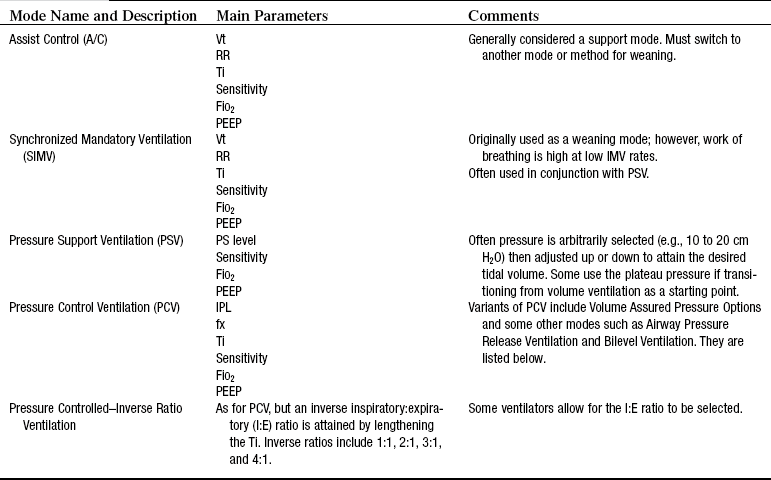
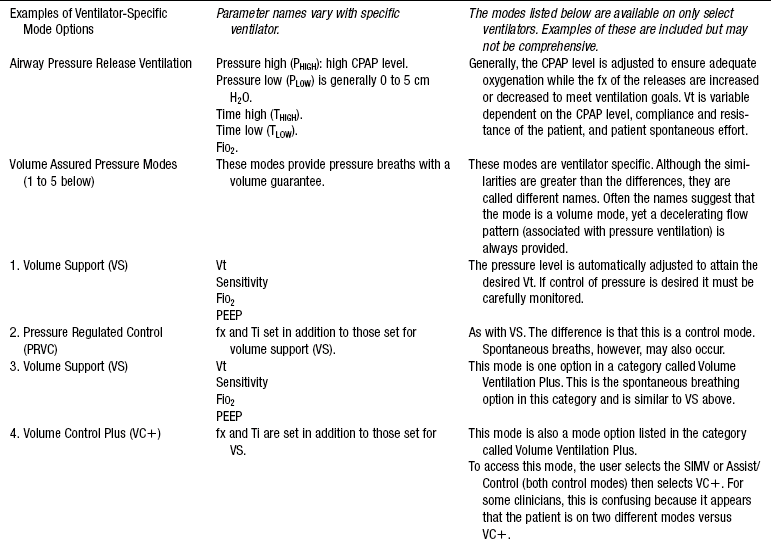
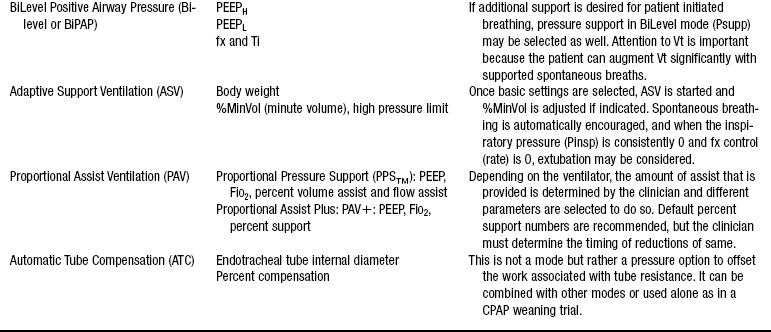
PROCEDURE 35 • Indications for the initiation of mechanical ventilation include the following: • Ventilators are categorized as either negative or positive pressure. Although negative-pressure ventilation (i.e., the iron lung) was used extensively in the 1940s, introduction of the cuffed endotracheal tube resulted in the dominance of positive-pressure ventilation (PPV) in clinical practice during the second half of the 20th century. Although sporadic interest in negative-pressure ventilation continues, the cumbersome nature of the ventilators and the lack of airway protection associated with this form of ventilation preclude a serious resurgence of this mode of ventilation. • Summary descriptions of modes, mode parameters, and ventilator alarms are provided within this procedure and in Tables 35-1, 35-2, and 35-3. Table 35-1 Traditional Modes of Mechanical Ventilation (on All Ventilators) Volume Modes Control Ventilation (CV) or Controlled Mandatory Ventilation (CMV) Description: With this mode, the ventilator provides all of the patient’s minute ventilation. The clinician sets the rate, Vt, inspiratory time, and PEEP. Generally, this term is used to describe situations in which the patient is chemically relaxed or is paralyzed from a spinal cord or neuromuscular disease and is unable to initiate spontaneous breaths. The ventilator mode setting may be set on CMV, assist/control (A/C), or synchronized intermittent mandatory ventilation (SIMV) because all these options provide volume breaths at the clinician-selected rate. Assist/Control (A/C) or Assisted Mandatory Ventilation (AMV) Description: This option requires that a rate, Vt, inspiratory time, and PEEP be set for the patient. The ventilator sensitivity also is set, and when the patient initiates a spontaneous breath, a full-volume breath is delivered. Synchronized Intermittent Mandatory Ventilation (SIMV) Description: This mode requires that rate, Vt, inspiratory time, sensitivity, and PEEP are set by the clinician. In between mandatory breaths, patients can spontaneously breathe at their own rates and Vt. With SIMV, the ventilator synchronizes the mandatory breaths with the patient’s own inspirations. Pressure Modes Pressure Support Ventilation (PSV) Description: This mode provides an augmented inspiration to a patient who is spontaneously breathing. With PS, the clinician selects an inspiratory pressure level, PEEP, and sensitivity. When the patient initiates a breath, a high flow of gas is delivered to the preselected pressure level, and pressure is maintained throughout inspiration. The patient determines the parameters of Vt, rate, and inspiratory time. Pressure-Controlled/Inverse Ratio Ventilation (PC/IRV) Description: This mode combines pressure-limited ventilation with an inverse ratio of inspiration to expiration. The clinician selects the pressure level, rate, inspiratory time (1:1, 2:1, 3:1, 4:1), and PEEP level. With prolonged inspiratory times, auto-PEEP may result. The auto-PEEP may be a desirable outcome of the inverse ratios. Some clinicians use PC without IRV. Conventional inspiratory times are used, and rate, pressure level, and PEEP are selected. Positive End-Expiratory Pressure (PEEP) and Continuous Positive Airway Pressure (CPAP) Description: This ventilatory option creates positive pressure at end exhalation. PEEP restores FRC. The term PEEP is used when end-expiratory pressure is provided during ventilator positive pressure breaths. Table 35-2 Volume and Pressure Modes and Corresponding Ventilator Parameters Adapted with permission from Burns S: Pressure modes of mechanical ventilation: the good, bad and the ugly, AACN Adv Crit Care 19:399-411, 2008. Table 35-3 Disconnect Alarms (Low-Pressure or Low-Volume Alarms) When disconnection occurs, the clinician must be immediately notified. Generally, this alarm is a continuous one and is triggered when a preselected inspiratory pressure level or minute ventilation is not sensed. With circuit leaks, this same alarm may be activated even though the patient may still be receiving a portion of the preset breath. Physical assessment, digital displays, and manometers are helpful in troubleshooting the cause of the alarms. Pressure Alarms High-pressure alarms are set with volume modes of ventilation to ensure notification of pressures that exceed the selected threshold. These alarms are usually set 10 to 15 cm H2O above the usual peak inspiratory pressure (PIP). Some causes for alarm activation (generally an intermittent alarm) include secretions, condensate in the tubing, biting on the endotracheal tubing, increased resistance (i.e., bronchospasm), decreased compliance (e.g., pulmonary edema, pneumothorax), and tubing compression. Low-pressure alarms are used to sense disconnection, circuit leaks, and changing compliance and resistance. They are generally set 5 to 10 cm H2O below the usual PIP or 1 to 2 cm H2O below the PEEP level or both. Minute ventilation alarms may be used to sense disconnection or changes in breathing pattern (rate and volume). Generally, low–minute ventilation and high–minute ventilation alarms are set (usually 5 to 10 L/min above and below usual minute ventilation). When stand-alone pressure support ventilation (PSV) is in use, this alarm may be the only audible alarm available on some ventilators. FiO2 alarms are provided on most new ventilators and are set 5 to 10 mm Hg above and below the selected FiO2 level. Alarm silence or pause options are built in by ventilator manufacturers so that clinicians can temporarily silence alarms for short periods (i.e., 20 seconds) because alarms must stay activated at all times. The ventilators reset the alarms automatically. Alarms provide important protection for patients on ventilation. However, inappropriate threshold settings decrease usefulness. When threshold gradients are set too narrowly, alarms occur needlessly and frequently. Conversely, alarms that are set too loosely (wide gradients) do not allow for accurate and timely assessments. From Burns SM: Mechanical ventilation and weaning. In Kinney MR, et al, editors: AACN clinical reference for critical care nursing, ed 4, St Louis, 1998, Mosby. • Complications of PPV include volume-pressure trauma, hemodynamic changes, and pulmonary barotrauma. • Associated complications of PPV include ventilator-associated pneumonia (VAP)6, deep vein thrombosis (and subsequent pulmonary embolus), and gastrointestinal bleeding. Although all the associated complications are important and require that appropriate evidence-based prophylaxis regimens are initiated, only VAP is discussed. Please refer to other system-specific chapters in this manual for information on the others. Table 35-4 Top Modifiable VAP Prevention Interventions: Guidelines by Authoritative Professional Organizations. Top Guideline Recommendations by Professional Associations* BRE (>30 to 45 degrees) CASS tubes Cuff inflation Hand washing and aseptic technique HMEs No routine ventilator circuit change Noninvasive ventilation when possible *Professional Associations: American Thoracic Society (ATS), American Association of Critical-Care Nurses (AACN), Centers for Disease Control and Prevention (CDC), and Canadian Critical Care Trials Group and the Canadian Critical Care Society (CCCT/CCCS). • Endotracheal or tracheostomy tube (see Procedures 2 and 14) • Electrocardiogram and pulse oximetry • Manual self-inflating resuscitation bag-valve device (with PEEP adjusted to patient baseline level or with a PEEP valve) • Appropriately sized resuscitation face mask • End-tidal carbon dioxide detector, with a colorimetric CO2 detector or continuous monitor: The colorimetric detectors are used to ensure proper endotracheal tube placement and are a standard of care for intubation in many institutions. The continuous monitors are used in assessment of patients on ventilation on an ongoing basis. • Explain the procedure and the reasons for PPV to the patient and family.6 • Discuss the potential sensations the patient will experience, such as relief of dyspnea, lung inflations, noise of ventilator operation, and alarm sounds. • Encourage the patient to relax. • Explain that the patient will be unable to speak. Establish a method of communication in conjunction with the patient and family before initiating mechanical ventilation, if necessary.
Invasive Mechanical Ventilation (Through an Artificial Airway): Volume and Pressure Modes
PREREQUISITE NURSING KNOWLEDGE
 Apnea (e.g., neuromuscular or cardiopulmonary collapse)
Apnea (e.g., neuromuscular or cardiopulmonary collapse)
 Acute ventilatory failure, which is generally defined as a pH of less than or equal to 7.25 with an arterial partial pressure of carbon dioxide (PaCO2) greater than or equal to 50 mm Hg
Acute ventilatory failure, which is generally defined as a pH of less than or equal to 7.25 with an arterial partial pressure of carbon dioxide (PaCO2) greater than or equal to 50 mm Hg
 Impending ventilatory failure (serial decrement of arterial blood gas [ABG] values or progressive increase in signs and symptoms of increased work of breathing)
Impending ventilatory failure (serial decrement of arterial blood gas [ABG] values or progressive increase in signs and symptoms of increased work of breathing)
 Severe hypoxemia: An arterial partial pressure of oxygen (PaO2) of less than or equal to 50 mm Hg on room air indicates a critical level of oxygen in the blood. Although oxygen delivery devices may be used before intubation, the refractory nature of shunt (perfusion without ventilation) may necessitate that positive pressure be applied to reexpand closed alveoli. Restoration of functional residual capacity (FRC; lung volume that remains at the end of a passive exhalation) is the goal.
Severe hypoxemia: An arterial partial pressure of oxygen (PaO2) of less than or equal to 50 mm Hg on room air indicates a critical level of oxygen in the blood. Although oxygen delivery devices may be used before intubation, the refractory nature of shunt (perfusion without ventilation) may necessitate that positive pressure be applied to reexpand closed alveoli. Restoration of functional residual capacity (FRC; lung volume that remains at the end of a passive exhalation) is the goal.
 Respiratory muscle fatigue: The muscles of respiration can become fatigued if they are made to contract repetitively at high workloads.87 Fatigue occurs when muscle energy stores become depleted. Weakness, hypermetabolic states, and chronic lung disease are examples of conditions in which patients are especially prone to fatigue. When fatigue occurs, the muscles no longer contract optimally and hypercarbia results.8,20 Twelve to 24 hours of rest are typically needed to rest the muscles. Respiratory muscle rest requires that the workload of the muscles (or muscle loading) be offset so that mitochondrial energy stores can be repleted.8,20 Respiratory work and rest vary with different modes and the application of the same. In general, when hypercarbia is present, mechanical ventilation is necessary to relieve the work of breathing. Muscle unloading is accomplished differently and depends on patient-ventilator interaction and the mode.13,14,55,57,61,68
Respiratory muscle fatigue: The muscles of respiration can become fatigued if they are made to contract repetitively at high workloads.87 Fatigue occurs when muscle energy stores become depleted. Weakness, hypermetabolic states, and chronic lung disease are examples of conditions in which patients are especially prone to fatigue. When fatigue occurs, the muscles no longer contract optimally and hypercarbia results.8,20 Twelve to 24 hours of rest are typically needed to rest the muscles. Respiratory muscle rest requires that the workload of the muscles (or muscle loading) be offset so that mitochondrial energy stores can be repleted.8,20 Respiratory work and rest vary with different modes and the application of the same. In general, when hypercarbia is present, mechanical ventilation is necessary to relieve the work of breathing. Muscle unloading is accomplished differently and depends on patient-ventilator interaction and the mode.13,14,55,57,61,68
 Positive pressure ventilation: Positive-pressure modes of ventilation have traditionally been categorized into volume and pressure. However, with the advent of microprocessor technology, sophisticated iterations of traditional volume and pressure modes of ventilation have evolved.69 Many of the modes have names that are different from traditional volume and pressure modes, but they are similar in many cases. Little data exist to show that the newer modes improve outcomes.17,69 A wide variety of modes described in this procedure are actually a combination of volume and pressure but for ease of learning are classified into specific categories.
Positive pressure ventilation: Positive-pressure modes of ventilation have traditionally been categorized into volume and pressure. However, with the advent of microprocessor technology, sophisticated iterations of traditional volume and pressure modes of ventilation have evolved.69 Many of the modes have names that are different from traditional volume and pressure modes, but they are similar in many cases. Little data exist to show that the newer modes improve outcomes.17,69 A wide variety of modes described in this procedure are actually a combination of volume and pressure but for ease of learning are classified into specific categories.
 Volume ventilation has traditionally been the most popular form of PPV, largely because tidal volume (Vt) and minute ventilation (MV) are ensured, which is an essential goal in the patient with acute illness. With volume ventilation, a predetermined Vt is delivered with each breath regardless of resistance and compliance. Vt is stable from breath to breath, but airway pressure may vary. To rest the respiratory muscles with volume ventilation, the ventilator rate must be increased until spontaneous respiratory effort ceases. When spontaneous effort is present, such as with initiation of an assist/control (A/C) breath, respiratory muscle work continues throughout the breath.61
Volume ventilation has traditionally been the most popular form of PPV, largely because tidal volume (Vt) and minute ventilation (MV) are ensured, which is an essential goal in the patient with acute illness. With volume ventilation, a predetermined Vt is delivered with each breath regardless of resistance and compliance. Vt is stable from breath to breath, but airway pressure may vary. To rest the respiratory muscles with volume ventilation, the ventilator rate must be increased until spontaneous respiratory effort ceases. When spontaneous effort is present, such as with initiation of an assist/control (A/C) breath, respiratory muscle work continues throughout the breath.61
 With traditional pressure ventilation, the practitioner selects the desired pressure level and the Vt is determined by the selected pressure level, resistance, and compliance. This characteristic is important to note in caring for a patient with an unstable condition on a pressure mode of ventilation. Careful attention to Vt is necessary to prevent inadvertent hyperventilation or hypoventilation. To ensure respiratory muscle rest on pressure-support ventilation (PSV), workload must be offset with the appropriate adjustment of the pressure-support (PS) level. To accomplish this adjustment, the PS level is increased to lower the spontaneous respiratory rate to less than or equal to 20 breaths/min and to attain a Vt of 6 to 10 mm/kg.13,14,55
With traditional pressure ventilation, the practitioner selects the desired pressure level and the Vt is determined by the selected pressure level, resistance, and compliance. This characteristic is important to note in caring for a patient with an unstable condition on a pressure mode of ventilation. Careful attention to Vt is necessary to prevent inadvertent hyperventilation or hypoventilation. To ensure respiratory muscle rest on pressure-support ventilation (PSV), workload must be offset with the appropriate adjustment of the pressure-support (PS) level. To accomplish this adjustment, the PS level is increased to lower the spontaneous respiratory rate to less than or equal to 20 breaths/min and to attain a Vt of 6 to 10 mm/kg.13,14,55
 Pressure ventilation provides for an augmented inspiration (pressure is maintained throughout inspiration). The flow pattern (speed of the gas) is described as decelerating; that is, gas flow delivery is high at the beginning of the breath and tapers off toward the end of the breath. This pattern is in contrast to volume ventilation, in which the flow rate is typically more consistent during inspiration (i.e., the same at the beginning of the breath as at the end of the breath). The decelerating flow pattern associated with pressure ventilation is thought to provide better gas distribution and more efficient ventilation.14,55,56
Pressure ventilation provides for an augmented inspiration (pressure is maintained throughout inspiration). The flow pattern (speed of the gas) is described as decelerating; that is, gas flow delivery is high at the beginning of the breath and tapers off toward the end of the breath. This pattern is in contrast to volume ventilation, in which the flow rate is typically more consistent during inspiration (i.e., the same at the beginning of the breath as at the end of the breath). The decelerating flow pattern associated with pressure ventilation is thought to provide better gas distribution and more efficient ventilation.14,55,56
 Increasingly sophisticated ventilator technology has resulted in the development of volume-assured pressure modes of ventilation. Ventilator manufacturers have responded rapidly to the request of practitioners that pressure modes of ventilation be designed in such a way that volume be guaranteed on a breath-to-breath basis. The potential value of such modes is obvious. The more desirable decelerating flow pattern may be provided and plateau pressures controlled, with ensured Vt and MV.
Increasingly sophisticated ventilator technology has resulted in the development of volume-assured pressure modes of ventilation. Ventilator manufacturers have responded rapidly to the request of practitioners that pressure modes of ventilation be designed in such a way that volume be guaranteed on a breath-to-breath basis. The potential value of such modes is obvious. The more desirable decelerating flow pattern may be provided and plateau pressures controlled, with ensured Vt and MV.
 Additional modes of ventilation have been promoted for use in patients with acute respiratory distress syndrome (ARDS), including high-frequency oscillation, pressure-release ventilation, and other ventilator-specific modes, such as biphasic, adaptive support and proportional assist ventilation. Although some data exist that suggest the modes may be beneficial in patients with ARDS, to date no change in mortality rate has been noted, although positive trends have been demonstrated in some variables of interest such as oxygenation.12,18,19,24,27,38,39,41,59,66,73,75,79–82,84,90
Additional modes of ventilation have been promoted for use in patients with acute respiratory distress syndrome (ARDS), including high-frequency oscillation, pressure-release ventilation, and other ventilator-specific modes, such as biphasic, adaptive support and proportional assist ventilation. Although some data exist that suggest the modes may be beneficial in patients with ARDS, to date no change in mortality rate has been noted, although positive trends have been demonstrated in some variables of interest such as oxygenation.12,18,19,24,27,38,39,41,59,66,73,75,79–82,84,90
 Volume-pressure trauma, in contrast to barotrauma (or air leak disease), was first described in animals with stiff noncompliant lungs who were ventilated with traditional lung volumes (range, 10 to 12 mL/kg). The investigators noted that the large volumes translated into high plateau pressures (also known as static, distending, or alveolar pressure) and subsequent acute lung injury. The lung injury was described as a loss of alveolar integrity (i.e., alveolar fractures) and movement of fluids and proteins into the alveolar space (sometimes called non-ARDS-ARDS).28,29,37,70,93 Plateau pressures of 30 cm H2O or more for greater than 48 to 72 hours were associated with the injury.28
Volume-pressure trauma, in contrast to barotrauma (or air leak disease), was first described in animals with stiff noncompliant lungs who were ventilated with traditional lung volumes (range, 10 to 12 mL/kg). The investigators noted that the large volumes translated into high plateau pressures (also known as static, distending, or alveolar pressure) and subsequent acute lung injury. The lung injury was described as a loss of alveolar integrity (i.e., alveolar fractures) and movement of fluids and proteins into the alveolar space (sometimes called non-ARDS-ARDS).28,29,37,70,93 Plateau pressures of 30 cm H2O or more for greater than 48 to 72 hours were associated with the injury.28
 Studies in humans followed the recognition that large Vts may be associated with lung injury.42,86 The ARDS Network conducted randomized controlled trial (RCTs) of adult patients with ARDS that compared low lung volume ventilation (6 mL/kg) with more traditional volumes (i.e., 12 mL/kg). The results showed that the lower volume ventilation resulted in a lower mortality rate.86 As a result, current recommendations are to limit volumes (and lower pressures) in patients with stiff lungs. With pressure ventilation, pressure is limited by definition; however, until additional evidence emerges on the efficacy of controlling pressures versus volumes in ARDS, a goal should be to ensure a Vt in the 6 mL/kg range. Another lung protective strategy is that of is that of “recruitment” and the prevention of “derecruitment.” Investigators showed that stiff noncompliant lungs were at risk of trauma from the repetitive opening associated with tidal breaths. The application of higher levels of positive end-expiratory pressure (PEEP) was associated with better recruitment and resulted in improved mortality rates.3,4,73
Studies in humans followed the recognition that large Vts may be associated with lung injury.42,86 The ARDS Network conducted randomized controlled trial (RCTs) of adult patients with ARDS that compared low lung volume ventilation (6 mL/kg) with more traditional volumes (i.e., 12 mL/kg). The results showed that the lower volume ventilation resulted in a lower mortality rate.86 As a result, current recommendations are to limit volumes (and lower pressures) in patients with stiff lungs. With pressure ventilation, pressure is limited by definition; however, until additional evidence emerges on the efficacy of controlling pressures versus volumes in ARDS, a goal should be to ensure a Vt in the 6 mL/kg range. Another lung protective strategy is that of is that of “recruitment” and the prevention of “derecruitment.” Investigators showed that stiff noncompliant lungs were at risk of trauma from the repetitive opening associated with tidal breaths. The application of higher levels of positive end-expiratory pressure (PEEP) was associated with better recruitment and resulted in improved mortality rates.3,4,73
 The extent of hemodynamic changes associated with PPV depends on the level of applied positive pressure, the duration of positive pressure during different phases of the breathing cycle, the amount of pressure transmitted to the vascular structures, the patient’s intravascular volume, and the adequacy of hemodynamic compensatory mechanisms. PPV can reduce venous return, shift the intraventricular septum to the left, and increase right ventricular afterload as a result of increased pulmonary vascular resistance.1,50 The hemodynamic effects of PPV may be prevented or corrected by optimizing filling pressures to accommodate the PPV-induced changes in intrathoracic pressures; by minimizing the peak pressure, plateau pressure, and PEEP; and by optimizing the inspiratory-to-expiratory (I:E) ratio.
The extent of hemodynamic changes associated with PPV depends on the level of applied positive pressure, the duration of positive pressure during different phases of the breathing cycle, the amount of pressure transmitted to the vascular structures, the patient’s intravascular volume, and the adequacy of hemodynamic compensatory mechanisms. PPV can reduce venous return, shift the intraventricular septum to the left, and increase right ventricular afterload as a result of increased pulmonary vascular resistance.1,50 The hemodynamic effects of PPV may be prevented or corrected by optimizing filling pressures to accommodate the PPV-induced changes in intrathoracic pressures; by minimizing the peak pressure, plateau pressure, and PEEP; and by optimizing the inspiratory-to-expiratory (I:E) ratio.
 Pulmonary barotrauma (i.e., air leak disease) is damage to the lung from extrapulmonary air that may result from changes in intrathoracic pressures during PPV. Barotrauma is manifested by pneumothorax, pneumomediastinum, pneumopericardium, pneumoperitoneum, and subcutaneous emphysema. The risk of barotrauma in a patient receiving PPV is increased with preexisting lung lesions (e.g., localized infections, blebs), high inflation pressures (i.e., large Vt, PEEP, main-stem bronchus intubation, patient-ventilator asynchrony), and invasive thoracic procedures (e.g., subclavian catheter insertion, bronchoscopy, thoracentesis). Barotrauma from PPV may be prevented by controlling peak and plateau pressures, optimizing PEEP, preventing auto-PEEP, ensuring patient-ventilator synchrony, and ensuring proper artificial airway position.
Pulmonary barotrauma (i.e., air leak disease) is damage to the lung from extrapulmonary air that may result from changes in intrathoracic pressures during PPV. Barotrauma is manifested by pneumothorax, pneumomediastinum, pneumopericardium, pneumoperitoneum, and subcutaneous emphysema. The risk of barotrauma in a patient receiving PPV is increased with preexisting lung lesions (e.g., localized infections, blebs), high inflation pressures (i.e., large Vt, PEEP, main-stem bronchus intubation, patient-ventilator asynchrony), and invasive thoracic procedures (e.g., subclavian catheter insertion, bronchoscopy, thoracentesis). Barotrauma from PPV may be prevented by controlling peak and plateau pressures, optimizing PEEP, preventing auto-PEEP, ensuring patient-ventilator synchrony, and ensuring proper artificial airway position.
 Auto-PEEP is a common complication of mechanical ventilation and can result in hemodynamic compromise and even death. Because increased intrathoracic pressures are transmitted to the adjacent capillaries, venous return is decreased and the effect can be profound. Auto-PEEP and dynamic hyperinflation should be assumed in the patient on ventilation with acute severe asthma whose condition is hemodynamically compromised, and a brief cessation of mechanical ventilation or decrease in rate and shortening of inspiratory time should be accomplished.54,71 Auto-PEEP is caused by inadequate expiratory time relative to the patient’s lung condition. Auto-PEEP is associated with prolonged inspiratory times, short expiratory times, high minute ventilation requirements, bronchospasm, low elastic recoil, mucus hypersecretion, increased wall thickness, airway closure or collapse, and mechanical factors (e.g., water in the ventilator circuit, pinched ventilator tubing).54,71 Correcting these factors reduces auto-PEEP. In some cases, adding set PEEP results in reduction of the inspiratory trigger threshold and thus improvement of patient triggering.15,58
Auto-PEEP is a common complication of mechanical ventilation and can result in hemodynamic compromise and even death. Because increased intrathoracic pressures are transmitted to the adjacent capillaries, venous return is decreased and the effect can be profound. Auto-PEEP and dynamic hyperinflation should be assumed in the patient on ventilation with acute severe asthma whose condition is hemodynamically compromised, and a brief cessation of mechanical ventilation or decrease in rate and shortening of inspiratory time should be accomplished.54,71 Auto-PEEP is caused by inadequate expiratory time relative to the patient’s lung condition. Auto-PEEP is associated with prolonged inspiratory times, short expiratory times, high minute ventilation requirements, bronchospasm, low elastic recoil, mucus hypersecretion, increased wall thickness, airway closure or collapse, and mechanical factors (e.g., water in the ventilator circuit, pinched ventilator tubing).54,71 Correcting these factors reduces auto-PEEP. In some cases, adding set PEEP results in reduction of the inspiratory trigger threshold and thus improvement of patient triggering.15,58
 VAP occurs after 3 to 5 days of mechanical ventilation and accounts for one third of all healthcare-associated infections and between 50% and 83% of infections in the patient with MV.6,26,52,78,91
VAP occurs after 3 to 5 days of mechanical ventilation and accounts for one third of all healthcare-associated infections and between 50% and 83% of infections in the patient with MV.6,26,52,78,91
 Modifiable risk factors to the aspiration of colonized organisms in the patient on ventilation include interventions such as proper endotracheal tube cuff inflation (secretions that collect above the cuff of the endotracheal or tracheostomy tube and leak past the cuff into the lungs), use of continuous aspiration subglottic suctioning (CASS) tubes, decreased ventilator tubing changes, use of heat and moisture exchangers (HMEs), stringent hand washing, backrest elevation (BRE) of greater than 30 degrees, and when possible, the use of noninvasive ventila- tion (especially in patients with immunocompromise).5,6,10,16,22,26,32,43,45,51,64,72,83
Modifiable risk factors to the aspiration of colonized organisms in the patient on ventilation include interventions such as proper endotracheal tube cuff inflation (secretions that collect above the cuff of the endotracheal or tracheostomy tube and leak past the cuff into the lungs), use of continuous aspiration subglottic suctioning (CASS) tubes, decreased ventilator tubing changes, use of heat and moisture exchangers (HMEs), stringent hand washing, backrest elevation (BRE) of greater than 30 degrees, and when possible, the use of noninvasive ventila- tion (especially in patients with immunocompromise).5,6,10,16,22,26,32,43,45,51,64,72,83
 Other interventions with a lower level of evidence supporting their use include oral care techniques such as mouth care and oral decontamination with agents such as chlorhexidine or oral antibiotics.45 Of interest, gastric residual volumes have not been found to be consistently associated with VAP.46,65 Table 35-4 lists the top recommendations of authoritative professional organizations for the prevention of VAP.
Other interventions with a lower level of evidence supporting their use include oral care techniques such as mouth care and oral decontamination with agents such as chlorhexidine or oral antibiotics.45 Of interest, gastric residual volumes have not been found to be consistently associated with VAP.46,65 Table 35-4 lists the top recommendations of authoritative professional organizations for the prevention of VAP.
EQUIPMENT
PATIENT AND FAMILY EDUCATION
 Rationale: Communication and explanations for therapy are cited as important needs of patients and families.
Rationale: Communication and explanations for therapy are cited as important needs of patients and families.
 Rationale: Knowledge of anticipated sensory experiences reduces anxiety and distress.
Rationale: Knowledge of anticipated sensory experiences reduces anxiety and distress.
 Rationale: This encouragement promotes general relaxation, oxygenation, and ventilation.
Rationale: This encouragement promotes general relaxation, oxygenation, and ventilation.
 Rationale: Ensuring the patient’s ability to communicate is important to alleviate anxiety.
Rationale: Ensuring the patient’s ability to communicate is important to alleviate anxiety.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


35: Invasive Mechanical Ventilation (Through an Artificial Airway): Volume and Pressure Modes
