Figure 17.1. Nasal airway anesthesia. Cotton pledgets soaked with anesthetic are inserted along the inferior and middle turbinates to produce anesthesia of the underlying sphenopalatine ganglion by transmembrane diffusion of the solution. Wide pledgets are needed to provide maximal topical anesthesia and vasoconstriction of the nasal mucosa as well.
C. Tracheal anesthesia is also unwise if preservation of active cough reflexes is desired.
D. Airway anesthesia is also useful in facilitating diagnostic fiberoptic laryngoscopy, and may help agitated intubated patients in intensive care units tolerate the presence of an endotracheal tube.
III. Drugs
A. Direct blockade of the superior laryngeal nerves can be performed by infiltration with local anesthetic agents such as 1% or 1.5% lidocaine.
B. The other innervation of the airway is just as easily approached by topical anesthesia. Higher concentrations of local anesthetics are required for topical application to overcome the usual slow penetrance of the drugs across mucosal membranes. Commercial preparations of local anesthetics (such as 10% flavored lidocaine) are available as oral sprays, but the delivered quantity cannot be measured. A better approach is to nebulize a known quantity of anesthetic (such as 10 mL of 4% lidocaine) with an atomizer such as those used in otolaryngology. Lidocaine 4% and tetracaine 0.5% to 1% are available for transtracheal injection or oral topical application in this manner. These high concentrations carry the obvious risk of rapidly exceeding the maximum recommended doses of these agents. This problem is further compounded by the common practice of using unmeasurable quantities of several different drugs for the multiple blocks performed.
C. Nasal anesthesia carries the additional requirement for vasoconstriction to reduce the incidence of bleeding from the nasal mucosa. Cocaine 4% has been the traditional agent of choice because it is the only local anesthetic with intrinsic vasoconstrictor properties. Because of cocaine’s high toxicity and abuse potential, the use of 3% lidocaine with 0.25% phenylephrine may be a better alternative for nasal topical anesthesia.
IV. Technique
Airway anesthesia can be performed with the patient in the supine position, but it is often more comfortable for the patient if it is done with the head slightly elevated or in the sitting position. If full mental alertness is not required, a mild sedative such as dexmedetomidine (which has minimal respiratory depression) can be used.
A. Nasal mucosa
1. For the nasal mucosa, cotton pledgets on long applicators are soaked in 4% cocaine (or a mixture of lidocaine-phenylephrine) and inserted gently into both nares. The first applicator is inserted directly posterior along the inferior turbinate to the posterior pharyngeal wall (Figure 17.1).
2. A second applicator is inserted with a slight cephalad angle to follow the middle turbinate and is again advanced to its full depth until it touches the mucosa over the sphenoid bone.
3. Anesthesia is performed bilaterally, because the object is to provide anesthesia of the branches of the sphenopalatine ganglion as well as topical anesthesia of the mucosa itself. Two to 3 minutes of contact time is usually required to provide adequate penetration of the agent into the mucosa. Cotton-tipped applicator sticks are available in most operating rooms, and are tolerated by patients. The more generous sized pledgets used by otolaryngologists are less comfortable, but more effective in providing adequate surface area for delivery of the anesthetic.
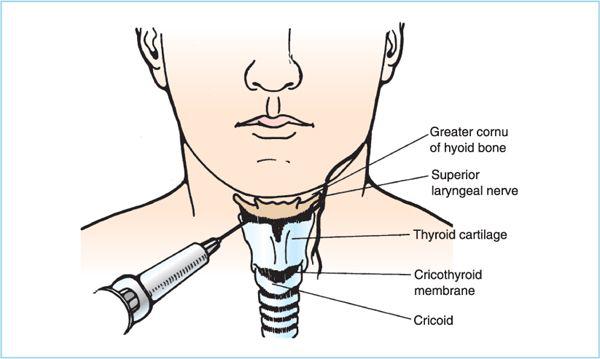
B. Superior laryngeal block
1. While the nasal applicators are in place, the superior laryngeal nerves are blocked bilaterally. The patient’s head is extended, and the thyroid cartilage and hyoid bone are identified. The index finger retracts the skin down over the superior ala of the thyroid cartilage, and the skin is wiped with an alcohol swab. A 23- or 25-gauge needle on a 5-mL syringe filled with 1% lidocaine is inserted onto the tip of the cartilage. The index finger then releases the skin traction, and the needle is “walked off” the cartilage superiorly and is inserted just through the firm thyrohyoid membrane. The tip now lies in the loose areolar tissue plane beneath the membrane (Figure 17.2). After aspiration to detect unwanted intravascular placement, 2.5 mL is injected into the plane beneath the membrane. This sequence is repeated on the opposite side.
2. Alternatively, the needle can be inserted onto the posterior (greater) cornu of the hyoid bone and “walked” caudad off the bone onto the membrane.
Figure 17.2. Superior laryngeal nerve block. The 23- to 25-gauge needle is introduced onto the superior border of the lateral wing of the thyroid cartilage. It is then gently advanced off the cartilage to drop through the thyrohyoid membrane. After gentle aspiration to exclude intravascular injection, 2 to 3 mL of local anesthetic is injected into the space below the membrane.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree