CHAPTER 53 ABDOMINAL VASCULAR INJURIES
Abdominal vascular injuries remain among the most lethal of injuries that the trauma surgeon will encounter. The successful management of these injuries requires a well-organized trauma system capable of swiftly transporting the patient to the appropriate facility, a trauma center capable of rapidly mobilizing an appropriate surgical team, and a trauma surgeon capable of expeditiously resuscitating the patient, localizing the injury, and controlling the source of hemorrhage.
EPIDEMIOLOGY
Penetrating abdominal injuries are the most common cause of abdominal vascular injuries, accounting for 67%–91%.1 Abdominal vascular injuries are treated much more commonly in today’s urban trauma centers than in recent military conflicts.2 Indeed, in DeBakey and Simeone’s3 classic review of 2471 arterial injuries from World War II, only 49 (2%) were abdominal arterial injuries. Similarly, Hughes4 reported on 304 arterial injuries from the Korean conflict and found 7 (2.3%) occurred in the iliac arteries. Finally, Rich and colleagues5 reviewed 1000 arterial injuries from the Vietnam conflict and found that only 29 (2.9%) involved abdominal vessels. In contrast, a 30-year review of 5760 cardiovascular injuries from Ben Taub General Hospital in Houston found 1947 (33.8%) abdominal vascular injuries.6 The Emory University trauma service at Grady Memorial Hospital consistently treats over 30 patients per year with abdominal vascular injuries. The marked difference between the two settings is believed to reflect the increased wounding power of military firearms, delayed transport to appropriate surgical facilities and, more recently, the protection of torso body armor.
Patients undergoing laparotomy after sustaining abdominal gunshot wounds will be found to have an injury to a major vessel 20%–25% of the time,7 while penetrating stab wounds will produce a major abdominal vascular injury in only 10% of patients.8 In contrast, only 5% of patients with blunt abdominal trauma are found to have an injury to a major abdominal vessel at laparotomy.9 Blunt trauma to the abdominal vasculature typically arises from either rapid deceleration or anterior crush injuries. Deceleration injuries result either in the avulsion of small branches from major vessels (such as avulsion of intestinal branches from the superior mesenteric artery) or in a proximal intimal tear with secondary thrombosis (i.e., renal artery thrombosis).10 Anterior crush injury also results in two different types of vascular trauma including an intimal flap resulting in secondary thrombosis (superior mesenteric artery, infrarenal abdominal aorta and iliac artery) or a direct blow that completely disrupts an exposed vessel (left renal vein over the aorta).11
Abdominal vascular injuries rarely occur in isolation because of a predominantly posterior-central location of a majority of the vasculature. Approximately two to four associated intra-abdominal injuries occur with abdominal vascular injuries, and patients with an injured abdominal vessel have an approximately 50% chance of having injured multiple vessels.6,12
INITIAL RESUSCITATION
Physical findings in patients with abdominal vascular trauma depend on the degree of containment of the injury. Patients with contained hematomas in the retroperitoneum, base of the mesentery, or hepatoduodenal ligament frequently present with transient hypotension that responds to an initial bolus of a crystalloid solution. These patients may remain hemodynamically stable with minimal physical findings until the hematoma is opened in the operating room. Conversely, patients presenting with free intraperitoneal hemorrhage have marked hypotension that does not respond to crystalloid boluses and may have a rigid abdomen on physical examination. Comparing patients with abdominal vascular injuries who had hypotension (a lowest emergency department systolic blood pressure of <100 mm Hg) with those without hypotension, it was noted in one study that patients with active bleeding had worse physiologic parameters (mean base deficit of −14.7 compared with −7.2), required more transfusions (15.1 units compared with 8.6 units of blood in the operating room), and had a worse survival rate (43% vs. 96%).13
Initial resuscitation for patients with suspected blunt or penetrating injuries to abdominal vessels includes basic airway maneuvers and optimizing pulmonary function. Peripheral intravenous lines should be inserted to start resuscitation with crystalloid solutions. There is no consistent evidence to definitively support either the prehospital administration of crystalloid solutions14 or the “delayed resuscitation” practice of withholding fluid.15
Agonal patients presenting to the trauma bay with a rigid abdomen secondary to penetrating trauma may require an emergency department thoracotomy with cross-clamping of the descending thoracic aorta in order to maintain cerebral and coronary arterial blood flow.16 This maneuver will clearly complicate the patient’s intraoperative course, and the need for performing this maneuver is predictive of a less than 5% survival rate.17
When transferred to the operating room, standard maneuvers need to be used to prevent hypothermia, including warming the room to more than 85° F (24.9° C), covering the head and exposed upper and lower extremities with a heating unit, using a heating cascade on the anesthetic circuit, and irrigating the body cavities with warm saline.18 If the patient’s systolic pressure is less than 70 mm Hg, some centers use a preliminary operating room thoracotomy with cross-clamping of the descending thoracic aorta before beginning a celiotomy. Even though this maneuver can assist with maintaining cerebral and cardiac blood flow, it has little effect on intra-abdominal vascular injuries because of the significant back flow. Persistent shock (systolic blood pressure <90 mm Hg) after placing a cross-clamp on the descending thoracic aorta portends a universally fatal prognosis.19
CLASSIFICATION OF INJURIES
Major abdominal vascular injuries are best classified as occurring in one of four zones as follows:
INJURIES IN SUPRAMESOCOLIC REGION OF ZONE 1
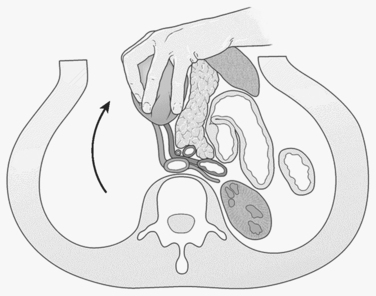
An abdominal hematoma or hemorrhage in the supramesocolic region of zone 1 typically results from an injury to the suprarenal aorta, celiac axis, proximal superior mesenteric artery, or proximal renal artery. Suprarenal aortic injuries carry reported survival rates ranging from 10%–50%.20 Proximal vascular control of the aorta should be obtained at the aortic hiatus of the diaphragm. This can be achieved either by manual compression with an aortic compressor (which is correctly positioned by dividing the lesser omentum and retracting the stomach and esophagus to the left; formal cross-clamping at this level will mandate separating the crura from the supraceliac aorta with the electrocautery) or by performing a formal left-sided medial visceral rotation (reflecting all left-sided intraabdominal viscera, including the colon, kidney, spleen, tail of the pancreas, and fundus of the stomach) (Figure 1). The advantage of the latter is that it provides exposure of the entire abdominal aorta from the hiatus to the aortic bifurcation. This is achieved at a cost of 5 minutes of exposure time and a significant risk of injury to the spleen, left kidney, or left renal artery.21,22 Supraceliac exposure can be improved by dividing the left crus of the diaphragm at the 2 o’clock position and exposing the distal descending thoracic aorta.23 An aortic cross-clamp can be applied quickly at this level with minimal dissection. Prolonged cross-clamping of the supraceliac aorta can lead to hepatic hypoperfusion, which may induce a primary fibrinolytic state24 and severe ischemia of the lower extremities. The lower extremities should be examined at the end of the procedure and compartment pressures measured below the knee; bilateral below-knee, two-skin incision, four-compartment fasciotomies should be considered for pressures over 30–35 mm Hg.
Asensio and colleagues25 recently reviewed 13 celiac axis injuries with an overall survival rate of 38% (5 of 13). Four of the five survivors were managed with ligation of the celiac axis. This is well-tolerated because of extensive collateral circulation, especially in the splenic and left gastric arterial beds. Injuries to the common hepatic artery proximal to the gastroduodenal artery are also amenable to ligation. Ligation of the celiac axis may result in necrosis of the gallbladder, however, and a cholecystectomy should be strongly considered.26 Graham et al.27 reported a series of patients with injuries to the celiac axis and noted a 100% survival in those with isolated injuries, 33% survival in those with one associated vascular injury, and 100% mortality in those with three associated vascular injuries.
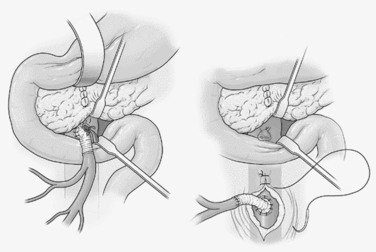
Mesenteric arterial injuries occur in only 12% of penetrating vascular injuries and are associated with 33%–57% mortality.28 Fullen and colleagues29 described four anatomic zones of the superior mesenteric artery which dictate options for repair. Fullen zone I injuries lie beneath the pancreas. Exposure requires either transection of the neck of the pancreas between Glassman clamps or a left medial visceral rotation in order to control bleeding. Fullen zone II injuries lie between the pancreaticoduodenal and the middle colic branches of the artery and lie between the pancreas and the base of the transverse mesocolon. Repairs at this level will lie adjacent to the pancreas and are susceptible to pancreatic leaks. Therefore, these lesions and those in zone I in hemodynamically unstable patients are best temporized with the insertion of a temporary intraluminal shunt until the patient is stabilized. Definitive repair can then be accomplished in a more stable patient by performing a saphenous vein or PTFE bypass from the distal infrarenal aorta through the posterior aspect of the small bowel mesentery to the distal superior mesenteric artery in an end-to-side fashion30 (Figure 2). The aortic suture line must then be protected with retroperitoneal fat or omentum in order to avoid the formation of an aorto-enteric fistula. Fullen zone III injuries lay beyond the middle colic branch, and Fullen zone IV injuries lay at the level of the enteric branches. These injures must be primarily repaired to preserve adequate blood flow to the affected regions of small bowel.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree