Acute Anorectal Pain
Frederick J. Denstman
I. Introduction
The most common causes of anal pain are fissure, hemorrhoidal thrombosis, and infection. Most patients afflicted by one of these lesions presents with a chief complaint of “rectal pain.” The key first step in the history taking process is garnering a more precise description of the pain and its location.
Most etiologies of anal pain can be diagnosed on the history coupled with a simple examination, which generally consists of inspection and palpation. Anal pain should never be dismissed as being due to hemorrhoids without a diligent exam.
Only a few simple instruments are required for the diagnosis and treatment of most acute cases of anorectal pain. Many colon and rectal surgeons employ a proctology table which allows examination in the prone jackknife position. Although ideal, these tables are seldom available in most emergency departments, and a standard examination table with a decubitus positioned patient is adequate. A good examination light is imperative and this need be little more than the light provided by a 60 W light bulb. Although anoscopes and rigid sigmoidoscopes should be available in the emergency room and acute care clinic, it should be stressed that in most patients with severe anal or rectal pain, endoscopy is usually unnecessary for arrival at the correct diagnosis and often causes avoidable discomfort for the patient.
Lidocaine ointment 5% is an excellent topical agent. For infiltration, lidocaine 0.5% with epinephrine is an excellent choice for local anesthesia. Some practitioners will mix this with bicarbonate solution to decrease the acidity of the lidocaine and therefore the pain of injection. Bupivacaine 0.25% can also be mixed with the lidocaine or used alone or after initial anesthesia to extend the duration of relief.
To deliver the local anesthesia, a 1 cc or 3 cc syringe with a 21 or 22 gauge needle with which to draw up local anesthesia is adequate. A 27 or 30 gauge needle is sufficient to inject the local anesthesia; injection with a 25 gauge needle is painful. A larger gauge needle, such as a 16 gauge, is excellent for aspiration of a suspected site of abscess.
II. Anatomy
The rectum and anus are specialized segments of the gastrointestinal tract. The rectum functions primarily as a reservoir for stool. The rectosigmoid junction is marked by the merging of the taenia coli into the complete layer of longitudinal muscularis propria of the rectum. This junction is easily defined during laparotomy but can only be estimated during endoscopy. The distance between anal verge and rectosigmoid junction varies over a fairly wide range from patient to patient, from approximately 12 to 16 cm.
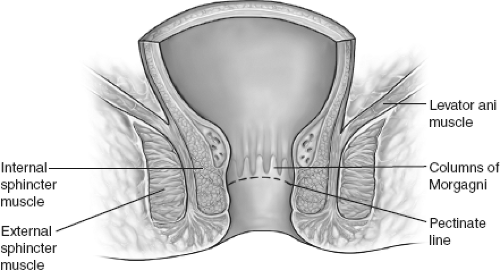
The surgical rectum ends at the level of the puborectalis muscle, which marks the hiatus through the levator ani muscles. This hiatus is palpable during digital rectal examination as the anorectal ring. The anal canal begins at the anorectal ring and extends to the anal verge. It is embraced by the anal sphincter muscles. The dentate line (pectinate line) is the line between mucosa and skin and is located several centimeters proximally within the canal. The skin immediately distal to this line is the anoderm. The anoderm is a modified squamous epithelium, containing no accessory glands. The anoderm is exquisitely sensitive to pain, whereas the anal mucosa is relatively insensitive. The anal verge marks the junction between the
anoderm and normal skin. This is easily identified by the appearance of hair-bearing skin.
Hemorrhoids are normal anatomic structures surrounding the anus. This collection of arteries and veins forms an anal cushion and is thought to participate in the mechanism of fecal continence. The vessels proximal to the dentate line or mucocutaneous border and covered by mucosa are called internal hemorrhoids. Those vessels distal to the dentate line and covered by anoderm are called external hemorrhoids. These vessels are supported by surrounding connective tissue. Degeneration of this supporting connective tissue seems to be a common pathway to the development of hemorrhoidal disease.
III. Fissure
Anal fissure is the most common cause of acute anal pain. When asked to describe the pain from a fissure, most patients will use terms such as “sharp,” “cutting,” or “it feels like something tore.” The pain usually is brought on by a bowel movement, but often the pain becomes most severe immediately following the movement and persists for 5 to 10 minutes. Occasionally it is constant or increased by sitting.
When asked, most patients will describe minor anal bleeding, usually on the toilet tissue, streaking the outside of the stool or occasionally dripping into the bowl. Patients will occasionally ascribe the pain to a swelling, but unlike the swelling described for hemorrhoids or abscesses, this swelling is usually chronic and small. The swelling is in fact not the exact site of the pain but is a sentinel skin tag. A sentinel tag is a small, firm mound of anoderm, which is adjacent but distal to the actual fissure. The tag itself is not painful. Removing the tag alone will not cure the pain, and in fact may make the fissure worse.
Fissures are typically classified as either acute or chronic, although many patients will have features of both. The typical acute fissure occurs following some excessive wear and tear on the anoderm, which is the sensitive ring of skin that extends from the dentate line to the anal verge. This is usually a hard, forceful bowel movement, although multiple loose stools over a short period of time (e.g., following colonoscopy bowel prep) can have an equally harmful effect. Patients with irritable bowel syndrome are prone to multiple, acute anal fissures. In an otherwise normal anal canal, an acute fissure will heal in a day or two. These acute fissures are usually superficial, narrow and linear, resembling a paper cut.
In patients with chronic fissure, the fissure fails to heal. Excessively high tone in the internal anal sphincter muscle is the accepted etiology of the chronic fissure, and this is thought to act by decreasing blood flow to the anoderm. As the fissure
matures, it becomes deeper and wider, eventually exposing the fibers of the internal sphincter muscle. The classic picture of the chronic fissure is completed by the development of a sentinel tag and an adjacent enlarged anal papillae, although these two additional features need not be present for the diagnosis.
Many patients seem to have a subacute syndrome, with overlapping features of both acute and chronic fissure. Their pain is characterized by good weeks and bad weeks. The fissure becomes relatively asymptomatic as it covered by a thin layer of immature scar, only to be split open again by a difficult bowel movement. This pattern of alternating severe pain and relief persists over a course of months. Even though these patients may present with acute pain, these fissures are best treated as chronic fissures.
Occasionally the fissures become infected. This usually occurs as a result of incomplete healing of the fissure, such that a hood of skin forms over the fissure and traps stool particles beneath. These lesions are more practically treated as infections than fissures in the acute setting (vide infra).
Diagnosis. In most cases, a careful history suggests the diagnosis, which can be verified on physical examination. Typical anal fissures are located in either the posterior or anterior midline. Since fissures reside in the anoderm, the most superficial aspect of the anal canal, an anoscope is usually not required to make this diagnosis, and insertion of an examining finger or anoscope may be painful and unnecessary. The anoderm can usually be well visualized by simply spreading the buttocks apart.
The acute fissure is usually superficial and linear. The classic chronic fissure is a tear-drop shaped ulceration of the anoderm, with an associated “sentinel tag” on its distal end and a hypertrophied papilla on its proximal end. The transversely oriented fibers of the internal sphincter may or may not be visible within the bed of the chronic fissure. The sphincter is not visible in an acute fissure. As stated, patients can sometimes manifest features of both acute and chronic fissures.
Once a typical midline fissure is visualized, no further immediate diagnostic maneuvers are required. If no fissure is visualized, proceed with a gentle digital examination. If the examination fails to evoke tenderness, anoscopy can be performed. If anoscopy is negative, assume the patient had an acute fissure, which has healed. If digital examination is tender in the absence of a visible fissure, rule this out as a diagnostic consideration and move down the list of differential diagnoses.
If the fissure is located well off the midline, this is referred to as an atypical fissure, and this must be noted as such because it may have special diagnostic and therapeutic significance.
Treatment. By definition, an acute fissure should heal after the precipitating problems with bowel habit are corrected. This is usually a matter of prescribing a better diet for the patient, including more fiber, water or a bulk laxative. Constipating medications, such as narcotics, should be avoided when possible. An antidiarrheal medication may be helpful in patients with chronic loose stools.
To treat the acute pain, topical anesthetic in the form of 5% lidocaine ointment is helpful. The patient places one inch of the ointment into the anal canal by fingertip about 5 minutes before a bowel movement. This will usually provide good pain relief while waiting for the fissure to heal.
With proper diet, most acute fissures, and even some chronic fissures will heal. However if healing does not occur within 3 to 4 weeks of good conservative management, additional treatment may be required. The standard for treatment of chronic fissure is a partial, lateral internal sphincterotomy. This surgical treatment has the advantage of a rapid and lasting relief of symptoms in 95% of patients.
Several topical medications are potential alternatives to sphincterotomy. These include injectable botulinum toxin and ointment formulations of 0.2% nitroglycerin, 2% diltiazem, or 0.3% nifedipine applied twice daily. These treatments avoid division of the internal sphincter but tend to be disappointing because they are temporary or incomplete.
Atypical fissure. Fissures located well off the midline are called atypical fissures. Occasionally patients with diarrhea will develop multiple, very superficial
fissures related to excessive bowel movements and wiping. This type of atypical fissure usually will heal spontaneously.
Solitary atypical fissures that do not heal quickly are a reason for concern. The differential diagnosis includes squamous cell carcinoma of the anus, Crohn’s disease, and syphilis. Many patients with Crohn’s will already carry a diagnosis. Even for the undiagnosed Crohn’s patient, there will usually be other signs or symptoms of the disease. However, there are rare patients whose initial presentation consists only of a painful, persistent atypical fissure. Squamous cell carcinoma of the anus can present as a small fissure. These early cancers tend to be extremely painful. As the disease progresses, the lesion takes on the more typical appearance of an ulcerated, hard mass. Diagnosis requires biopsy. At their earliest presentation these cancers are difficult to diagnose and may resemble typical fissures.
IV. Hemorrhoids
Thrombosis of external hemorrhoids
External hemorrhoid thrombosis is a common cause of anal pain. It is caused by clot formation within the portion of the hemorrhoid covered by skin. The patient complains of a painful swelling, usually of acute onset. The pain is constant and the swelling is tender. This can occur without any obvious cause, or may follow straining, multiple loose stools, etc.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree