CHAPTER 87 ADVANCED TECHNIQUES IN MECHANICAL VENTILATION
Since the introduction of mechanical ventilation using a bicycle tire and bellows about 50 years ago, the science and art of respiratory therapy has advanced dramatically—allowing the clinician to ventilate and oxygenate patients who would have died in the past due to limitations of man and machine. This chapter focuses on recent advances and future considerations in ventilatory support to allow further improvements in respiratory care and survival from acute lung injury (ALI), acute respiratory distress syndrome (ARDS), and chronic respiratory failure.
ALTERNATIVES TO CONVENTIONAL MECHANICAL VENTILATION
Pressure-Controlled Ventilation
Pressure-controlled ventilation (PCV) is pressure-limited timecycled breathing that is completely controlled by the ventilator, with no participation by the patient. Inspiratory airway pressure increases early in the respiratory cycle, and is maintained at that specified pressure throughout the remainder of the delivery phase. The major benefit of PCV relates to the inspiratory flow pattern and its benefit in gas delivery for patients with suppressed respiratory efforts. In pressure-cycled breathing, the inspiratory flow decreases exponentially during lung inflation in order to keep the airway pressure at the preselected value. Thus, this type of flow pattern can improve gas exchange. The primary disadvantage of PCV is the tendency for inflation volumes to vary with changes in the mechanical properties of the lungs. There is a proportional relationship between the lung inflation and the peak inflation pressure. When a constant peak inflation pressure is reached, the inflation volume decreases as the airway resistance increases or lung compliance decreases. The result is fluctuation in inflation volumes due to reliance on a specific pressure target.
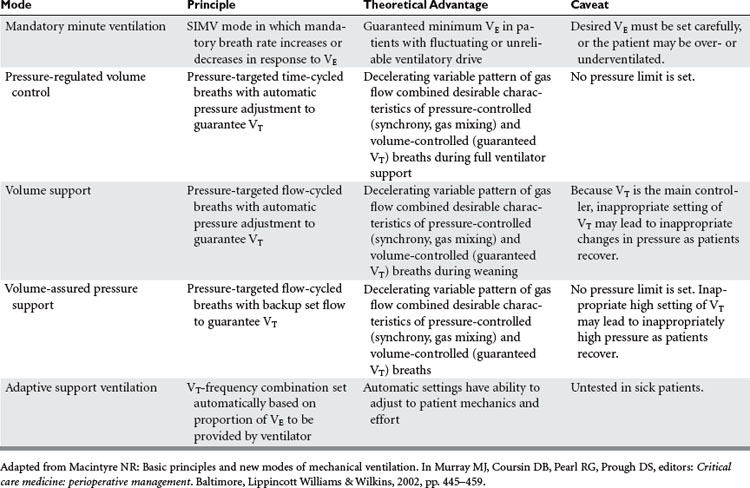
Mandatory Minute Ventilation
Mandatory minute ventilation (MMV) is a mode of mechanical ventilation in which the minimum level of VE needed by the patient is provided. If the patient’s spontaneous ventilation is insufficient to meet the predetermined VE, the ventilator provides the difference. Conversely, if the patient’s spontaneous breathing exceeds the target VE no ventilator support is provided. This mode is one of the so-called “closed-loop” ventilation modes (Table 1) because the ventilator varies its parameters in response to the patient’s own intrinsic ventilatory requirements. The major advantage of MMV is the capability to vary ventilatory support according to the response of the patient. This mode of mechanical ventilation is best suited for patients with severe neuromuscular disease or drug overdose, or patients heavily sedated. One of the main disadvantages with MMV is that alveolar ventilation may not be matched equally with exhaled VE, thus diminishing closing volumes and leading to atelectasis. None of the closed-loop modes, MMV included, has been tested sufficiently on critically ill patients to recommend widespread incorporation into practice.
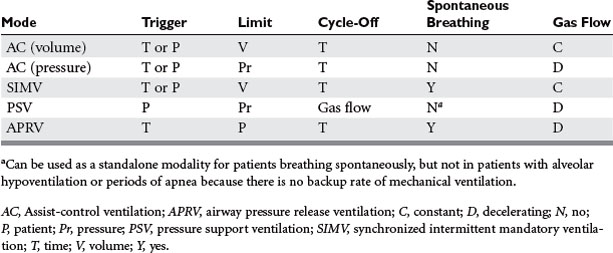
Airway Pressure Release Ventilation
Airway pressure release ventilation (APRV) (Table 2) has been used as an alternative mode of mechanical ventilation in patients with acute respiratory failure. APRV, which has been available in some ventilator models since the mid-1990s, allows for the unloading during exhalation of any positive pressure provided during inhalation in order to facilitate the egress of the tidal breath. Release of airway pressure from an elevated baseline simulates exhalation. Technically, APRV is time-triggered, pressure-limited, time-cycled mechanical ventilation. Conceptualizing APRV as continuous positive airway pressure (CPAP) with regular, brief, intermittent releases of airway pressure may facilitate understanding. It can augment alveolar ventilation in the patient breathing spontaneously, or provide full support to the apneic patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree