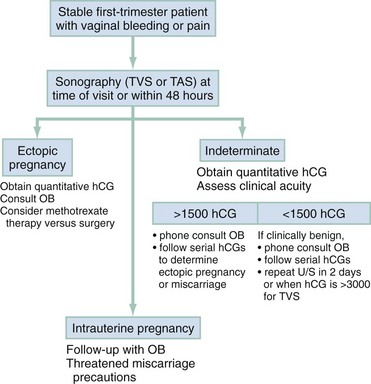
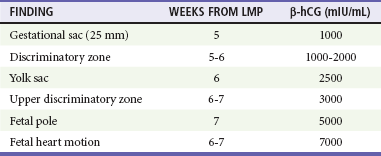
Chapter 178 Miscarriage, the most common serious complication of pregnancy, is defined as the spontaneous termination of pregnancy before 20 weeks of gestation. Fetal demise after 20 weeks of gestation or when the fetus is more than 500 g is considered premature birth. Loss of early pregnancy, defined as detection of human chorionic gonadotropin (hCG) within 6 weeks of the last normal menstrual period, occurs in approximately 20 to 30% of pregnancies.1–3 Embryonic and fetal loss after implantation occurs in up to one third of detectable pregnancies. The risk of miscarriage rises with increasing maternal age (fivefold increase in those older than 40 years compared with those 25 to 29 years), increasing paternal age, alcohol use, increased parity, history of prior miscarriage, poorly controlled diabetes mellitus and thyroid disease, low pre-pregnancy body mass index, maternal stress, and history of vaginal bleeding.4–6 Approximately 80% of miscarriages occur during the first trimester; the rest occur before 20 weeks of gestation. Threatened or actual miscarriage is a common presentation of patients in the emergency department (ED). Approximately one fourth of clinically pregnant patients experience some bleeding. It is estimated that up to 50% of all women who have bleeding during early pregnancy miscarry, although the risk is probably higher in the ED population.7,8 Patients who have a viable fetus visualized on ultrasound examination have a much lower risk of miscarriage (3-6%), although vaginal bleeding is a high-risk indicator, even when a viable fetus is present.9 Those with a history of bleeding who do not miscarry may have otherwise normal pregnancies, although they have an approximately twofold increased risk of premature birth and low-birth-weight infants.10 Pathophysiology.: The majority of miscarriages are due to either uterine malformations or chromosomal abnormalities, which account for the majority of miscarriages that occur within 10 weeks of gestation.6 In some cases the ovum never develops (anembryonic gestation). In the majority of early miscarriages, fetal death precedes clinical miscarriage, often by several weeks. Although clinical symptoms of miscarriages are most common between 8 and 12 weeks of gestation, sonographic evidence in most cases demonstrates death before 8 weeks; if fetal viability can be demonstrated by heart activity and a normal sonogram, the subsequent risk of fetal loss decreases significantly. Maternal factors that increase the risk of miscarriage include congenital anatomic defects, uterine scarring, leiomyomas, and cervical incompetence. Other conditions associated with increased miscarriage rates include toxins (e.g., alcohol, tobacco, and cocaine), autoimmune factors, endocrine disorders, including luteal phase defects, and occasional maternal infections.2–5 Terminology.: Miscarriage can be broadly categorized into three categories. The first is a threatened miscarriage, in which the patient presents with vaginal bleeding but is found to have a closed internal cervical os. The risk of miscarriage in this population is estimated at 35 to 50%, depending on the patient’s risk factors and severity of symptoms.11 If the internal cervical os is open, the miscarriage is considered inevitable. If products of conception are present at the cervical os or in the vaginal canal, the miscarriage is termed incomplete, the second classification of miscarriage. The third classification is a completed miscarriage, which occurs when the uterus has expelled all fetal and placental material, the cervix is closed, and the uterus is contracted. Establishment of the diagnosis of completed miscarriage is difficult in the ED. A gestational sac should be visualized for diagnosis because the cervix may close after an episode of heavy bleeding and clot passage without or after only partial expulsion of the products of conception. Unless an intact gestation is passed and recognized, completed miscarriage should be diagnosed only after dilation and curettage (D&C) with pathologic confirmation of gestational products, demonstration by sonography of an empty uterus with a prior known intrauterine pregnancy (IUP), or reversion to a “negative” pregnancy test result. This may take up to several weeks after the initial presentation. Any tissue that is passed should be suspended in saline or tap water (or viewed under low-power microscopy) to differentiate sloughing endometrium and organized clot from chorionic villi, which form fronds and appear feathery in the saline suspension. Except in the rare instance of heterotopic pregnancy (combined intrauterine and ectopic pregnancies), this reliably excludes ectopic pregnancy. Passage of tissue called the decidual cast in ectopic pregnancy can easily be confused with intrauterine miscarriage if the physician does not confirm the absence of chorionic villi in the tissue.12 A hemoglobin level is useful to provide a baseline measurement and to evaluate the degree of blood loss in women whose bleeding persists. In addition, an Rh type should be obtained. Ultrasonography is the primary means of evaluating the health of the fetus as well as its location (Table 178-1). Because historical and clinical estimations of gestational age are often inaccurate, ultrasonography is useful to provide an accurate measure of fetal age and viability (Box 178-1). Table 178-1 Landmarks for Gestational Age and β-hCG Level by Transvaginal Ultrasonography β-hCG, beta subunit of human chorionic gonadotropin; LMP, last menstrual period. Modified from Ramsey E, Shilitto J: How early can fetal heart pulsations be detected reliably using modern ultrasound equipment? Ultrasound 16:193-195, 2008. In the stable patient with threatened miscarriage, expectant management may be sufficient to determine when intervention is needed as long as ectopic pregnancy has been excluded. Serial quantitative hCG levels are used to assess the health of the fetus if sonographic findings are indeterminate or if the gestational age is less than 6 or 7 weeks. The sonographic “discriminatory zone” is defined as the quantitative hCG level at which a normally developing IUP should reliably be seen. This is considered to be 6500 mIU/mL for transabdominal ultrasonography and 1000 to 2000 mIU/mL for transvaginal ultrasonography.13 Ultrasonography can be performed or repeated when hCG levels rise to 1500 to 3000 mIU/mL. If hCG levels are flat or decline or if sonographic criteria for fetal demise are demonstrated (see Box 178-1), the patient should be referred to an obstetrician for follow-up to ensure miscarriage completion and to rule out subsequent complications. Ectopic pregnancy can masquerade as a threatened miscarriage in the early stages of pregnancy and should always be considered in the differential diagnosis. Even in the patient with painless vaginal bleeding, the diagnosis of ectopic pregnancy must be considered.12 Thus early ultrasonography is imperative to locate the pregnancy in the patient who has bleeding or pain. After assessment of hemodynamic status and management of blood loss, a patient with a threatened miscarriage requires very little specific medical treatment. Anti-D immune globulin should be administered if the patient is Rh negative (unless the father is also known to be Rh negative). A 50-µg dose is used during the first trimester and a full 300-µg dose after the first trimester.14 Once ectopic pregnancy has been excluded, ultrasonography can be scheduled more routinely at a later time in the patient without significant pain as long as the patient is aware that the potential for ectopic pregnancy exists until it is excluded by identification of an IUP. In the patient who is planning pregnancy termination, prompt referral should be encouraged and chorionic villi confirmed at the time of uterine evacuation. Unless an IUP is diagnosed, the patient with threatened miscarriage should be given careful instructions on discharge to return if she has signs of hemodynamic instability, significant pain, or other symptoms that might indicate ectopic pregnancy (so-called ectopic precautions). In conjunction with gynecologic colleagues, an ED protocol is useful to determine when follow-up sonographic evaluation and serial hCG measurements should be obtained as ultrasonography can be an inaccurate diagnostic tool if the hCG level is significantly low, if vaginal bleeding is significant, or if ultrasonographic findings do not include a fetal pole or yolk sac.15 Patient counseling is paramount with threatened miscarriage.16,17 Determination of fetal viability can be helpful in either reassuring the mother or preparing her for probable fetal loss. Miscarriages are associated with a significant grieving process, which is frequently more difficult because early pregnancy is unannounced and early fetal death is not publicly recognized. Because many women consider that small falls, injuries, or stress during the first trimester can precipitate miscarriage, patients should be reassured that they have done nothing to cause miscarriage. It is important to make them aware that miscarriage is common, grieving is normal, and counseling may be beneficial.18,19 A follow-up appointment should be scheduled after miscarriage to support the patient in resolving such issues. Treatment of the patient with incomplete miscarriage includes expectant management, medical management with misoprostol, or surgical evacuation.18,20 When the miscarriage is incomplete, the uterus may be unable to contract adequately to limit bleeding from the implantation site. Bleeding may be brisk, and gentle removal of fetal tissue from the cervical os with ring forceps during the pelvic examination often slows bleeding considerably. Management of patients with presumed completed miscarriage is more complicated. If the patient brings tissue with her, this should be sent to the pathology department for evaluation. Unless an intact gestational sac or fetus is visualized, it is rarely clear clinically whether miscarriage is “complete.” Studies have shown that in women with a history consistent with miscarriage who have minimal remaining intrauterine tissue as determined by ultrasonography, expectant management is safe, but only if ectopic pregnancy can be excluded.20 If endometrial tissue is not seen with ultrasonography, bleeding is mild, and gestational age is less than 8 weeks, curettage is frequently unnecessary and the patient can be safely observed by a gynecologist for serial hormonal assays. Up to 80% of women with first-trimester miscarriage complete the miscarriage without intervention.21 However, the need for later visits and procedures may be decreased by uterine curettage, particularly if the fetal pole or a gestational sac is visible on the sonogram at the time of evaluation.20 Medical management with misoprostol instead of D&C is also an option and has a success rate of up to 96%.18,22,23 The patient should be instructed to return if uncontrolled bleeding, severe pain or cramping, fever, or tissue passage occurs. Follow-up is recommended in 1 or 2 weeks to ensure that the miscarriage is complete. After miscarriage, the patient should be advised that fetal loss, even during the first trimester, can cause significant psychological stress.16 Follow-up in 1 or 2 weeks with a gynecologist should be provided. Some physicians prescribe antibiotics after D&C (usually doxycycline or metronidazole), particularly in populations of patients at high risk for genital tract infections. Ergonovine or methylergonovine (0.2 mg orally twice daily) can be used to stimulate uterine involution. The patient should be advised to return if signs of infection (fever or uterine tenderness) occur, if bleeding resumes, or if further tissue is passed. Ectopic pregnancy, or pregnancy implanted outside the uterus, is an increasingly frequent problem that poses a major health risk to women during the childbearing years. It is the third leading cause of maternal death, responsible for 6% of maternal mortality.24 The incidence of ectopic pregnancy has risen steadily during several decades and now accounts for approximately 2% of all pregnancies. Although the incidence of ectopic pregnancy is highest in women aged 25 to 34 years, the rate is highest among older women and women belonging to minority groups. Simultaneous intrauterine and extrauterine gestations (heterotopic pregnancy) have historically been rare, occurring in approximately 1 in 4000 pregnancies; more recently, women who have undergone assisted reproduction techniques with embryo transfer have demonstrated a risk of one of the pregnancies being ectopic of 4% or greater. The incidence of ectopic pregnancy among women presenting to the ED with vaginal bleeding or pain in the first trimester is consistently approximately 10% in several series.25,26 Implantation of the fertilized ovum occurs approximately 8 or 9 days after ovulation. Risk factors for an abnormal site of implantation include prior tubal infection (50% of cases), anatomic abnormalities of the fallopian tubes, and abnormal endometrium (host factors). These result in failure of the embryo to implant in the endometrium. The risk of ectopic pregnancy increases approximately threefold after a patient has had pelvic inflammatory disease (PID). In recent studies, one fourth of patients with ectopic pregnancies have had tubal surgery, including tubal sterilization or removal of ectopic pregnancy.27 If the patient is currently using an intrauterine device, increased risk can occur from complicating PID or from failure of the intrauterine device to prevent pregnancy while preventing endometrial implantation. All forms of contraception except the intrauterine device and tubal sterilization decrease the incidence of ectopic pregnancy. After an ectopic pregnancy, the risk of a subsequent ectopic pregnancy was 22% in one series of women trying to conceive again (Box 178-2).28 The classic clinical picture of ectopic pregnancy is a history of delayed menses, followed by abdominal pain and vaginal bleeding in a patient with known risk factors. Unfortunately, this history is neither sensitive nor specific. Risk factors for ectopic pregnancy are absent in almost half of patients. Fifteen percent to 20% of patients with symptomatic ectopic pregnancy have not missed a menstrual period, and occasionally the patient has no history of vaginal bleeding. Abdominal pain is most commonly severe, peritoneal in nature, and constant. Shoulder pain implies free fluid in the peritoneal cavity and is suggestive of an ectopic pregnancy with significant hemorrhage. The pain of ectopic pregnancy can also be crampy, intermittent, or even absent.12,29 The physical examination findings in ectopic pregnancy are likewise variable. Vaginal bleeding, uterine or adnexal tenderness, or both in the patient with a positive pregnancy test result should trigger consideration of ectopic pregnancy. Tachycardia is not always present, even with significant hemoperitoneum; hemoglobin level is usually normal, and hypotension may be seen.29 The presence of peritoneal signs, cervical motion tenderness, or lateral or bilateral abdominal or pelvic tenderness indicates increased likelihood of an ectopic pregnancy. If significant peritoneal irritation is present, pain can preclude accurate bimanual examination. Adnexal masses are felt in only 10 to 20% of patients with ectopic pregnancy.12,29 Vaginal bleeding is often mild. Heavy bleeding with clots or tissue usually suggests a threatened or incomplete miscarriage, although the patient with an ectopic pregnancy who has decreasing hormonal levels may experience endometrial sloughing, which can be mistaken for passage of fetal tissue. Passed tissue should be examined, as with cases of miscarriage, in tap water or saline (or under low-power microscopy). Unless fetal parts or chorionic villi are seen, ectopic pregnancy should not be excluded in the patient with bleeding or passage of “tissue.” Ultrasonography.: Ultrasonography is the primary method used to locate early gestation, to establish gestational age, and to assess fetal viability. Transabdominal ultrasonography is most useful for identification of IUPs with fetal heart activity and exclusion of ectopic pregnancy (except in patients at high risk for heterotopic pregnancy because of infertility procedures).13 Transvaginal ultrasonography is more sensitive, recognizes IUP earlier than transabdominal ultrasonography does, and is diagnostic in up to 80% of stable patients presenting in the first trimester.30 Sonographic findings in the patient with suspected ectopic pregnancy are listed in Box 178-3 and illustrated in Figures 178-1 to 178-5. In general, an indeterminate ultrasound study usually does not result in a diagnosis of normal pregnancy; one series of more than 1000 pelvic ultrasound examinations reported that 53% of indeterminate ultrasound studies resulted in a diagnosis of embryonic demise, 15% were ectopic pregnancies, and only 29% had an IUP.31 However, correlation of sonographic results with quantitative hCG measurements can add to the predictive value.32 With hCG levels of less than 1000 mIU/mL, the risk of ectopic pregnancy increases fourfold; ultrasonography is still diagnostic in a significant minority of patients (one third of patients with ectopic pregnancy), although the accuracy of sonographic findings may decrease.31 Normal pregnancy is unlikely if no gestational sac is seen by transvaginal ultrasonography with an hCG level higher than 1000 to 2000 mIU/mL, depending on the institution’s discriminatory zone, but the differential diagnosis includes both miscarriage and ectopic pregnancy. Unfortunately, levels of approximately 1500 mIU/mL develop in only approximately half of patients with ectopic pregnancies (see Table 178-1).8,13 Figure 178-1 Pregnancy in the fallopian tube, diagnostic of an ectopic pregnancy. (Courtesy Mary Ann Edens, MD.) Figure 178-4 Ultrasonography showing fluid around the fallopian tube. (Courtesy Mary Ann Edens, MD.) Indeterminate sonograms, which demonstrate neither an IUP nor extrauterine findings suggestive of ectopic pregnancy, occur in approximately 20% of ED evaluations of women with first-trimester bleeding or pain. Ectopic pregnancy is more likely among this subgroup with indeterminate sonograms if the hCG level is less than 1000 mIU/mL and when the uterus is empty. Endometrial debris and fluid in the uterus do not exclude ectopic pregnancy.33 Use of bedside ultrasonography in the ED for the diagnosis of IUP and the exclusion of ectopic pregnancy has shown good sensitivity and negative predictive value in ruling out ectopic pregnancy, but it requires significant operator training.34–38 In addition to operator-based limitations, it is also limited by device availability and quality within the ED. Hormonal Assays.: The quantitative hCG levels have two primary uses: serial levels can be used in the stable patient who can be observed as an outpatient, and a single level can be correlated with sonographic results for improved interpretation. Serum hCG levels normally double every 1.8 to 3 days for the first 6 or 7 weeks of pregnancy, beginning 8 or 9 days after ovulation. An initial quantitative level can be measured at the time of the ED visit, particularly if the sonogram is indeterminate or the gestational age is estimated as less than 6 weeks. A repeated level should be measured 48 to 72 hours later. Levels that fall or rise slowly are associated with abnormal pregnancy, either intrauterine or ectopic. Twenty-one percent of women with an ectopic pregnancy in one series had an initial rise in hCG at a rate consistent with an IUP.36 Single quantitative hCG levels can also be useful in conjunction with ultrasonography; normal IUPs should be visible transvaginally at 1000 to 2000 mIU/mL hCG or higher (see Table 178-1). A benign course for ectopic pregnancy cannot be assumed with low hCG levels; ruptured ectopic pregnancies requiring surgery have been reported with very low or absent levels of hCG.39 Other Ancillary Studies.: Dilation and evacuation can be used in patients without a viable IUP or ectopic pregnancy on ultrasonography to differentiate intrauterine miscarriage from ectopic pregnancy. Identification of chorionic villi in endometrial samples is seen in approximately 70% of patients and excludes ectopic pregnancy (except in infertility patients). Identification of chorionic villi can be made even in 50% of women with an empty uterus on ultrasonography and limits the need for laparoscopy to exclude ectopic pregnancy in this population.40 Although it is invasive, laparoscopy is extremely accurate as a diagnostic (and therapeutic) procedure for possible ectopic pregnancy. It is the diagnostic treatment of choice in the unstable first-trimester patient with frank peritoneal signs and is also indicated in patients with significant peritoneal fluid or an ectopic gestation in the pelvic cavity. Medical alternatives for management of ectopic pregnancy have resulted in decreased indications in stable patients.32,41 A ruptured corpus luteum cyst should also be considered in the patient who has first-trimester bleeding associated with peritoneal pain or irritation. The corpus luteum normally supports the pregnancy during the first 7 or 8 weeks. Rupture causes pelvic pain and peritoneal irritation. Ultrasonography is helpful if it reveals an IUP (except in patients with in vitro fertilization). During early gestation, when ultrasonography is nondiagnostic, free fluid is usually visible by ultrasonography, and serial observation may be required (see Fig. 178-4). If the patient is unstable (especially if an IUP cannot be identified by ultrasonography), laparoscopy or, rarely, laparotomy may be required to differentiate between the two conditions. Classically, approximately 20% of women with ectopic pregnancies manifest signs and symptoms warranting immediate intervention.41 This includes patients with significant hypovolemia, large amounts of peritoneal fluid, or an open cervical os. For patients with significant signs of hypovolemia, rapid volume resuscitation should be instituted with intravenous fluids and blood products as necessary, and a baseline hemoglobin level and type and crossmatch should be obtained. A D&C or evacuation procedure with examination of endometrial contents for products of conception can be performed urgently in the unstable patient with an open cervical os. If the patient remains unstable, immediate surgery is warranted. Laparoscopy may be indicated for patients who stabilize with treatment or for those who are hemodynamically stable but exhibit significant peritoneal signs. One study reported that identification of free fluid in Morison’s pouch on bedside ultrasonography predicted the need for operative intervention in the majority of cases in patients with suspected ectopic pregnancies.26 All patients with ectopic pregnancy who are Rh negative should be given Rh immune globulin 50 µg intramuscularly, unless the father is known to be Rh negative. In low-risk patients with only minor symptoms or bleeding, ectopic pregnancy is still a possibility. Two general outpatient approaches can be considered. In most institutions, ultrasonography is the initial screening tool (Fig. 178-6). If an IUP is not seen, quantitative hCG levels help stratify patients by risk. In all cases, if the patient is discharged, careful instructions are given for symptoms that would require her earlier return (ectopic precautions). An alternative strategy uses hCG levels first. However, waiting times for the serum assay can increase ED length of stay. In addition, ultrasonography is usually diagnostic of IUP or ectopic pregnancy, even if the hCG level is less than 1000 mIU/mL.29,30 In most hands, the initial sonogram provides more rapid and accurate information. A significant minority of patients have indeterminate sonographic results and hCG levels below 1000 mIU/mL. When the hCG levels never rise to the discriminatory zone, the differential diagnosis includes intrauterine fetal demise and ectopic pregnancy. Early D&C with identification of products of conception can be useful in the patient with nonrising hCG levels to detect chorionic villi and to confirm a failed IUP or to strongly suggest ectopic pregnancy.40 Alternatively, hCG levels can be followed until they reach zero, particularly if initial levels are low. Although laparotomy may be required for patients who have ectopic pregnancies, an increasing number of surgeries are being performed through the laparoscope. Salpingostomy is preferred to salpingectomy if the patient is stable and the procedure is technically feasible. Overall, the advent of transvaginal ultrasonography has resulted in a decreased number of surgeries and a trend toward nonoperative management.42 Medical management has become standard in many areas for the stable patient with minimal symptoms and is cost-effective when subsequent fertility is being considered.41 Methotrexate is the drug most commonly used to treat early ectopic pregnancy. It causes destruction of rapidly dividing fetal cells and involution of the pregnancy. Medical treatment is most often used for patients who are hemodynamically stable with a tubal mass smaller than 3.5 cm in diameter, no fetal cardiac activity, and no sonographic evidence of rupture. Although there is no agreed on cutoff for single-dose methotrexate, a systematic review found that patients with an hCG level above 5000 mIU/mL had an increased failure rate.43 Medical therapies are associated with an 85 to 93% success rate, with no significant difference between single- and multiple-dose protocols.44 Pelvic pain is common (60%) in patients receiving methotrexate, even when it is used successfully.45 Indications of methotrexate failure and need for rescue surgery include decreasing hemoglobin levels, significant pelvic fluid, and unstable vital signs. All patients receiving methotrexate require close follow-up until the hCG level reaches zero, which may take 2 or 3 months. Molar pregnancy, also known as gestational trophoblastic disease, comprises a spectrum of diseases characterized by disordered proliferation of chorionic villi. In the absence of fetal tissue, the pregnancy is termed a complete hydatidiform mole. More rarely, if fetal tissue is present and trophoblastic hyperplasia is focal, it is called an incomplete mole. In approximately 19% of molar pregnancies, neoplastic gestational disease develops, with persistence of molar tissue after the pregnancy has been evacuated.46,47 Metastatic disease can develop, requiring chemotherapy and intensive oncologic management. Early molar pregnancy is usually not clinically apparent. The most well described risk factor for development of a molar pregnancy is extremes of maternal age.48 Many patients present with abdominal pain, nausea and vomiting, or vaginal bleeding, and it may be difficult to differentiate these patients from those with threatened miscarriage or ectopic pregnancy by historical features alone.49 Patients sometimes seek treatment for apparent persistent hyperemesis gravidarum from high circulating levels of hCG, bleeding or intermittent bloody discharge, or respiratory distress; failure to hear fetal heart tones during the second trimester is the usual initial clue to diagnosis.50,51 If molar pregnancy spontaneously aborts, it is usually in the second trimester (before 20 weeks), and the patient or physician may note passage of grapelike hydatid vesicles. Uterine size is larger than expected by date (by more than 4 weeks) in approximately 30 to 40% of patients. Theca lutein cysts may be present on the ovaries as a result of excessive hormonal stimulation, and torsion of affected ovaries can be seen.50,51 The diagnosis of hydatidiform mole is based on the characteristic sonographic appearance of hydropic vesicles within the uterus, described as a “snowstorm” appearance (Fig. 178-7). Alternatively, cystic changes are seen in partial molar pregnancies. In some cases, partial molar pregnancy is detected only on pathologic examination of abortion specimens.52 Complications of molar pregnancy include preeclampsia or eclampsia (which can develop before 24 weeks of gestation), pulmonary embolization of trophoblastic cells, hyperemesis gravidarum, and significant uterine bleeding, either acute or chronic. Ultrasonography usually provides the diagnosis of complete molar pregnancy, either in the second-trimester patient who has “threatened miscarriage” or during sonographic assessment for fetal well-being and size. However, ultrasonography is only 58% sensitive, and diagnosis of partial mole is made in 17% of cases.52 Up to two thirds of molar pregnancies are diagnosed by pathologic specimens after miscarriage.52 Vaginal Bleeding in Later Pregnancy Bleeding during the second trimester before the fetus is potentially viable (14-24 weeks) is not benign. One third of fetuses are ultimately lost when maternal bleeding occurs. Management is supportive and expectant because fetal rescue is impossible at this level of fetal immaturity. In the third trimester, vaginal bleeding is still associated with significant morbidity in approximately one third of women, but the treatment includes consideration of urgent delivery.53 Principles of Disease.: Abruptio placentae, or separation of the placenta from the uterine wall, is believed to account for approximately 30% of episodes of bleeding during the second half of pregnancy. In addition, small subclinical or marginal separations may go undetected until the placenta is examined at delivery and probably account for many of the other self-limited episodes of bleeding for which no diagnosis is made. In cases of nontraumatic abruptio placentae, apparently spontaneous hemorrhage into the decidua basalis occurs, causing separation and compression of the adjacent placenta. Small amounts of bleeding may be asymptomatic and remain undetected until delivery. In other instances, the hematoma expands and extends the dissection; bleeding may be concealed or may be clinically apparent if dissection occurs along the uterine wall and through the cervix. Placental separation can be acute or an indolent problem throughout late pregnancy. Abruptio placentae is most clearly associated with maternal hypertension and preeclampsia; it is also more common with increasing maternal age and parity, history of smoking, thrombophilia, prior miscarriage, prior abruptio placentae, and cocaine use.53,54 Placental separation can also be associated with blunt trauma to the abdomen. In such instances, the cause appears to be shearing of a nonelastic placenta from the easily distorted elastic uterine wall at the time of traumatic impact. Women who reported physical violence during pregnancy were twice as likely as women who did not report violence to have an abruption.55
Acute Complications of Pregnancy
Problems in Early Pregnancy
Perspective
Principles of Disease
Clinical Features
Diagnostic Strategies
Differential Considerations
Management
Ectopic Pregnancy
Principles of Disease
Clinical Features
Diagnostic Strategies


Differential Considerations
Management
Molar Pregnancy
Complications of Late Pregnancy
Perspective
Abruptio Placentae
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Acute Complications of Pregnancy
Only gold members can continue reading. Log In or Register to continue