CHAPTER 17 AIRWAY MANAGEMENT: WHAT EVERY TRAUMA SURGEON SHOULD KNOW, FROM INTUBATION TO CRICOTHYROIDOTOMY
The concept of immediate and appropriate airway management spans all disciplines of medicine. Achieving, protecting, and maintaining the airway have been well recognized as the initial steps necessary in resuscitation of the critically ill and/or injured patient. The basic premise of the Advanced Trauma Life Support for Doctors Course (ATLS®) is that all resuscitations should follow the mnemonic “ABCDE.” This mnemonic “defines the specific, ordered evaluations and interventions that should be followed in all injured patients,”1 where the “A” stands for airway, and the “B” for breathing.
The optimal airway is the airway that the awake patient can maintain without assistance, while the worst-case scenario is an airway that can only be achieved with surgical intervention. The success or failure to achieve an adequate and protected airway is dependent on many factors. Techniques available to the clinician range from the simple to the complex. The concept of tracheal intubation is by no means a new one. In fact, the first documented report of tracheal intubation dates back to 1543, and actually refers to a tracheostomy. In his atlas On the Fabric of the Human Body, the Renaissance anatomist Anreas Vesalius observed, “Life may, in a manner of speaking, be restored. An opening must be attempted in the trunk of the trachea into which a reed or cane should be put; you will then blow into this so that the lung may rise again.”2
AIRWAY ANATOMY
Successful execution of any procedure demands a thorough understanding of the procedure: indications, technical requirements, and necessary equipment to complete the task. In addition, the operator must be cognizant of potential complications and their management. Obtaining an airway, whether by conventional or surgical means, is no different than any other procedure.3,4 The anatomy and normal functions of the structures that comprise the upper airway are complex. The surgeon must recognize the essential anatomic structures to effectively manage the airway.
Although separated anteriorly by the palate, the mouth and nasal cavities join posteriorly at the end of the soft palate to form the pharynx. The pharynx is separated into the nasopharynx and the oropharynx. The pharynx extends to the inferior border of the cricoid cartilage anteriorly and the inferior border of the body of C6 posteriorly. The wall of the pharynx is composed of two layers of pharyngeal muscles: the external circular layer consists of the constrictor muscles and the internal longitudinal layer consists of muscles that elevate the larynx and pharynx during swallowing and speaking. The nasopharynx follows directly from the nasal cavity at the level of the soft palate, and communicates with the nasal cavities through the nasal choanae and with the tympanic cavity through the Eustachian tube. It contains the pharyngeal tonsils in its posterior wall. The oropharynx begins at the soft palate and continues to the tip of the epiglottis. It contains the palatine tonsils, important landmarks in the Mallampati airway classification.5
The epiglottis is a spoon-shaped plate of elastic cartilage that lies behind the tongue. It prevents aspiration by covering the glottis—the opening of the larynx—during swallowing. The laryngopharynx/hypopharynx extends from the upper border of the epiglottis to the lower border of the cricoid cartilage. It is separated laterally from the larynx by the arytenoepiglottic folds, which contain the piriform recesses. The piriform sinuses are found at each side of the opening of the larynx, in which the inferior laryngeal nerve lies and swallowed foreign materials may be lodged.
Unlike the thyroid cartilage, which does not project posteriorly, the cricoid cartilage is a complete signet-shaped cartilaginous ring connected to both the thyroid cartilage and the first tracheal ring. This anatomic relationship was used by Sellick,6 who described the prevention of passive regurgitation of gastric contents by posterior pressure on the cricoid cartilage during the induction of general anesthesia, a technique that has since become the accepted standard of care.
The epiglottis is an elastic cartilaginous structure covered by a mucous membrane. The reflection of this mucous membrane forms a slight depression known as the vallecula. It is at this point that the tip of the laryngoscope blade is placed so as to elevate the epiglottis and visualize the vocal cords. The epiglottis is anteriorly attached, superiorly to the hyoid bone by the hypoepiglottic ligament, and inferiorly to the thyroid cartilage by the thyroepiglottic ligament. The quadrangular ligament extends between the lateral aspects of the arytenoid and epiglottic cartilages. Its free inferior edge is the vestibular ligament, and, covered with mucosa, it forms the vestibular fold, which lies above the vocal cord (fold) and extends from the thyroid to the arytenoid cartilage. The arytenoids articulate with the superolateral aspect of the cricoid, and each has an anterior vocal cord process that attaches to the vocal cords via the cord ligament. The free superior margin forms the aryepiglottic ligament, and its mucosal covering forms the aryepiglottic fold. It is within the posterior aspects of aryepiglottic folds that the cuneiform and corniculate cartilages can be seen. These cartilages rest on the apex of the arytenoids. Their elastic properties facilitate the return of the arytenoid cartilages to their anatomic position of rest after abduction, and can usually be seen during direct laryngoscopy. They can, therefore, be used as a landmark for the tracheal opening when it is difficult to visualize the vocal cords (Figure 1).
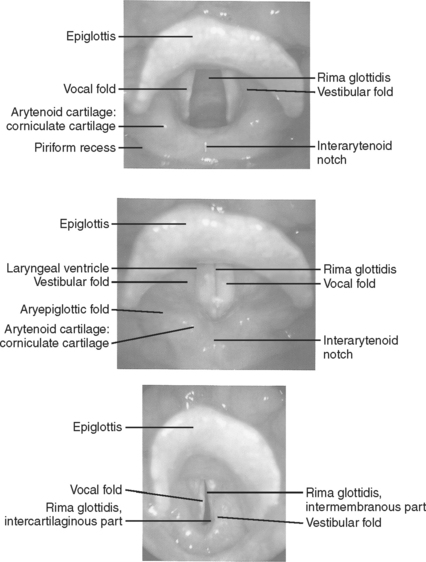
Figure 1 Landmarks of the tracheal opening.
(From Putz R, Pabst R, editors: Sobotta Atlas of Human Anatomy, 13 ed Baltimore, Williams & Wilkins, 2001, with permission.)
The glottis is contained within the larynx, and is the narrowest part of the adult airway. It is composed of the vocal cords (or folds) and the space between them is called the rima glottides. Because the true vocal cords are covered by stratified epithelium, they have the characteristic pearly white color when illuminated. The cords are innervated by the recurrent laryngeal nerves, and the musculature of the larynx receives its innervation from branches of the vagus nerve (cranial nerve X). The larynx is inclusive of the structures noted previously.
ASSESSING THE AIRWAY
Patient anatomy, both inherent and as altered by injury, is an important factor that requires careful assessment by the clinician prior to attempting intubation, whether nasal, orotracheal, or surgical. In the trauma patient, the clinician must always be cognizant of the potential for cervical spine injury. This is particularly important in the patient whose physical exam is compromised by an altered mental status, regardless of the cause. The presence of maxillofacial trauma or injuries of the soft tissues of the neck must also be considered when deciding the best way to secure and protect the airway. In the absence of injury or pathologic conditions, the ability to ventilate and control the supraglottic airway is a function of the size of the airway and the compliance of the supralaryngeal tissues. It should be remembered that under normal conditions air flow through the nasal cavity is not usually a concern in that this portion of the airway is usually supported by rigid elements in its walls. Conversely, the pharynx does not have a rigid support system, and therefore, it is predisposed to collapse. It can also be obstructed by the tongue in obtunded or comatose patients; in most cases this collapse and/or obstruction can initially be dealt with effectively with the use of the oral airway.7
A more ominous situation arises when the airway is compromised in the immediate vicinity of the laryngeal inlet because of the size of the base of the tongue or the epiglottis. Air flow in this region will be inversely proportional to the size of these structures, as well as the condition of the perilaryngeal tissues. Trauma to the neck causing anatomic disruption and/or tissue edema, prior irradiation to the neck, head and neck tumors, or redundant fatty tissue in the perilaryngeal area secondary to obesity will all restrict normal air flow. These conditions may lead to the “cannot-ventilate-and-cannot-intubate scenario,” a potentially lethal situation in even the most competent intubators.7
As with any other medical procedure, it is always prudent to perform a methodical evaluation of the situation, and determine the preferable approach and equipment needed to perform the task efficiently. In addition to factors previously discussed, one must also assess for scarring and fibrosis to the airway and surrounding tissues, injury to the trachea; congenital anomalies; acute inflammatory or neoplastic diseases of the airway; and finally gingival, mandibular, and dental anomalies/disease.8 Short, muscular individuals with very short necks and obese patients tend to be difficult to intubate. Morbidly obese patients can compromise the airway with excessive redundant tissue in the paratonsillar and paraglottic areas, masking visualization and accessibility of the glottis during laryngoscopy. Anatomic factors that should be assessed include mandibular mobility at the temporomandibular joints; mobility of the head at the atlanto-occipital joint (when cervical spine injury has been ruled out); the length, size, and muscularity of the neck; size and configuration of the palate; the proportionate size of the mandible in relation to the face; and the presence of an overbite of the maxillary teeth.
Difficulty in laryngoscopic visualization varies in accordance with the extent of anatomic variation or pathologic conditions. The Mallampati classification is routinely used by anesthesiologists to evaluate the airway in elective cases (see Figure 1 on page 59).
In order to classify a patient, the patient is asked to open the mouth as widely as possible and protrude the tongue out as far as possible while seated, with the head in the neutral position,8 something that is almost impossible to accomplish in the trauma setting. Evaluation of the atlanto-occipital extension is another tool that is used by anesthesiologists in the elective setting. Because this requires an awake patient who can sit upright and flex and extend the neck, it is not useful in the trauma setting. However, a clinician familiar with the Mallampati classification can perform a cursory evaluation of the oropharynx using a tongue blade or laryngoscope, which provides the clinician some idea as to the potential for difficulty in intubation. It will also demonstrate the existence of any evidence of injury to the oropharynx, the presence of foreign bodies, blood, or vomitus.
CONTROLLING THE AIRWAY
The best airway is the airway that the patient can safely maintain without any external intervention. The Eastern Association for the Surgery of Trauma has sited the need for emergency tracheal intubation in trauma patients with airway obstruction, hypoventilation, severe hypoxia in spite of supplemental oxygen administration, severe cognitive impairment (GCS score <8), cardiac arrest, and severe hemorrhagic shock.9 Once it has been decided that the airway is not adequate, or that the patient is unable to protect the airway, then intubation must be accomplished in an efficient and safe manner. It is important to remember that all trauma patients must be intubated with one person maintaining in-line cervical immobilization throughout the procedure to protect the possibly injured cervical spine.
As with all other procedures, a successful outcome depends on the operator’s experience and on having immediate access to all of the correct equipment. Most emergency departments have airway carts that contain all of the equipment that will routinely be needed for emergency intubations, as well as specialty carts designed for the “difficult airway.” While the contents of these carts will vary from institution to institution, they will usually be standardized within each hospital. Examples of stocking lists for the standard airway cart (Figure 2) and the difficult airway cart appear in Tables 1 and 2, respectively.
Table 1 Respiratory/Airway Cart
| Top of Airway Cart |
| Stat respiratory rx box |
| 2 − 2’s |
| Hurricane spray |
| Benzoin (1) |
| 2% xylocaine jelly (1) |
| Surgilube (1) |
| EID (1) |
| #7, 7.5, 8 ETT (1 @) |
| Stylette (1) |
| 12-cc syringe (1) |
| #18 NG tube (1) |
| 60-cc catheter tip syringe (1) |
| Magill forceps (1) |
| Green, yellow, red oral airway (1 @) |
| Laryngoscope handle |
| #2, 3, 4 Mac blades (1 @) |
| #2, 3 Wis/Miller blades (1 @) |
| Top Drawer |
| #6, 6.5, 7, 7.5, 8, 8.5, 9 ETT (2 @) |
| Stylette (2) |
| #2, 3 Miller blades (1 @) |
| #2, 3, 4 Miller blades (1 @) |
| Drawer 2 |
| PEEP valves (2) |
| Nasal cannulas (2) |
| ETCO2 sensors (2) |
| Adult O2 sensors (2) |
| Green, yellow, red oral airways (2 @) |
| #28, 30, 32 nasal airways (1 @) |
| Tube holders, IV tubing, tape, Dale holders |
| Drawer 3 |
| Luekens trap (2) |
| #18, 14 NG tube (2 @) |
| Surgilube |
| 2% xylocaine jelly |
| Yankauer (2) |
| Suction catheters (2) |
| Drawer 4 |
| Transtrach jet (1) |
| Bag-in aerosol setups with meds (2) |
| Rebreather masks (2) |
| Venti masks (2) |
| Drawer 5 |
| BVM (2) |
| Cross-vent circuits (2) |
| Extra vent sheets |
| Left Side Facing Front |
| Waste bin |
| BVM |
| Right Side Facing Front |
| Sterile gloves |
Table 2 Difficult Intubation Cart
| Outside of Cart |
| Jet ventilator present and connected to 50-psi regulator |
| Jet vent tank, regulator attached, >1500 psi (50 psi/1–15 lpm regulator) |
| Portable CO2 monitor with line attached and charger (in top drawer) or |
| CO2 clip colormetric detector |
| Drawer 1 |
| Intubation stylette 6 Fr., 10 Fr., 14 Fr. (1 @) |
| 2% lidocaine jelly (1 @) |
| Cetacaine spray (1 @) |
| 4% lidocaine solution (1 @) |
| Nasal spray (1 @) |
| 14 Fr. Jelco (5 @) |
| Magill forceps, pediatric (1 @) |
| Magill forceps, adult (1 @) |
| Bite block (1 @) |
| Fiberoptic bronchoscope adapter swivel (2 ea) |
| Ovasappian airway (2 ea) |
| Sampling elbow (1 @ch) |
| Sampling tee (1 @ch) |
| Sample tubing for CO2 monitor (2 @ch) |
| MAD (mucosal atomization device) (1 @) |
| Drawer 2 |
| Fiberoptic laryngoscope handle standard size ((1 @) |
| Fiberoptic laryngoscope handle penlight size (1 @) |
| Fiberoptic laryngoscope handle stubby size (1 @) |
| Fiberoptic laryngoscope blade Miller 1, 2, 3, 4 (1 @) |
| Fiberoptic laryngoscope blade Mac 2, 3 (1 @) |
| Fiberoptic CLM laryngoscope blade size 3, 4 (1 @) |
| Drawer 3 |
| Endotracheal tube cuffed 4.0, 5.0, 5.5, 6.0, 6.5, 7.0, 7.5, 8.0, (2 @) |
| Endotrol endo tube 6.0, 7.0 (2 @) |
| MLT endotracheal tube 6.0 (2 @) |
| Drawer 4 |
| Endotracheal tube uncuffed w/monitoring lumen 2.5, 3.0, 3.5, 4.0, 4.5, 5.0, 5.5 (1 @) |
| Drawer 5 |
| Sheridan Combitube© 41 Fr., 37 Fr. (1 @) |
| Mask size child (1 @) |
| Mask size small adult (1 @) |
| Mask size large adult (1 @) |
| Drawer 6 |
| LMA size 3 (1 @) |
| LMA size 4 (1 @) |
| Duoflex long guidewire (1 @) |
| Hyperinflation bag 3 liter (1 @) |
| Retrograde intubation kit (Cook) (1 @) |
| Cook airway exchange catheter 3 mm, 4 mm, 5 mm, 6 mm, 7 mm (1 @) |
| Cook “Frova Catheter” (1 @) |
| Cook “Melker” emergency cricothyrotomy catheter sets size 3.5, 4.0 (1 @) |
| Fastrach intubating LMA size 4 with endotracheal tubes and pusher (1 @) |
| Tissue spreader (1 @) |
| Bougie (1 @) |
| Olympus LF-GP |
| Cabinet for FOB |
| Cric Set |
| 2 Army Navy retractors |
| 2 thyroid retractors |
| 1 needle holder |
| 2 curved hemostats |
| 2 straight hemostats |
| 1 trach spreader |
| 2 Jackson tracheal hooks |
| 2 disposable scalpels |
| 2 sutures |
| Check |
| Satisfactory batteries in laryngoscope |
| Outdates on drugs and supplies |
Oropharyngeal and nasopharyngeal airways (see Figure 2) are useful, but must be inserted with care. While neither one is well tolerated by the awake patient, the nasopharyngeal airway is better tolerated in the semiresponsive patient, and is less likely to stimulate gagging and vomiting.10 They can both be used to help maintain a patent upper airway in the obtunded patient. In the adult, the oral airway is inserted with the convexity facing down initially, and then rotated 180 degrees once in the oropharynx. It must be placed carefully, so that it does not push the tongue posteriorly, but rather, is seated posterior to the tongue displacing the tongue anteriorly. In children, the oral airway must always be placed with the convex surface facing cephalad initially to avoid injury to the soft tissues of the mouth and pharynx. It is important to remember that in patients with a persistent (intact) upper airway gag reflex, the insertion of the oral airway can precipitate laryngospasm and bronchospasm, as well as coughing, gagging, vomiting, and ultimately, aspiration.11










