Altered Mental Status and Coma
J. Stephen Huff and Marcus L. Martin
Viewed from a physiologic perspective, consciousness is the sum of the activities and interactions of the reticular activating system and the cerebral cortex. A useful model is to think of the general state of alertness and wakefulness as arising in the reticular activating system, a group of neurons in the brainstem. Cognition, language, personality, and higher awareness of the environment are functions of the cerebral cortex. Coma results from the dysfunction of either the reticular activating system, the bilateral cerebral cortices, or both the reticular activating system and the cerebral cortices.
CLINICAL PRESENTATION
A patient with an altered mental status presents along a spectrum of consciousness. In the drowsy or lethargic state, there is slightly decreased wakefulness and interaction with the environment, but the patient may be aroused by verbal stimuli or light touch. Coma is the state in which the patient cannot be fully aroused to normal alertness by any environmental stimuli. The deeply comatose patient has failure of the arousal system and is unable to be awakened by vigorous sensory stimulation. Obtundation and stupor are intermediate states where the patient may be awakened only briefly by energetic stimulation. Rather than using clinical terms that are sometimes inexact, a simple description of the patient’s response to the examiner’s stimulus is preferred for clarity in communication.
Some other disorders of consciousness include the recently described “minimally conscious state” in patients with inconsistent but discernible evidence of partial consciousness; these patients may demonstrate sustained visual fixation and limited motor function including localizing stimuli and automatic movements such as scratching. The persistent vegetative state is characterized by complete absence of self or environmental awareness but with preserved capacity for stimulus-induced or spontaneous arousal. Sleep–wake cycles are preserved. The locked-in syndrome is a mimic of altered consciousness. Because of damage to efferent motor tracts, patients appear to lack responsiveness but have preserved consciousness, cognition, and emotion; they are tetraplegic and are unable to speak. Sometimes vertical eye movements are the only remnant of voluntary motor activity. This syndrome is often due to pontine infarction, but high cervical spinal cord injuries and severe drug-related dystonias may simulate the syndrome. Clinicians may underestimate the degree of awareness in patients with altered mental status and it is best to assume that some element of comprehension is preserved.
Pathophysiologic causes of coma may range from dysfunction at the cellular level to grossly visible pathologic changes of the brain. Impairment at the larger structural level includes focal injury to central nervous system (CNS) structures, which may result from increased intracranial pressure, reduction in cerebral perfusion pressure, or from direct destruction due to tumors, trauma, stroke, or hemorrhage. Dysfunction of many of the body’s organ systems may impair CNS function at a cellular level. This may occur with hypothyroidism or adrenal insufficiency, with disturbances of electrolyte regulation such as hypo- or hypernatremia, hypercalcemia, or other metabolic disturbances, such as hypoglycemia or hyperosmolar states. Illnesses resulting in renal or hepatic damage may cause encephalopathies with impairment of neurotransmitters likely being the mechanism. Hypoxia from pulmonary or cardiac etiologies may also affect CNS function. Hypotension with decreased cerebral perfusion may result from a primary cardiac etiology, sepsis, or volume loss from gastrointestinal (GI) bleeding or trauma. External environmental or toxic insults may also cause CNS depression through a direct effect at the cellular level or secondarily through damage to specific organ systems.
In general, when the CNS function is impaired at the cellular level, global CNS dysfunction follows and focal clinical findings such as hemiparesis or abnormal extraocular movements are not present on examination. Some notable clinical exceptions are hypoglycemia, hyperglycemia, and hepatic failure where focal findings may be seen. Pupillary light reflexes generally remain intact with toxic and metabolic causes of altered mental status, except when the CNS depression is caused by certain toxins that affect pupillary size, such as anticholinergics or opiates.
There are often focal findings on examination when a destructive process causes structural damage to a specific area of the CNS. Localized lesions of the CNS may also induce an additional injury process such as cerebral edema secondary to a tumor or hemorrhage, or vasospasm following aneurysmal subarachnoid hemorrhage.
DIFFERENTIAL DIAGNOSIS
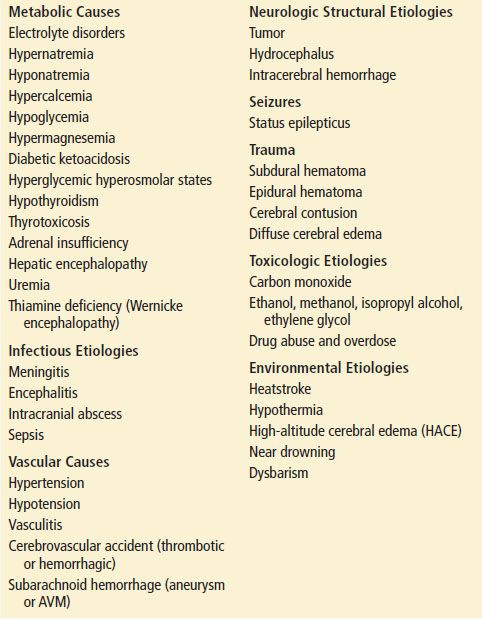
The differential diagnosis of coma is extensive (Table 11.1). In the emergency department (ED), history and physical examination will help narrow the possibilities. History will often suggest a likely cause and all sources—family, witnesses, emergency medical service (EMS) providers, and medical records—should be considered. The emergency physician must identify reversible causes and remediate injury when possible while simultaneously pursuing a strategy to sort the patient with altered mental status into structural, metabolic, infectious, toxic, environmental, or other etiologies. An organized approach is necessary to detect easily remedial cause, prevent ongoing neurologic injury, and determine a diagnostic strategy.
TABLE 11.1
Differential Diagnosis of Altered Mental Status and Coma
Hypoxia and Hypoglycemia
In the evaluation of any patient with mental status changes or coma, failure of substrate supply necessary for neuronal function (oxygen, glucose) must always be considered. After briefly evaluating for hypoxia and initiating oxygen supplementation, hypoglycemia, another common cause of altered mental status that is readily detectable and reversible, must be considered. Hypoglycemia is most common in patients on insulin therapy. It may be due to dosage errors, missed meals, a change in exercise pattern, or erratic absorption from injection sites. Interaction with other drugs, such as β-blockers or salicylates, may potentiate hypoglycemia. The oral hypoglycemic agents may also produce hypoglycemia. Many of these agents have a long duration of action, and pharmokinetics may change with overdosage, so the patient should be carefully observed for recurrent hypoglycemia or admitted. Hypoglycemia may also occur with alcohol intoxication and some other toxins. Renal or hepatic disease and other processes such as sepsis also increase the risk that a patient will develop hypoglycemia.
When blood glucose levels fall to a level of 50 to 70 mg/dL, symptoms of CNS excitation may appear; these may include anxiety, tremor, sweating, and occasionally hallucinations. As the glucose level falls further, progressive CNS depression and coma occur. Brainstem reflexes are preserved until late. Loss of consciousness is usually preceded by a period of confusion but may happen suddenly. Hypoglycemia may also cause focal neurologic signs including hemiparesis and should be considered early in the differential diagnosis of stroke. Other described signs of hypoglycemia include hyperreflexia, pupillary dilation, tachycardia, and primitive movements such as sucking movements of the lips, forced grasping, and extensor plantar responses.
Hyperglycemia
At the other end of the glycemic spectrum are the hyperglycemic conditions that may also cause altered mental status. Diabetic ketoacidosis (DKA) may be seen as the initial presentation of new-onset juvenile diabetes, in a known diabetic with poor compliance, or in a diabetic with a precipitating stressful event such as infection. A history of polyuria, polydipsia, nausea, vomiting, or abdominal pain may be obtained. Acetone-tinged breath or Kussmaul breathing may be present. Hyperosmolar hyperglycemic nonketotic coma typically occurs in an older patient with undiagnosed diabetes or type II diabetes experiencing another intercurrent illness. Gram-negative pneumonia, uremia with vomiting, or acute viral illnesses are the most commonly reported predisposing conditions. In contrast to DKA, the patient often has a longer period of symptoms before presentation.
Adrenal and Thyroid Emergencies
Though unusual in clinical practice, adrenal and thyroid emergencies are important to consider in the differential diagnosis of coma since treatment may be lifesaving. In a patient with suspected myxedema coma, history may reveal symptoms or prior treatment of hypothyroidism. Radioactive iodine treatment is associated with a relatively high incidence of delayed hypothyroidism. A history of noncompliance with thyroid medications may be obtained. Clinically, mild hypothermia, hypotension, and bradycardia may be present as well as periorbital and pretibial nonpitting edema. On neurologic examination, the muscle relaxation phase of the deep tendon reflexes is often described as delayed. Laboratory studies may reveal hyponatremia, hypo-osmolarity, and an elevated creatine phosphokinase as well as abnormalities in the thyroid laboratory panel.
Thyroid storm rarely presents as coma. Confusion, agitation, or occasionally hallucinations are more common. Temperature above 38°C (hyperthermia), tachycardia, and cardiac failure may be present. Often there is a precipitating event such as trauma or infection.
Acute adrenal crisis may occur because of an acute exacerbation of chronic adrenal insufficiency, rapid cessation of chronic steroid medications, or adrenal hemorrhage. Physiologic stressors such as infection, trauma, or surgery may all precipitate an adrenal crisis. Nausea, vomiting, abdominal pain, and fever may be present. Hypovolemic shock may develop and the mental status may deteriorate into lethargy or coma. A patient with known adrenal insufficiency or who is taking glucocorticoid replacement medication may not develop dehydration and hypotension until late in the course of adrenal crisis.
Hypertension
There is no distinct level of hypertension that correlates with mental status changes. In a patient with altered mental status and severe hypertension, possible causes include intracerebral hemorrhage or hypertensive encephalopathy. Hypertension is often present in subarachnoid or intracerebral hemorrhages. Hypertension, headache, altered mental status, and focal findings such as hemiparesis or aphasia are consistent with intracerebral hemorrhage. Subarachnoid hemorrhages may present with diffuse neurologic findings on examination and mental status changes range from confusion to coma. The classic history is the sudden onset of a severe headache associated with nausea and vomiting. A patient may give a history of prodromal headaches in the preceding weeks. In a small number of patients with subarachnoid hemorrhage, the computed tomography (CT) scan is normal. If a subarachnoid hemorrhage is suspected and the CT scan is negative, a lumbar puncture must be performed. Hypertensive encephalopathy is a diagnosis of exclusion. Funduscopic changes such as papilledema or hemorrhages will be present. Posterior reversible encephalopathy syndrome (PRES) is associated with uncontrolled hypertension and visual changes. MRI is the confirmatory procedure showing changes suggesting white-gray matter edema involving the posterior cerebral regions.
Toxic Causes
There are a wide variety of medications and illicit substances that may produce mental status changes. Correct diagnosis requires obtaining an adequate history and recognizing the toxidromes that appear in some specific toxic exposures.
High doses of benzodiazepines may produce sedative–hypnotic effects. Cardiac depression is usually minor, as is respiratory depression. However, respiratory depression may become severe if benzodiazepines are combined with other CNS depressants, in the elderly, or in patients with underlying respiratory disease.
Opiates and barbiturates may produce severe respiratory depression and hypotension. Miosis is usually present with opiates (exceptions are meperidine, propoxyphene, and tramadol, with which pupils may be of normal size). Pulmonary edema is most commonly seen with intravenous (IV) heroin overdose but may occur in other opiate or barbiturate intoxications. Cutaneous bullae and hypothermia may occur with sedative–hypnotic overdoses and are associated with prolonged unresponsiveness.
Ethanol intoxication may produce a somnolent, difficult-to-arouse patient with varying degrees of respiratory depression. Ingestion of ethanol substitutes such as methanol, ethylene glycol, or isopropyl alcohol also occurs in the alcoholic or with intentional overdoses. Isopropyl alcohol can present as stupor in a known alcoholic or as an encephalopathy of unknown cause in persons with hidden addictions. In addition to CNS depression, GI effects (abdominal pain, gastritis, nausea, or vomiting) and cardiac toxicity can occur. The major metabolite of isopropyl alcohol is acetone; as such, the severe anion-gap metabolic acidosis seen in methanol and ethylene glycol poisoning is not seen with isopropyl poisoning. In methanol intoxication, the patient may present with visual changes ranging from blurred vision to blindness. Calcium oxalate crystals may be present in the urine of patients who have ingested ethylene glycol. The osmolal gap should be calculated and any discrepancy that cannot be attributed to ethanol ingestion alone should prompt consideration of ingestion of other osmotically active substances.
Ingestion of tricyclic antidepressants may produce rapid mental status changes, coma, seizures, and cardiovascular effects. Sinus tachycardia is most commonly noted. The QRS complex may become widened and atrial or ventricular dysrhythmias may occur. Anticholinergic effects such as delayed gastric emptying, decreased bowel sounds, and mydriasis may be present.
A history of tinnitus and vomiting may lead the clinician to suspect salicylate intoxication. Chronic salicylism in the elderly is often subtle. Respiratory alkalosis in adults or metabolic acidosis in children may be seen. Acetaminophen and salicylate levels should be obtained in the patient suspected of an intentional ingestion. Carbon monoxide or cyanide toxicity should be suspected if the patient has been in a fire. Carbon monoxide poisoning should also be suspected in colder weather, particularly if the patient or others in the household have experienced flulike symptoms. Arterial blood gas levels may show a normal PO2, but the measured hemoglobin saturation may be low. Arterial blood co-oximetry should be performed to quantitate carboxyhemoglobin and to look for other abnormal hemoglobin complexes.
Seizures
Convulsive seizures are easily recognized. The clinician must remember that the seizures may be a symptom of a disease process, injury, ingestion, or withdrawal, and that epilepsy (unprovoked recurrent seizures) is largely a diagnosis of exclusion. Following generalized convulsions, patients often have altered mental status. Patients are frequently described as postictal, yet there is no definition or test for this condition or any consensus as to the duration. However, the clinician must always consider a broad differential diagnosis of altered mental status or complications of the seizures, particularly if the patient does not have improvement of level of consciousness over 20 to 30 minutes following cessation of the convulsive activity. Should the patient’s mental status not improve following cessations of generalized convulsions, the possibility of subtle status epilepticus must be considered. Subtle status epilepticus, also known as epileptic encephalopathy and by other terms, is present when the abnormal electrical seizure activity is continuing in the absence of motor movements. Nonconvulsive status epilepticus, sometimes used as a synonym, may also present with prolonged confusion or altered mental status. These uncommon nonconvulsive seizures with clouded consciousness or confusion require a high level of suspicion for recognition. Typically there is a history of seizures. Neurology consultation with electroencephalographic evaluation may be required for recognition.
DIAGNOSTIC APPROACH
The initial assessment of a patient presenting with coma or transient loss of consciousness should be performed in a relatively short time and combined with stabilization procedures. The state of consciousness is determined by assessing functions of both cerebral cortical and the ascending reticular activating system. Key observations will often help determine whether the disease is of the brainstem or cerebral hemispheres.
Before the unresponsive patient arrives in the ED, field personnel should assist with airway support and administer oxygen. The spine is immobilized and stabilized if there is the possibility of trauma. IV access is obtained, and cardiac monitoring is initiated. Point-of-care glucose testing should be performed if possible, and the patient should receive glucose if hypoglycemic or if there is suspicion of hypoglycemia. Support procedures not performed by field personnel should be quickly initiated in the ED.
The history, physical examination, and serial neurologic examinations are all of importance. However, life-threatening and reversible processes causing coma or altered level of consciousness should be considered before detailed history and physical examinations are performed; these include hypoxia, hypoglycemia, poisoning, infections, and increased intracranial pressure. Evaluation of the cardiorespiratory status and blood glucose takes precedence over investigation of other potential etiologies. Glucose administration to a patient with stroke or other brain injury may theoretically worsen the injury process and should be avoided when possible by using reliable point-of-care testing.
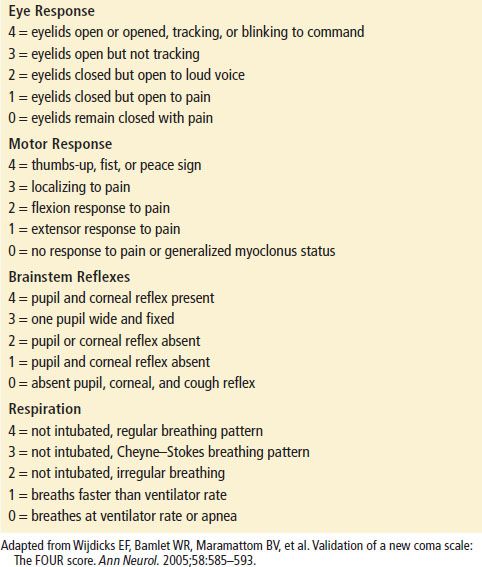
Obtaining historical information proceeds with patient stabilization. Information should include the abruptness of change in mental status, preceding events, medical history, current medications, and use of toxic agents. The clothing should be checked for suicide notes and drug bottles, and any medical alert tags should be noted. After the ABCs have been addressed, the patient is evaluated for signs of injury, including pupillary asymmetry and reactivity, hemotympanum, and other signs of head trauma. Assess vital signs including a core body temperature. The level of consciousness is documented, and the Glasgow Coma Scale is usually used to roughly quantify the patient’s condition though limitations of the scale have been noted (see Chapter 22). Recently the FOUR score has been validated for use in comatose patients. The FOUR score includes some assessment of brainstem reflexes and may find use in the ED (Table 11.2).
TABLE 11.2
The Four Score