and between the L4 rami and the lumbosacral trunk. As with the brachial plexus, we can describe a pre- or a postfixed plexus with respect to the main anastomosis; however, an important characteristic of lumbar plexus anatomy is its great variability and frequent asymmetry. The best definition is given by Bonniot: “The superior limit corresponds to the first roots where the first collateral of the lumbar plexus originate, and the inferior part is defined by the first roots entirely distributed to the sacral plexus” (1922).
In the majority of cases, the fourth roots give rise to fibers for the three main trunks of the lower limb: the femoral, obturator, and sciatic nerves (lumbosacral trunk). This may explain the effectiveness of the posterior approach of the lumbar plexus at the L4 level for hip surgery.
The lumbar plexus lies anterior to the transverse process between the two parts of the psoas muscle. All of the branches of the lumbar plexus emerge from the psoas muscle and all leave the pelvis, though, not all by the same path. Near the vertebral body, the psoas muscle is divided into two planes: a superficial plane that arises from the lateral faces of the vertebral bodies from T12 to L4 and a deep plane arising from the transverse process
of L1 to L5. Within these two planes lie the trunks of the lumbar plexus and the ascending lumbar vein. In addition, the lumbar arteries, which supply the psoas muscle, provide branches for the plexus. The two parts of the muscle then fuse to form the psoas major.
of L1 to L5. Within these two planes lie the trunks of the lumbar plexus and the ascending lumbar vein. In addition, the lumbar arteries, which supply the psoas muscle, provide branches for the plexus. The two parts of the muscle then fuse to form the psoas major.
Besides two small branches—for the quadratus lumborum and the psoas muscles—six branches originate from the lumbar plexus. They are classified either as collateral or terminal branches.
Lumbar Plexus Collateral and Terminal Nerves (Fig. 11-2)
Iliohypogastric Nerve (L1)
The iliohypogastric nerve emerges at the level of the psoas muscle and runs down and laterally along the anterior face of the quadratus lumborum muscle. Close to the iliac crest, it runs between the transversus abdominis and the oblique muscles. It leaves a lateral branch for the anterosuperior part of the buttock, supplying the skin as far as the greater trochanter (55% of cases). Variations are possible, however, including a shorter branch that does not reach the greater trochanter (20%) and a longer branch that extends beyond it (15%). The nerve divides into two branches: an abdominal branch, which supplies the muscles and skin of the inferior part of the abdomen, and an inguinal branch, supplying the skin of the pubis and the scrotum (men) or labium majus (women). The inguinal branch perforates the internal oblique muscle and then runs between the oblique muscles.
Ilioinguinal Nerve (L1)
The ilioinguinal nerve follows the iliohypogastric nerve. Its diameter is inversely proportional to that of the iliohypogastric nerve, and it may be absent in some cases. It gives rise
to an abdominal branch, which is frequently anastomosed with the abdominal branch of the iliohypogastric nerve, and the inguinal branch, which supplies the skin of the superior and medial aspects of the thigh and the genital area. It can replace the genital branch of the genitofemoral nerve and all or part of the lateral femoral cutaneous nerve.
to an abdominal branch, which is frequently anastomosed with the abdominal branch of the iliohypogastric nerve, and the inguinal branch, which supplies the skin of the superior and medial aspects of the thigh and the genital area. It can replace the genital branch of the genitofemoral nerve and all or part of the lateral femoral cutaneous nerve.
Genitofemoral Nerve (L1-2)
This nerve crosses the psoas muscle and extends along its anterior face before dividing into genital and femoral branches. The genital branch passes through the inguinal canal and supplies the cremaster muscle and the skin of the pubis and scrotum (or labium majus). The femoral branch enters the thigh under the inguinal ligament in the femoral sheath and then supplies the skin of the upper part of the femoral triangle. This branch is probably the most variable of the lumbar plexus. It supplies an important part of the anterior aspect of the thigh. In some cases, it receives an anastomosis from T12, and sometimes it is completely absent, in which case it is replaced by the ilioinguinal and the lateral femoral cutaneous nerve.
Lateral Femoral Cutaneous Nerve (L2-3)
After crossing the psoas muscle, the lateral femoral cutaneous nerve follows an oblique and lateral course between the iliac muscle and the fascia iliaca in the direction of the anterosuperior iliac spine. It provides branches for the peritoneum. It then enters the thigh by passing through or under the inguinal ligament and then divides into a posterior branch, which supplies the skin of the superior and lateral aspects of the thigh, and an anterior branch, which supplies the anterolateral part of the thigh as far as the knee. Variations in the course of this nerve are described in 25% of cases, and it may arise directly from the femoral nerve in 18% of cases. Variability also exists with respect to the superficial territories supplied by this nerve. In 31% of cases, this innervation may extend medially as far as the anterior surface of the thigh. This may represent a possible explanation for failure of anesthesia in this region after femoral block in some patients. The lateral femoral cutaneous nerve is considered by some as a branch of the femoral nerve that leaves the femoral nerve after its origin.
As noted previously, these nerves are highly variable in their courses and their extension territory. These variations explain why anesthesia of the anterior face of the thigh is difficult to anticipate both with a femoral block and with a posterior approach. However, it is important to recognize that all of the cutaneous branches of these nerves are mainly subaponeurotic and therefore can be blocked with a subcutaneous injection at the level of the inguinal crease.
Obturator Nerve (L2-4)
The obturator nerve exits the psoas muscle at the level of the sacroiliac joint. It runs outward and downward close to the ureter and the internal iliac artery. Its position in the pelvis, after it leaves the psoas muscle, explains why extension of anesthesia to this nerve after an anterior approach (three-in-one or iliofascial block) is unlikely. It reaches the obturator groove at the upper part of the obturator foramen and then enters the thigh. It then divides into an anterior and a posterior branch. In 50% of cases, this division occurs in the obturator groove, but it may also occur before or after the groove. In the pelvis, it sometimes provides a ramus for the articular capsule of the hip joint. This represents an additional argument for using a posterior lumbar plexus approach for hip surgery.
Anterior Branch
This branch runs in front of the adductor brevis and adductor magnus muscles and behind the adductor longus. It innervates the pectineus, adductor longus, gracilis, and adductor brevis muscles. It typically supplies a limited skin territory at the medial surface of the thigh and the knee. However, there are important variations in the location and extent of this area. The frequent anastomosis of the anterior branch with the saphenous and anterior femoral cutaneous nerves in the adductor canal (the subsartorial plexus) is responsible for significant overlaps. It has been established that an effective block of the obturator nerve is associated with no sensory block in 57% of patients in the presence of a reduction of the adduction motor function. For German anatomists the specific sensitive area of the obturator nerve corresponds to a small posteromedial territory at the distal third of the thigh between the adductor gracilis and the adductor magnus. This explains why the determination of the intensity of an obturator block based only on sensory assessment is difficult in the absence of simultaneous assessment of motor function.
Posterior Branch
This branch runs between the adductor brevis and adductor magnus muscles. It supplies the obturator externus, adductor magnus and adductor brevis muscles, and produces articular branches for the hip and the knee joints.
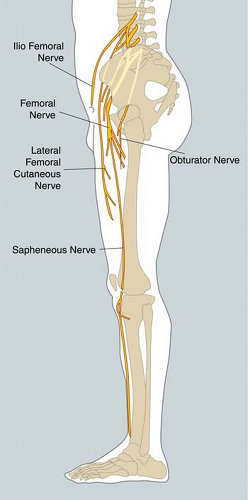
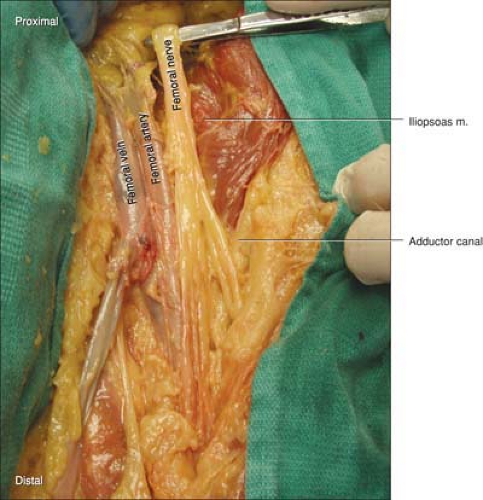
Femoral Nerve (L2-4) (Fig. 11-3)
The femoral nerve is the largest branch of the lumbar plexus. It exits the lateral side of the psoas muscle and runs in the iliopsoas groove toward the inguinal ligament, beneath which it enters the thigh. In the pelvis, it produces branches for the psoas and iliac muscles. Generally, it divides in four terminal branches at the level of or immediately below the inguinal ligament, although in some cases the division occurs before. In the femoral triangle, there are two planes to be considered. The anterior femoral nerve is located within the anterior plane, which innervates the skin over the front and medial sides of the thigh and also contributes to the subsartorial plexus and branches to the sartorius, pectineus, and sometimes part of adductor longus muscles. The posterior plane consists of the quadriceps femoris and the saphenous nerve. The saphenous nerve also contributes to the subsartorial plexus. It supplies the skin of the medial part of the knee and the anteromedial part of the leg as far as the foot, although in some cases it may extend as far as the base of the first toe. Additionally, the saphenous nerve also plays an important role in the innervation of the knee joint.
There are frequent overlaps concerning the cutaneous regions supplied by some branches of the lumbar plexus, especially the lateral femoral cutaneous and the femoral branch of the genitofemoral nerves, which may explain instances of incomplete superficial blocks.
B. Sacral Plexus (Fig. 11-4)
Overview
The sacral plexus is formed by the anterior sacral roots from S1 to S3, and the lumbar roots from L5 are associated with an anastomotic branch from L4 (furcal nerve). The L5 roots and the L4 anastomotic branch form the lumbosacral trunk. The lumbosacral trunk and the sacral roots converge toward the sciatic foramen and merge before entering the buttock. The sacral plexus is shaped like a triangle, with its base lying against the anterior sacral foramina and its vertex corresponding to the anteromedial border of the sciatic foramen. The sacral plexus transverses the sciatic foramen lying anterior to the piriformis muscle and is covered by the pelvic aponeurosis (corresponding to the fascia of the pelvic muscles), which separates it from the visceral structures of the pelvis. In this section only the collateral branches of the sacral plexus for the lower limb are described.
Branches Collateral and Terminal Nerves (Fig. 11-4)
In the buttock, the sacral plexus branches into several nerves supplying the muscles of the region. Some are more relevant for regional anesthesia.
Superior Gluteal Nerve
The superior gluteal nerve leaves the plexus before it crosses the sciatic foramen. It supplies the gluteus medius and gluteus minimus muscles and finishes its course in the tensor fasciae latae muscle. In this regard, it is important to note that it is a branch of the lumbar plexus that provides sensory innervation of the skin over the tensor fasciae latae muscle before it leaves a branch for the hip joint.
Nerve to the Quadratus Femoris and Inferior Gemellus Muscles
This nerve leaves the plexus while crossing the sciatic foramen. In addition to supplying these two muscles, it also produces a small ramus for the hip joint.
Inferior Gluteal Nerve
The inferior gluteal nerve arises directly from L5 to S2. It penetrates the buttock through the lateral border of the sciatic foramen. It may have a common origin with the posterior cutaneous nerve of the thigh, but frequently these two nerves are separated. Beyond the piriformis muscle, the inferior gluteal nerve hooks around the inferior border of the gluteus maximus muscle and supplies it.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree