CHAPTER 75 AIRWAY MANAGEMENT IN THE TRAUMA PATIENT: HOW TO INTUBATE AND MANAGE NEUROMUSCULAR PARALYTIC AGENTS
Injury is the leading cause of death in persons between the ages of 1 and 45 years in the United States and the third leading cause overall. Airway compromise is a common cause of death or severe morbidity in trauma victims. Management of the airway is a fundamental skill in trauma medicine. Obstruction of the airway has been reported in two-thirds of patients who die in the prehospital setting when death was not inevitable. Airway care is a cornerstone of resuscitation and is the first priority for patients both in the prehospital setting and in the emergency room (ER).
AIRWAY CONSIDERATIONS IN THE TRAUMA PATIENT
There is an increased risk for awareness among trauma patients during airway manipulation and surgery. The incidence of awareness in the general adult patient population undergoing anesthesia is 0.1%–0.2%. Approximately 50% of these patients will have some psychological impact from their experience, and the most severe reaction is full-blown post-traumatic stress syndrome. The incidence of awareness is reported to be higher among trauma patients. These patients often have such hemodynamic instability that they tolerate only very light levels of anesthesia. It is, therefore, good practice to always consider giving amnesia-inducing drugs when neuromuscular blocking agents are used. To be paralyzed and unable to communicate is an extremely traumatic experience.
EVALUATION OF AIRWAY AND RESPIRATORY FUNCTION
In recent years, the development of classification systems to predict difficult intubations has reduced the incidence of airway complications in patients undergoing elective surgery. The Mallampati classification of the airway (see page 59) is commonly used and is based on assessment of tongue size in relation to other pharyngeal structures. The I to IV scoring scale predicts difficulty of intubation. The atlanto-occipital joint extension test measures the ability to extend the neck and, consequently, the ability to align pharyngeal and laryngeal axes to accommodate intubation. Measurements of the thyro-mental distance, sterno-mental distance, mandibulo-hyoid distance and inter-incisor distance are also helpful in evaluating the airway.
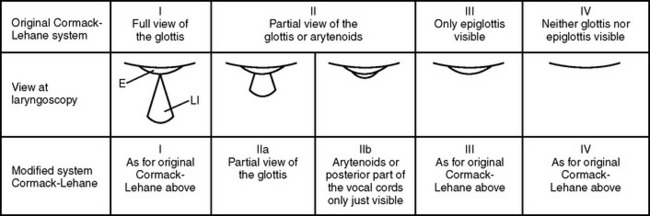
To provide high specificity and sensitivity for successful intubation and to assess the level of difficulty of an endotracheal intubation, several tests must be performed. These tests are usually correlated to the visualization of laryngeal structures and vocal cords. The gold standard for classifying the degree of exposure to the larynx entrance is the description by Cormac and Lehane (Figure 1). Grades III and IV are associated with difficult intubation. The dilemma is that all these tests are difficult to utilize in the trauma patient for many reasons, including an immobilized neck. Thus, alternative scoring systems such as the LEMON method have been proposed.
The LEMON method was developed by the U.S. National Emergency Airway Management Course and has a maximum score of 10 points, calculated by assigning 1 point for each criterion (Table 1). It has been demonstrated that an airway assessment score based on the LEMON criteria is helpful in predicting difficult intubation in the ER. The LEMON test is designed to be a quick and easy-to-use assessment tool. A poor laryngoscopic view is more common, for example, among patients with large incisors, a reduced inter-incisor distance, and a reduced thyroid-to-floor-of-mouth distance.
| Physical Sign | Less Difficult Airway | Indicators of Difficult Airway |
|---|---|---|
| Look at exterior | No face or neck pathology | Face or neck pathology, obesity, and so on |
| Evaluate the 3-3-2 rule | Mouth opening >3F | Mouth opening <3F |
| Hyoid–chin distance >3F | Hyoid–chin distance <3F | |
| Thyroid cartilage–mouth floor distance >2F | Thyroid cartilage–mouth floor distance <2F | |
| Mallampati | Classes I and II | Classes III and IV |
| Obstruction | None | Obstruction within or surrounding upper airway |
| Neck mobility | Normal extension and flexion | Limited range of motion |
F, Finger-breadths.
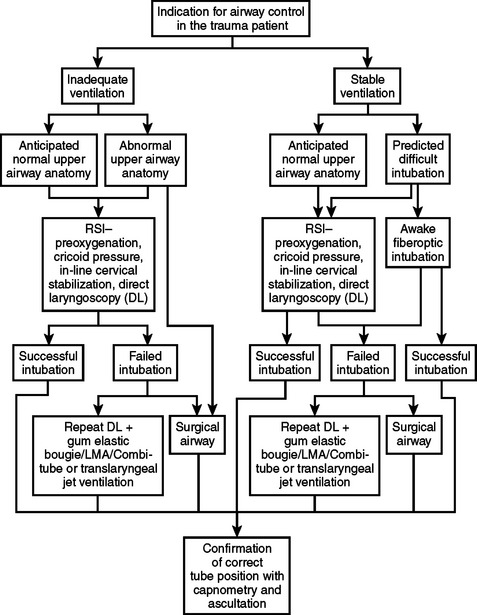
Planning an approach is the final step of the assessment (Figure 2). The team should then proceed with the airway management plan. When the patient can maintain adequate oxygenation and ventilation, and time permits, it may be beneficial to transport the patient to the OR which normally has better equipment and resources than the ER. In other situations, the right decision may be to immediately establish a surgical airway with the patient breathing spontaneously.
INDICATIONS FOR INTUBATION AND CONTROLLED VENTILATION
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree