Acute Pancreatitis
Ari K. Leppäniemi
I. Introduction
The annual incidence of acute pancreatitis varies between 7 and 102/100,000 population, depending on the prevalence of gallstone disease and the level of alcohol consumption. Of patients admitted for acute abdominal pain, acute pancreatitis is responsible for 3% to 4%. About 80% of the patients have the edematous or mild form of the disease that usually resolves with symptomatic treatment in a few days. The severe form, necrotizing or hemorrhagic pancreatitis, is a life-threatening condition with hospital mortality rates of 10% to 20%.
The management of severe acute pancreatitis (SAP) is resource-intensive and is associated with lengthy hospital and ICU stays, multiple interventions, and high costs. Once identified, the management of SAP follows the same principles – with some additional procedures for gallstone-induced pancreatitis – regardless of the etiology.
II. Etiology and pathogenesis
Excessive alcohol consumption and gallstone disease (passage of gallstones into the common bile duct) account for 70% to 80% of cases of acute pancreatitis. However, only a small minority of patients with symptomatic gallstone disease develop acute pancreatitis.
Rare causes of acute pancreatitis include hypercalcemia, hypertriglyceridemia, trauma, certain drugs, infections, postoperative conditions (e.g., cardiac surgery), endoscopic retrograde cholangiopancreatography (ERCP), developmental anomalies (e.g., pancreas divisum), tumors, hereditary and autoimmune diseases. In about 10% of the cases, the etiology remains unknown.
The pathogenesis of acute pancreatitis involves several steps: First, a triggering factor is needed to initiate the pancreatic acinar cell injury. Second, pancreatic proenzymes (zymogens) become activated intracellularly, resulting in acinar cell injury. This is followed by local inflammation of the pancreas resulting in activation of several inflammatory cells and release of inflammatory mediators. If this inflammation cannot be controlled locally, a systemic inflammatory response syndrome (SIRS) develops. A frequent complication of SIRS is the development of multiple organ dysfunction syndrome (MODS) characterized by impairment of the respiratory, cardiovascular, renal, hepatic, hematologic, gastrointestinal, or central nervous system.
Recently, increased intra-abdominal pressure (IAP) and the development of abdominal compartment syndrome (ACS) have been recognized as a contributor to the development of early MODS in SAP.
If the patient survives the initial inflammatory insult, a second phase usually follows 2 to 4 weeks later with the appearance of local infection, sepsis or other complications. Infection of the pancreatic and peripancreatic necrosis occurs in 20% to 40% of patients with SAP, and is associated with worsening MODS. Local complications, such as the development of pancreatic abscesses or pseudocysts, especially after non-operative management, can develop even at a later stage, 4 to 6 weeks after the initial symptoms.
Clinical presentation and diagnosis
History. Seek history of any previous episodes of acute pancreatitis and causes along with recent abdominal trauma, surgical or endoscopic procedures, new drugs, infections, and family history of acute pancreatitis. The history of alcohol abuse can be
difficult to demonstrate and often patients underestimate the amount of alcohol consumed. Acute pancreatitis can also be the first manifestation of a gallstone disease.
A typical patient complains of sudden pain in the epigastrium, often radiating into the back and feeling like a belt around the upper abdomen. The pain is more constant than colicky, and the patient may ask for strong analgesics. Nausea and vomiting are frequently seen. Fever is common in manifest disease and in patients with accompanying cholangitis.
Some patients with alcohol-induced pancreatitis have altered sensorium and cannot give an appropriate history. Interview family members or relatives to form a reliable picture of the events leading to the acute condition.
Physical examination.
Assess the vital signs and airway adequacy to guide initial care. Start crystalloid fluid resuscitation immediately if any shock (overt hypotension) exists, and consider occult or compensated shock when vital signs seem “close to normal” (mild tachycardia or low normal systolic blood pressure).
Look for abdominal distension (caused by ileus, ascites, visceral edema), and possible discolorations around the umbilicus (Cullen’s sign) or in the flanks (Grey-Turner’s sign). Palpation may reveal local (epigastric) or generalized tenderness, and ascites. Also, absence of bowel sounds suggests ileus.
Laboratory data. Serum amylase or lipase levels can be used to diagnose acute pancreatitis, but the amylase levels may have returned to normal if several days have passed from the onset of symptoms. C-reactive protein level (CRP) elevations lag 24 to 48 hours behind and can be completely normal in the initial phase of even a severe form of the disease.
Blood count, liver function tests, electrolyte, glucose, and renal function should be assessed in all to identify illness severity. In those who appear ill, arterial blood gas analysis and serum lactate measurements can aid detection of cellular hypoperfusion. Triglyceride levels should be measured, if suspected to be the cause.
Imaging
Except for those patients with potential gut obstruction or perforation, plain abdominal radiographs are not needed. Chest radiographs are used if any respiratory symptoms exist to evaluate for concomitant infection or edema.
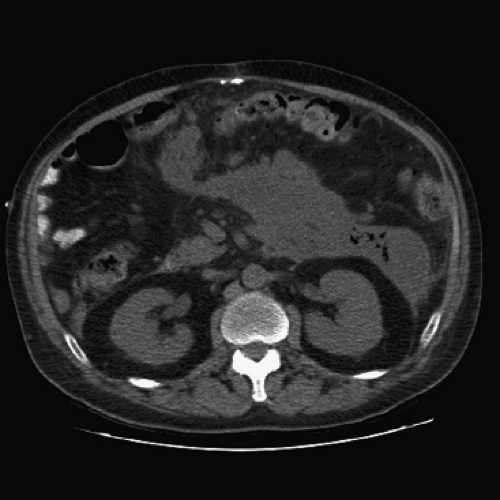
Abdominal CT is the best imaging test. Oral contrast can be used, but intravenous contrast material should be used with caution and only after confirming adequate circulating volume and urine output. A non-contrast scan provides much information and detects virtually all severe forms of acute pancreatitis.
If necrotizing pancreatitis is suspected, a later abdominal CT with intravenous contrast can be done once volume restoration and renal function are restored. If infection and necrosis are suspected (recurring CRP increase, persistent fever, worsening organ dysfunctions), gas bubbles seen in CT scan are diagnostic (Fig. 48-1).
Ultrasonography is useful to identify gallstones and a dilated common bile duct (when duct stones or cholangitis are suspected).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree