Fig. 84.1
Axial CT with arterial phase imaging demonstrates an intact left superficial femoral artery (SFA) without evidence of filling abnormality
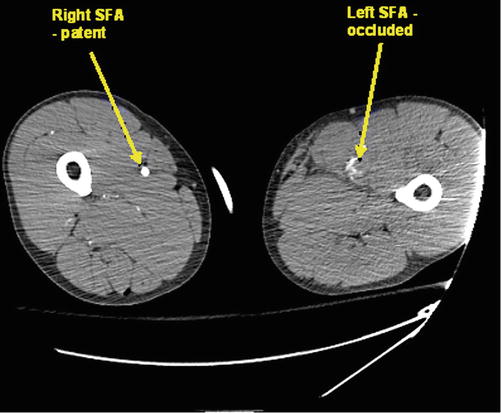
Fig. 84.2
Axial CT demonstrates occlusion of the left SFA in the more distal extremity. Note the normal, patent right SFA
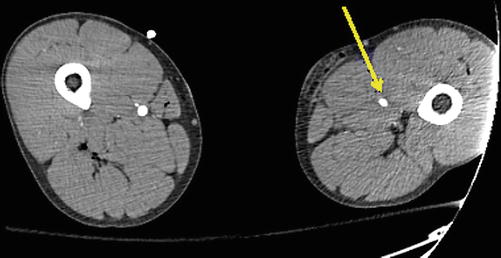
Fig. 84.3
Axial CT from the mid-distal thigh demonstrates an intact left SFA just caudal to the occluded segment without evidence of filling defect
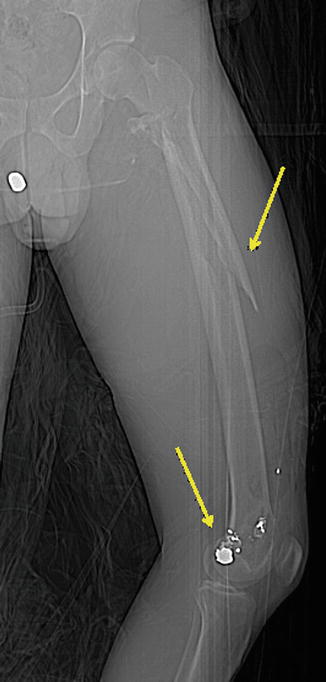
Fig. 84.4
Ballistic fracture of left femur with pelvic and knee foreign bodies
Question
What is the diagnosis and what is the next step in management?
Answer
Acute limb ischemia secondary to high velocity penetrating trauma. Consider the merits of immediate bone fixation versus a revascularization first approach. Consultation to Vascular Surgery and Orthopedic Surgery at an early juncture may facilitate an optimal multidisciplinary approach in order appropriately sequence reperfusion and musculoskeletal fixation.
The CTA demonstrated a left SFA injury with segmental thrombosis but no active extravasation. Vascular Surgery and Orthopedic Surgery were consulted. In the operating room, the patient was hemodynamically stable. The ischemic time at operation was approximately 4.5 h. A decision was made to locally explore the wound, obtain proximal and distal vascular control, and then place an intraoperative vascular shunt while the orthopedic surgeons performed an external fixation of the femur (Fig. 84.5). After completion of the femur fixation, saphenous vein from the contralateral leg was harvested and reversed. An interposition reversed great saphenous vein reconstruction was then performed for definitive vascular reconstruction. Four compartment fasciotomies were next performed to limit potential for compartment syndrome given the ischemic time. The patient was subsequently admitted to the intensive care unit with hourly neurovascular checks ensuring that Doppler signals were present. The patient recovered and arterial brachial index (ABI) obtained prior to discharge was 1.09 on the right and 1.08 on the left.
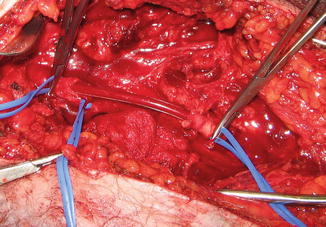
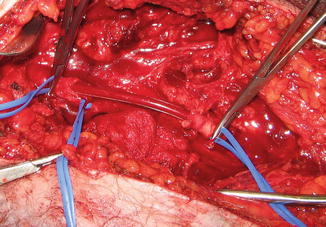
Fig. 84.5
This example of in-line arterial shunting using a 12 French carotid bypass shunt (Bard®) demonstrates tension on silastic loops for proximal and distal fixation of the shunt. This restores arterial inflow to the ischemia extremity immediately, and definitive vascular reconstruction can be performed after bony stabilization. The ballistic cavity is easily seen
Principles of Management
Initial Evaluation
When there are hard signs of vascular injury including active hemorrhage, rapidly expanding hematoma, absent pulses or a palpable thrill/bruit, immediate operative exploration is warranted. Patients who present without these signs, however, should undergo complete physical exam with special attention to the vascular exam. Physical exam in conjunction with arterial pressure index measurement by Doppler has high sensitivity for injury [1, 2]. As such, patients with lower extremity trauma should also undergo arterial pressure indices in which the Doppler pressure for the affected extremity distal to the presumed injury site is indexed to the higher of the two upper extremity arterial Doppler pressures. In the setting of a normal physical exam and pressure index >0.9, patients may be observed and/or discharged home safely with follow up [3]. Those patients who have either an abnormal physical exam and/or ankle-brachial index (ABI) <0.9 should have further imaging.
Diagnostic Imaging
CT angiography (CTA) has mostly replaced catheter angiography for the primary modality of diagnostic imaging in lower extremity trauma. Many recent studies have found the sensitivity and specificity of CTA approach 100 % [4, 5]. Catheter angiography is still considered as an additional technique when the CTA is not diagnostic, when an overabundance of metal hardware renders image quality inferior due to scatter artifact, or when endovascular intervention is considered highly likely following the diagnostic portion of the procedure.
Intervention and Post-operative Management
Intervention includes open exploration of the wound after obtaining proximal and distal control. Temporary balloon occlusion for proximal control using endovascular techniques is more commonly employed in contemporary practice, especially for injuries approaching the junctional region (groin). It is important to prep both extremities in the operating room for potential vein harvest from the unaffected limb.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







