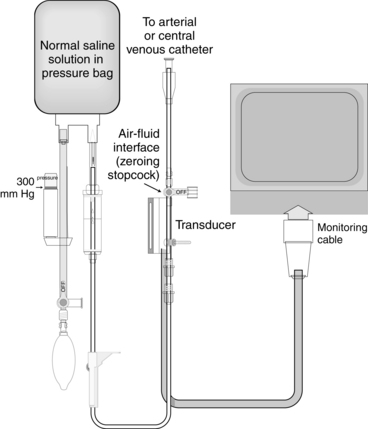
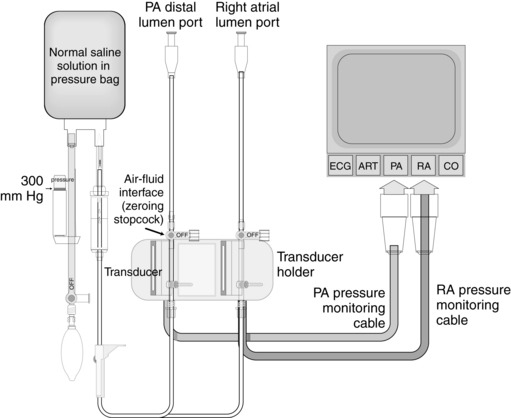
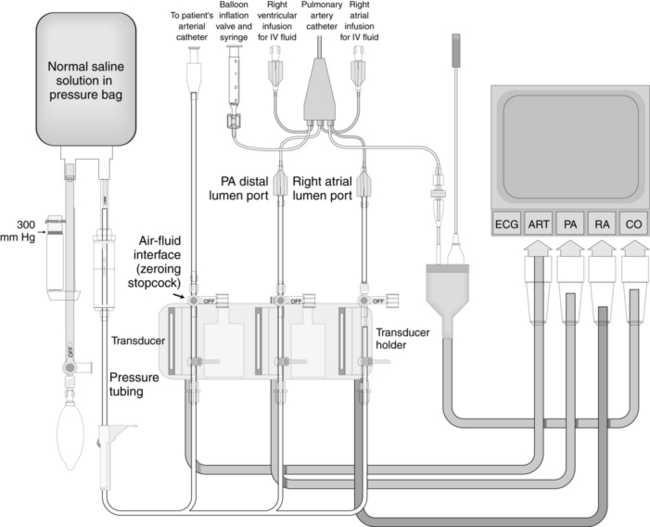
PROCEDURE 76 • Knowledge of the anatomy and physiology of the cardiovascular system is needed. • Knowledge of principles of aseptic technique is necessary. • Fluid-filled pressure monitoring systems used for bedside hemodynamic pressure monitoring are based on the principle that a change in pressure at any point in an unobstructed system results in similar pressure changes at all other points of the system. • Pressure transducers detect the pressure waveform generated by ventricular ejection and convert that pressure wave into an electrical signal, which is transmitted to the monitoring equipment for representation as a waveform on the oscilloscope. • Invasive measurement of intravascular (arterial) pressure requires insertion of a catheter into an artery. • Invasive measurement of intracardiac (right atrial and pulmonary artery) pressures requires insertion of a catheter into the pulmonary artery. • A single-pressure transducer system is used to measure pressure from a single catheter (e.g., arterial catheter, central venous; Fig. 76-1). • A double-pressure transducer system is used to measure pressure from two catheters (e.g., arterial and central venous) or two ports (e.g., pulmonary artery and right atrial) from a single catheter (e.g., pulmonary artery catheter; Fig. 76-2). • A triple-pressure transducer system is commonly used to measure pressures from the arterial and pulmonary artery catheters. With this system, arterial pressures, pulmonary artery pressures, and right atrial pressures can be obtained (Fig. 76-3). Figure 76-3 Triple-pressure transducer system. (Drawing by Paul W. Schiffmacher, Thomas Jefferson University, Philadelphia, PA.) • For accuracy of the hemodynamic values obtained from any transducer system, leveling and zeroing are essential. • All hemodynamic values (pulmonary artery, right atrial, and arterial) are referenced to the level of the atria. The external reference point of the atria is the phlebostatic axis. • Invasive catheter (e.g., arterial, pulmonary artery) • Pressure modules and cables for interface with the monitor • Cardiac output cable with a thermistor/injectate sensor for use with the pulmonary artery catheter • Pressure transducer system, including flush solution recommended according to institution standard, a pressure bag or device, pressure tubing with transducers, and flush device • Monitoring system (central and bedside monitor) Additional equipment as needed includes the following: • Assess patient and family understanding of hemodynamic monitoring and the reason for its use. • Explain the procedure for hemodynamic monitoring. • Assess the patient for conditions that may warrant the use of a hemodynamic monitoring system, including hypotension or hypertension, cardiac failure, cardiac arrest, hemorrhage, respiratory failure, fluid imbalances, oliguria, anuria, and sepsis.
Single-Pressure and Multiple-Pressure Transducer Systems
PREREQUISITE NURSING KNOWLEDGE
EQUIPMENT
PATIENT AND FAMILY EDUCATION
 Rationale: Clarification or reinforcement of information is an expressed patient and family need.
Rationale: Clarification or reinforcement of information is an expressed patient and family need.
 Rationale: This information prepares the patient and the family for what to expect and may decrease anxiety.
Rationale: This information prepares the patient and the family for what to expect and may decrease anxiety.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
 Rationale: Assessment provides data regarding signs and symptoms of hemodynamic instability.
Rationale: Assessment provides data regarding signs and symptoms of hemodynamic instability.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


76: Single-Pressure and Multiple-Pressure Transducer Systems