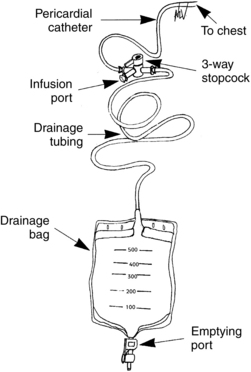
PROCEDURE 78 • Knowledge of the anatomy and physiology of the cardiovascular system, the principles of cardiac conduction, electrocardiogram (ECG) lead placement, basic dysrhythmia interpretation, and electrical safety is needed. • Understanding of sterile technique is essential. • Advanced cardiac life support knowledge and skills are needed. • Pericardial effusion is an excessive collection of fluid in the pericardial space. • The pericardial space normally contains 20 to 50 mL of fluid. Injury to the pericardium causes increased production of pericardial fluid, formation of fibrin, and cellular proliferation.2,13 • Pericardial fluid has electrolyte and protein profiles similar to plasma.13 • Causes of pericardial effusion are numerous and include infection, malignant neoplasms, autoimmune disorders, kidney failure, heart failure, acute myocardial infarction, trauma, radiation exposure, inflammatory disorders, and myxedema. Pericardial effusion may also be medication-induced, idiopathic, or a complication of invasive procedures.7,13,14 • Pericardiocentesis is an effective treatment for pericardial effusion (see Procedures 45 and 46). An indwelling pericardial catheter may be left in place after a pericardiocentesis to drain excess or continued excess production of pericardial fluid. • The pericardial catheter may be connected to a closed drainage system (Fig. 78-1). Figure 78-1 Indwelling pericardial catheter system. (From Hammel WJ: Care of patients with an indwelling pericardial catheter, Crit Care Nurse 18[5]:40-45, 1998.) • The pericardial catheter may also be left in place to allow the instillation of certain medications (i.e., nonabsorbable corticosteroid or antineoplastic agents) depending on the patient’s underlying disease state.8,12 • The indwelling pericardial catheter is usually removed within 48 to 72 hours after placement to avoid the risk of infection or iatrogenic pericarditis.13,14 The indwelling pericardial catheter may be left in place for longer periods of time to promote the resolution of a pericardial effusion or cardiac tamponade.1 Pericardial catheters are immediately removed if there is an abrupt rise in the white blood cell (WBC) level.12 • Pericardial catheters are usually removed when the total amount of drainage has decreased to less than 25 to 30 mL over the preceding 24 hours.1,13,14 • Extended catheter drainage is associated with a reduction of the re-occurrence of cardiac tamponade compared with a single pericardiocentesis in patients with pericardial effusion related to malignancy.2,3 • Sterile drapes: small drapes and a full-body drape • Sterile and nonsterile gloves, gowns, masks, protective eyewear • Sterile 0.9% normal saline solution for irrigation and sterile basin • Anticoagulant flush available for dwell as prescribed (i.e., heparin) • Sterile syringes: 3-, 5-, 30-, or 60-mL Luer-Lok • Sterile 1000-mL vacuum bottle available for the initial procedure • Antiseptic solution (e.g., 2% chlorhexidine-based preparation) • Sterile transparent occlusive dressing
Pericardial Catheter Management
PREREQUISITE NURSING KNOWLEDGE
EQUIPMENT
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


78: Pericardial Catheter Management
