135 Acute Radiation Emergencies
• The nature and extent of an acute radiologic emergency should be identified to determine whether hospital disaster plans should be activated.
• Large-scale radiologic emergencies require triage of multiple patients based on the estimated radiation dose, presence of traumatic injuries, and availability of local resources.
• An emergency physician can use the symptoms and findings on physical examination to estimate the whole-body radiation dose (rad or gray) for predicting a patient’s course and subsequent need for treatment.
• A complete blood count with differential at triage and 24 to 48 hours later can be used to guide the diagnosis, treatment, and prognosis of acute radiation syndrome.
• Decontamination is an important aspect of acute radiation emergencies but should not supersede stabilization of unstable patients.
• Recognition of patients who have been exposed to moderate to high doses of radiation and triage to early treatment of acute radiation syndrome can significantly decrease mortality.
Epidemiology
Acute radiologic emergencies are a rare occurrence, yet with increasing use of radioisotopes in medicine, research, and industry, as well as ongoing use in national defense and electrical power generation, it is imperative that emergency physicians (EPs) be versed in acute medical management after radiologic emergencies. The relative magnitude of the situation and the resources needed to address an emergency vary depending on the scale of the exposure event. Small-scale events include contained exposure in hospitals or research facilities or contained breaches at nuclear power plants in which small amounts of material may lead to exposure or contamination of a limited number of individuals. Large-scale events involve relatively large quantities of radioactive material or potential widespread exposure or contamination of a significant population. Examples of large-scale events include nuclear reactor meltdowns (e.g., Fukushima Daiichi, Japan, in March 2011; the Chernobyl meltdown in April 1986), detonation of nuclear weapons, or terrorist attacks with a radiologic dispersal device—otherwise known as a “dirty bomb.”1,2 Hospitals are required by the Joint Commission to have disaster plans in place for mass casualty events, including radiologic emergencies, and EPs and emergency medical service personnel will be at the forefront of decision making and patient care when a radiologic event occurs.
The first priority during an acute radiation emergency is to establish the reality and type of radiologic event. Information received from the field is essential in mounting an effective response in the emergency department (ED) and the hospital. Important information to obtain from the field, if possible, is listed in the Documentation box. With large events, EDs should anticipate patients arriving from multiple field triage and stabilization sites, as well as individuals who arrive on their own accord without first being triaged or evaluated for injury or radiation exposure or contamination.
![]() Documentation
Documentation
Important Information to Obtain from the Field after Acute Radiologic Emergencies
Type of radioactive material involved. Different types of radioactive material can expose patients in different ways. Important specifics include the type of radioisotope or source (α-, β-, γ-emitters, or neutrino), the form that it was in when the exposure occurred, and whether those exposed were also contaminated via inhaled dust or ingestion
Types of traumatic injuries occurring with the radiation exposure (blast or burn)
Type of decontamination procedures taking place at the scene or in field triage
Number of patients expected to require triage, evaluation, and treatment
What local, regional, or federal resources have been activated and notified of the acute radiologic emergency
Communication between the field triage team and the ED must be clear because no federal or internationally agreed-upon medical triage systems have been established specifically for radiation mass casualty incidents, and thus existing mass casualty emergency triage algorithms should be used with modifications for the impact of the radiation exposure or contamination.1,3–5 The Scarce Resources for a Nuclear Detonation Project has published new triage recommendations for the first 4 days following a possible nuclear detonation, and formal guidelines will probably be recommended in the near future.5–7
The disaster response coordinator should prepare the ED to receive patients triaged at all levels with blast, thermal, and radiation injuries. Importantly, standard personal protective equipment sufficient to protect the emergency personnel treating these patients in the decontamination area and in the ED must be used.1,8–11 Those triaging and caring for patients with possible contamination should be using strict isolation precautions.
In any acute radiation emergency, initial mass casualty field triage should not be confused with the subsequent clinical triage used by EPs and other providers for more definitive medical management. It is essential that those involved in triage and provision of emergency care for radiologic emergencies understand that lifesaving medical stabilization takes precedence over other concerns, including external radiation decontamination.1,4,10–12
Pathophysiology
Radioactivity refers to the loss of particles or energy from an unstable atom that is decaying. There are two distinct types of radiation: ionizing radiation (e.g., α and β particles from a decaying radioisotope and nonparticulate electromagnetic γ-rays and x-rays) and nonionizing radiation (e.g., all forms of the electromagnetic spectrum, except for γ-rays and x-rays).The main means of exposure to a dose of radiation are (1) from an external radiation source, (2) by loose radioactive material deposited on the skin or into wounds, and (3) by ingestion or inhalation of radioactive material.1 Significant radiation injuries can occur from irradiation with or without contamination (contact of the substance directly with human tissue). A contaminated patient will have been exposed to radioactive material that could still be on or inside the patient’s body. Irradiated patients without contamination have been exposed but do not have radioactive material on or in them. Irradiated patients are not “radioactive.” Such differentiation in a radiologic emergency situation is important because it dictates whether decontamination is needed. A radioactivity meter (most commonly a Geiger counter is the initial screening tool) and the patient’s history should be used to determine whether a patient has been contaminated.
To comprehend the physiologic effects of radiation, it is important to understand the units of measurement for types of doses (see the Facts and Formulas box). Radiation damage occurs within microseconds of exposure and most significantly affects rapidly reproducing types of cells (e.g., intestinal crypt cell, stem cells) or cells with a large nucleus, such as lymphocytes. The threshold of 2 Gy of whole-body irradiation is often used as the reference point for when cells have been irreparably damaged and symptoms of acute radiation syndrome (ARS) develop.1,12
![]() Facts and Formulas
Facts and Formulas
Dose Equivalent or Equivalent Dose (SI Terms)
Triage Formula for Irradiated Patients When CBC with Differential Is Available (Adapted from AFRRI, 2010; REAC/TS, 2011)
In otherwise healthy adult patients who have been exposed to external irradiation without trauma or burn, a clinically detrimental radiation dose can be distinguished from a dose lower than 1 Gy 4 hours after exposure by using a triage score involving two criteria: the N/L ratio and whether emesis has occurred in the 4 hours since exposure
The triage score T is assigned as follows:
Given: N = WBC × (% neutrophils); L = WBC × (% lymphocytes); E = 0 if no emesis is present by 4 hours; E = 2 if emesis is present by 4 hours
If T is higher than 3.7, the patient should be referred for further evaluation; otherwise can be discharged with follow-up if clinically stable
Presenting Signs and Symptoms
Depending on the cause of the radiologic emergency (spill or leak versus explosion), the emergency provider may be in the position of having to stabilize and treat traumatic injuries and burns before assessing patients for signs of ARS. In cases of blast and thermal injury, patients’ traumatic injuries are of primary concern because poor outcomes after radiation injury are compounded by traumatic injury and thermal burns (e.g., combined injury).12,13
ARS has four subsyndromes—hematopoietic, gastrointestinal, cutaneous, and neurovascular—and the time until onset and severity are related to the dose for all syndromes. The hematopoietic system is most vulnerable, with at least mild changes occurring at whole-body exposure to doses of less than 1 Gy, and acute treatment is typically considered at 2 Gy and higher.4,11,14 The cutaneous, gastrointestinal, and cardiovascular subsyndromes generally occur with whole-body exposure to doses of greater than 4 Gy, greater than 6 Gy, and greater than 10 Gy, respectively.11
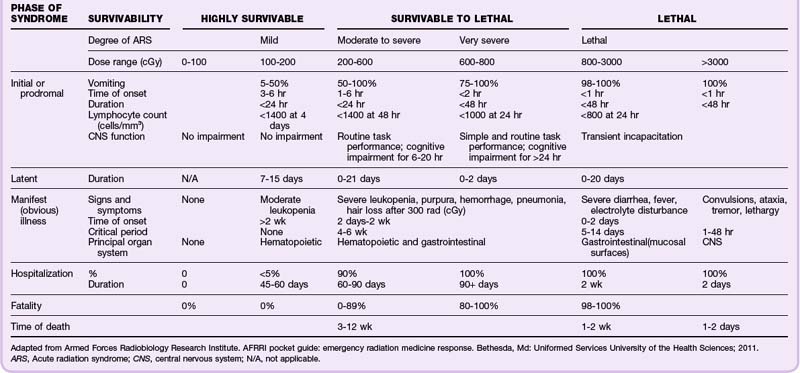
ARS and the subsyndromes typically follow four predictable phases. The first, or prodromal, phase can include the symptoms of nausea and vomiting, diarrhea, fatigue, fever, erythema, conjunctivitis, and respiratory difficulty. Altered mental status occurs in the cardiovascular subsyndrome in association with very high radiation doses (>10 Gy). This prodromal phase indicates that more serious manifestations may follow and provides important clues for triage.5,9–12,14,15 Next is the latent phase, in which the symptoms subside; it lasts days to weeks, with patients exposed to higher doses typically having shorter latency. The latent phase is followed by the manifest illness phase, in which the four ARS subsyndromes are evident and patients require intensive medical management. The final phase is eventual recovery or death (Fig. 135.1; Table 135.1).
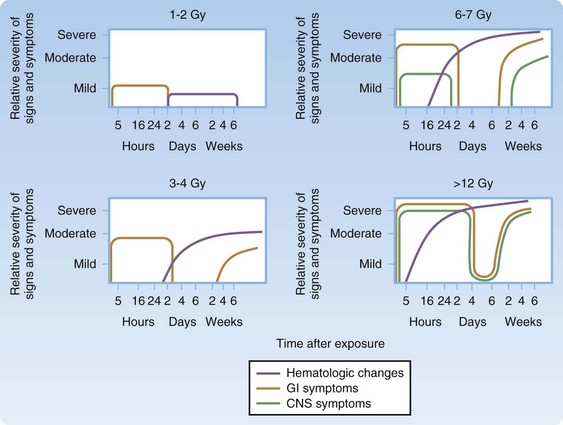
Fig. 135.1 Nature and time course of symptoms based on radiation dose.
(Adapted from Waselenko JK, MacVittie TJ, Blakely WF, et al. Medical management of the acute radiation syndrome: recommendations of the Strategic National Stockpile Radiation Working Group. Ann Intern Med 2004;40:1037-51.)
Differential Diagnosis and Medical Decision Making
Given that modern supportive care is effective in increasing LD50/60 doses (lethal dose for 50% of the population surviving at 60 days) in nontrauma patients from 3.5 to 4 Gy (without medical care) to up to 6 to 8 Gy (treated with transfusions, antibiotics, colony-stimulating factors, and intensive care), it is of the utmost importance to triage and treat patients appropriately early in the postexposure period.1,5,10,11 The goal is to provide the highest level of care possible to patients who may have had radiation exposure, are possibly contaminated, and may or may not have sustained concomitant trauma or burns.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree