CHAPTER 33. The Pediatric Patient
Reneé Semonin Holleran
Competencies
1. Identify the differences between the pediatric and adult patient.
2. Perform a primary and secondary assessment of the pediatric patient in preparation for transport.
3. Provide an overview of some selected pediatric illnesses and injuries.
4. Identify the equipment necessary to perform a competent pediatric transport.
The care and transport of the ill or injured pediatric patient requires an ability to quickly assess and treat acute changes in a child’s condition. Consideration of the critical anatomic and physiologic differences in this population is paramount for safe and effective intervention. An understanding of normal growth and development in children is an invaluable tool for the pediatric practitioner.
A DEVELOPMENTAL APPROACH TO PEDIATRIC ASSESSMENT
The assessment of an ill or injured child is for all intents and purposes not dissimilar to the evaluation of an adult. The challenge in caring for children is the impact of growth and development on a variety of clinical factors. A child’s age can present challenges in ability to communicate verbally, response to invasive procedures, and ability to be separated from a family member, and it may be a risk factor for traumatic injury. For proper treatment of children with illness and injuries and, more importantly, for teaching parents and children to avoid injury, growth and developmental factors must be used as a foundation for clinical care. Table 33-1 summarizes age-specific development and injury patterns.
| SIDS, Sudden infant death syndrome; MVC, motor vehicle collisions. | ||
| Age | Development | At-Risk Injuries |
|---|---|---|
| Infant, 0 to 4 months | Feeding, holding, bonding and dependence on caregivers. | Aspiration, SIDS, bathing injuries (burns, near drowning), environmental exposures (heat and cold), abuse/neglect/homicide/sexual assault, MVCs without proper restraint. |
| Infant, 4 to 8 months | Introduction of solid foods, teething, rolling side to side, sitting up, crawling. | Falls, electrocution from cords/outlets, foreign body aspiration, toxic ingestions, MVCs without proper restraint, burns, near drowning, abuse/neglect/homicide/sexual assault, lacerations, fractures, head and spine injuries. |
| Infant, 8 to 12 months | Crawling, walking, increased motor coordination (opening doors, latches, etc). | Falls, aspiration, foreign body ingestion, toxic ingestion, pedestrian versus vehicle injuries, near drowning, electrocution, MVCs without proper restraint, burns, suffocation, abuse/neglect/homicide, lacerations, fractures, head and spine injuries. |
| Child, 15 months to 3 years | Walking well and running, increased climbing skills, increased use of riding toys, use of utensils and cup, advanced motor skills (latches, doorways, match/lighter use). Emotionally, have increased desire for autonomy but have stranger anxiety. Beginning to speak simple sentences. | Falls, strike by vehicle as pedestrian or bike rider, burns, suffocation, near drowning, toxic ingestions, foreign body aspiration, electrocution, MVCs without proper restraint, abuse/neglect/homicide, lacerations, fractures, head and spine injuries. |
| Child, 4 to 9 years | Bike riding, swimming skills, entry into school systems; use of tools, firearms, and weapons. Increased exposures to nonfamily members, involvement in team sports. Use of seat belts. Emotionally continue to increase autonomy with heightened body awareness and sensitivity to invasive examinations/procedures. Rapidly increasing verbal skills. | Toxic ingestions, foreign body aspiration, electrocution, MVCs without proper restraint, abuse/neglect/homicide/sexual assault, lacerations, fractures, head and spine injuries. |
| Child, 10 to 12 years | Rapid physical growth, learning complex social skills, beginning of alcohol/tobacco/drug experimentation, increased sexual experimentation, and involvement in largely physical team sports. Use of motorized vehicles. Emotionally, have heightened awareness in gender differences, intense need for privacy, sense of responsibility, and need to be involved in decision making. May experience clinical depression. | Falls, strikes by vehicle as pedestrian or vehicle rider, burns, near drowning, toxic ingestions, drug/alcohol overdose, foreign body aspiration, electrocution, MVCs without proper restraint, abuse/neglect/homicide/sexual assault, suicide, complications of pregnancy or contraception, lacerations, fractures, head and spine injuries. |
| Child, 12 to 16 years | Increased incidence of risk-taking behaviors, increased autonomy in decisions of daily living, begin car driving, begin part-time jobs, increased sexual behavior, increased drug/alcohol/tobacco use. Emotionally, have increased body image disturbances, increased need for independence/decision making. May suffer from clinical depression. | MVCs, falls, occupational injuries, strikes by vehicle as pedestrian or bike rider, burns, near drowning, toxic ingestions, drug/alcohol overdose, foreign body aspiration, electrocution, abuse/neglect/homicide/suicide/sexual assault, complications of pregnancy or contraception, lacerations, fractures, head and spine injuries. |
Although not addressed in Table 33-1, children, regardless of age, are at risk for emergent complications that arise from infectious disease and metabolic or endocrine disorders. These conditions are discussed briefly later in this chapter. Box 33-1 contains examples of developmental approaches to the pediatric patient. 5,6
BOX 33-1
Get Clinical Tree app for offline access

Developmental Stages and Approach Strategies for Pediatric Patients
Infants
Major Fears
Separation and strangers.
Approach Strategies
Provide consistent caretakers.
Reduce parent anxiety because it is transmitted to the infant.
Minimize separation from parents.
Toddlers
Major Fears
Separation and loss of control.
Characteristics of Thinking
Primitive.
Unable to recognize views of others.
Little concept of body integrity.
Approach Strategies
Keep explanations simple.
Choose words carefully.
Let toddler play with equipment (stethoscope).
Minimize separation from parents.
Preschoolers
Major Fears
Bodily injury and mutilation.
Loss of control.
The unknown and the dark.
Being left alone.
Characteristics of Thinking
Highly literal interpretation of words.
Unable to abstract.
Primitive ideas about the body (e.g., fear that all blood will “leak out” if a bandage is removed).
Approach Strategies
Keep explanations simple and concise.
Choose words carefully.
Emphasize that a procedure helps the child be healthier.
Be honest.
School-Age Children
Major Fears
Loss of control.
Bodily injury and mutilation.
Failure to live up to expectations of others.
Death.
Characteristics of Thinking
Vague or false ideas about physical illness and body structure and function.
Able to listen attentively without always comprehending.
Reluctant to ask questions about something they think they are expected to know.
Increased awareness of significant illness, possible hazards of treatments, lifelong consequences of injury, and the meaning of death.
Approach Strategies
Ask children to explain what they understand.
Provide as many choices as possible to increase the child’s sense of control.
Reassure the child that he or she has done nothing wrong and that necessary procedures are not punishment.
Anticipate and answer questions about long-term consequences (e.g., what the scar will look like, how long activities may be curtailed).
Adolescents
Major Fears
Loss of control.
Altered body image.
Separation from peer group.
Characteristics of Thinking
Able to think abstractly.
Tendency toward hyperresponsiveness to pain (reactions not always in proportion to event).
Little understanding of the structure and workings of the body.
Approach Strategies
When appropriate, allow adolescents to be a part of decision making about their care.
Give information sensitively.
Express how important their compliance and cooperation are to their treatment.
Be honest about consequences.
Use or teach coping mechanisms such as relaxation, deep breathing, and self-comforting talk.
From Sanders MJ: Mosby’s paramedic textbook, ed 2, St Louis, 2000, Mosby.
PEDIATRIC RESUSCITATION
The resuscitation of the pediatric patient involves knowledge and skills that each transport team member needs to have. Some transport programs use specialty teams to care for the child during transport. However, many pediatric transports are still provided by teams who do not specialize in pediatrics but have received additional education and training for working with this group of patients. Specialized pediatric critical care transport teams can bring expertise in the assessment and stabilization of critically ill pediatric patients and when available they should be considered for the transport of complex pediatric cases.
Pediatric resuscitation begins with the use of an algorithm that outlines pediatric advanced life support. The following is a more detailed description of the components of that algorithm and a discussion of the transport of the ill or injured pediatric patient.
Pediatric Airway Management/Respiratory Distress
The most important clinical skill for any clinician involved in pediatric care is the ability to assess respiratory distress and intervene appropriately. Most life-threatening complications in pediatric care are related to inadequate oxygenation and ventilation.
Pediatric Airway Anatomy
Pediatric airway anatomy differs from adult anatomy in the following ways (see Figure 11-14 in Airway Management Chapter):
▪ Airway diameter in children is smaller when compared with adults.
▪ The tongue (especially in infants) is proportionately larger.
▪ The larynx is anteriorly located in infants and children.
▪ The epiglottis is long and narrow and angled away from the trachea.
▪ The vocal cords are attached lower anteriorly.
▪ In children younger than 10 years, the narrowest portion of the trachea is at the cricoid process.
The clinical implications of these differences are as follows3:
▪ Small amount of edema or obstruction can markedly decrease air exchange.
▪ Posterior displacement of the tongue may cause airway obstruction.
▪ Control of the tongue with the laryngoscope may be difficult.
▪ The angle between the base of the tongue and the glottic opening is more acute, which makes straight blades more efficacious in visualization of the glottis.
▪ Control of the epiglottis with the laryngoscope blade may be more difficult.
▪ A blind endotracheal tube placement may become caught at the anterior commissure of the vocal cords.
▪ Properly sized endotracheal tubes have a minimal air leak with ventilation.
▪ Airway adjuncts for respiratory distress are listed in Box 33-2.
BOX 33-2
Airway Adjuncts for Respiratory Distress in the Pediatric Patient
Nasal cannula: Children rarely tolerate flows > 4 L/min. Not humidified.
Simple oxygen mask: Can deliver 35% to 60% O 2 at 6 to 10 L/min.
Nonrebreathing mask with reservoir: Can deliver 95% to 100% O 2 at 10 to 12 L/min.
Face tent or shield: Can deliver 40% O 2 at 15 L/min. Allows access to face without interruption of oxygen flow.
Oxygen hood: Plastic shell that encompasses the child’s head. Can deliver 80% to 90% O 2 at 10 to 15 L/min. Usually not large enough for children over 1 year old.
Oropharyngeal airway: A plastic flange that displaces the tongue from the posterior pharynx and provides an oral channel for ventilation and suction. The oral airway should be placed with a tongue depressor and direct visualization in the unconscious child in whom other airway maneuvers (jaw thrust and chin lift) have been unsuccessful at opening the airway. The proper size is determined with external measurement. With the flange at the level of the mouth, the tip should reach the angle of the jaw. Airways range from 4 to 10 cm in length.
Nasopharyngeal airway: A plastic or rubber tube that provides a conduit for air or oxygen from the nares to the posterior pharynx. It also allows for suctioning from the posterior pharynx. These airways are better tolerated in responsive patients. Proper size is again determined externally. The airway is approximated to equal the length from the tip of the nose to the tragus of the ear. A properly sized nasopharyngeal airway should not cause blanching of the external nares. These airways should be lubricated before placement.
Initial Management of Respiratory Distress/Arrest in the Pediatric Patient
▪ Open the airway. This can be accomplished with a jaw thrust or chin lift maneuver.
▪ Support breathing. This can be accomplished with any of the preceding adjuncts dependent on clinical severity of the respiratory distress.
Advanced Management of Respiratory Distress in the Pediatric Patient
Some patients may present with or progress to respiratory distress and need more aggressive support. These patients can be supported with bag-valve-mask (BVM) ventilation (Box 33-3) with or without endotracheal intubation. A pediatric resuscitation bag is shown in Figure 33-1.
BOX 33-3




Bag-Valve-Mask Ventilation
• Bag-valve-mask ventilation is a two-handed technique or preferably a two-person technique. With one hand or person securing the mask to the child’s face, the other provides bag ventilation.
• The technique is best performed with proper positioning. The child should be managed with a head tilt/chin lift maneuver while care is taken not to depress the submental area. Depression of the submental area may cause airway obstruction. Patients with suspected cervical spine injury should be managed with the cervical spine in a neutral position. Infants are often best managed in a neutral sniffing position, whereas toddlers benefit from a roll or towel placed under the head and neck to provide optimal airway patency. A variety of head and neck positions may be attempted to find the optimal position for effective ventilation.
• All bag-valve-mask ventilation should be provided with 100% oxygen, which is best achieved with the use of self-inflating bag-valve devices with an attached reservoir. Anesthesia bags may also be used but require greater training and experience to use successfully.
• An oropharyngeal or nasopharyngeal airway (depending on the patient’s level of consciousness) is helpful in providing more effective oxygenation/ventilation.
• Gastric distention is common during bag-valve-mask ventilation. This distention may worsen respiratory embarrassment and lead to emesis. Relief of this distention with a gastric tube is extremely important in the pediatric population.
• In the unconscious or extremely sedated patient, application of cricoid pressure (Sellick’s maneuver) may limit gastric distention and passive regurgitation.
• A resuscitation bag should not have a pop-off valve or one that is easily occluded for proper ventilation of patients with poor lung compliance or airway resistance.
• A manometer that attaches to the self-inflating bag can be helpful in assessment of pressure ventilation during resuscitation.
 |
| FIGURE 33-1 Pediatric resuscitation bags. |
Endotracheal Intubation
Endotracheal intubation is the most effective and reliable method of airway control for a variety of reasons, 1.2.3.4. and 5. including:
▪ The airway can be isolated, which ensures adequate ventilation and oxygen delivery.
▪ The potential for aspiration is decreased.
▪ Ventilations with chest compressions can be provided more efficiently.
▪ Inspiratory times and pressures can be controlled.
▪ Positive end expiratory pressure (PEEP) can be delivered.
▪ Endotracheal medications can be administered when access cannot be achieved.
▪ Pulmonary toilet can be accomplished.
▪ Functional or anatomic airway obstruction.
▪ Loss of airway protective reflexes.
▪ Excessive work of breathing, which may lead to fatigue or respiratory insufficiency.
▪ Need for high inspiratory pressures or PEEP.
▪ Need for mechanical ventilatory support.
▪ Potential for any of the preceding if patient transport is anticipated.
▪ As a route for resuscitative medications when access cannot be achieved.
Endotracheal intubation is a skill that requires as much clinical judgment as it does manual skill. Pediatric practitioners must always assess for and anticipate respiratory distress. The ability to determine which patients will need aggressive ventilatory support is an indispensable talent. The cricoid process is the narrowest portion of the trachea in children less than 8 to 10 years of ages. Thus, uncuffed endotracheal tubes are the most appropriate choice in this group (Figure 33-2). However, in certain circumstances, such as a near drowning, where lung compliance may be poor, a cuffed tube may be indicated. If a cuffed tube is used by the transport team, they must pay attention to the endotracheal tube size, the position of the tube, and the cuff inflation pressure. The cuff inflation pressure should be kept less than 20 cm of water. 3 A variety of ways are used for selection of proper endotracheal tube size, including3:
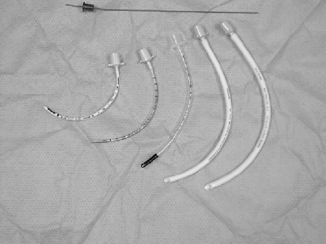 |
| FIGURE 33-2 Pediatric uncuffed endotracheal tubes. |
▪ Matching the outside diameter of the endotracheal tube to the child’s little finger.
▪ Matching the outside diameter of the endotracheal tube to the child’s nares.
▪ Use of length-based resuscitation tapes (Broselow tapes) reliable to approximately 35 kg.
▪ For children older than 2 years, the formulas:
or
or
Multiplying the internal diameter of the endotracheal tube (ET) by 3 can approximate the proper depth of endotracheal tube placement (i.e., a 3.5-mm ET × 3 is inserted 10.5 cm).
Preparation for endotracheal intubation is the most overlooked but often the most important part of the procedure. Proper preparation for problems that may arise can often prevent life-threatening complications during this procedure. The necessary equipment is listed in Box 33-4.
BOX 33-4
Equipment Necessary for Intubation
• Oxygen delivery system
• Bag-valve resuscitation bag without pop-off valve
• Resuscitation masks of various pediatric sizes
• Oral and nasopharyngeal airways of various pediatric sizes
• Suction devices, including pediatric-sized catheters
• Pulse oximeter with pediatric probes
• Cardiac monitor
• If sedation and paralytics are used, rescue medications (i.e., naloxone) should also be available
• Pediatric endotracheal tubes (Figure 33-2) and pediatric laryngoscope blades
• Pediatric stylettes
• End-tidal CO 2 detectors (disposable or in line)
• Securing tape or device
Immediately after intubation, proper tube placement can be verified clinically with a variety of means:
▪ Observation of symmetric chest movement.
▪ Auscultation of bilateral breath sounds high in the axillae.
▪ Absence of breath sounds over the stomach.
▪ Positive end-tidal CO 2 readings via colormetric detectors or capnography.
▪ Chest radiograph results, when clinically possible, should verify proper tube placement.
Esophageal obturator airways and oxygen-powered breathing devices are both discouraged in the pediatric population because of variability in patient sizes. 1.2.3. and 4.
Loading and unloading an intubated child into an aircraft or ground vehicle can place a child at risk of extubation. If change is seen in the child’s condition, the mnemonic DOPE may be of help in identification of a problem. The components include3,5:
D: Displacement of the tube from the trachea.
O: Obstruction of the tube.
P: Pneumothorax.
E: Equipment failure.
Needle Cricothyroidotomy
A rare occurrence in the pediatric population is the necessity for control of the airway via surgical means. 3,5 A surgical airway can be placed through the cricothyroid membrane on children over the age of 11 years (see Chapter 11), but needle cricothyroidotomy is recommended for children younger than this (Figure 33-3).
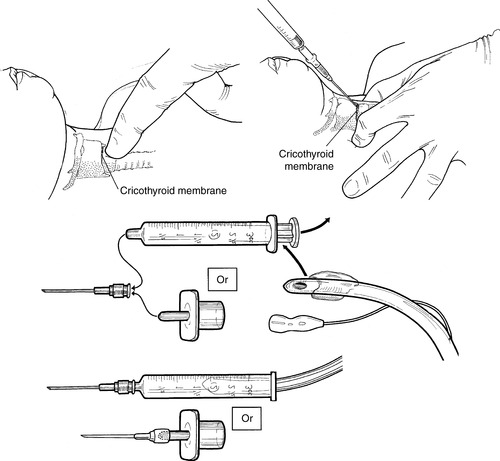 |
| FIGURE 33-3 Needle cricothyrotomy. (From Dieckmann R, et al: Pediatric emergency and critical care procedures, St Louis, 1997, Mosby.) |
Indications for needle cricothyroidotomy include:
▪ Complete airway obstruction.
▪ Severe orofacial injuries.
▪ Laryngeal transection.
▪ Inability to secure the airway with less invasive means.
The procedure for needle cricothyroidotomy is shown in Box 33-5.
BOX 33-5
Needle Cricothyroidotomy
1. Place the patient in a supine position.
2. Assemble a no. 14-gauge, 8.5-cm, over-the-needle catheter to a 10-mL syringe.
3. Surgically prepare the neck with antiseptic swabs.
4. Palpate the cricothyroid membrane between the thyroid and cricoid cartilage.
5. Stabilize the trachea with the thumb and forefinger to prevent lateral movement.
6. Puncture the skin in the midline over the cricothyroid membrane with the no. 14-gauge needle attached to the syringe. A small incision with a no. 11 blade may facilitate passage of the needle.
7. Direct the needle at a 45-degree angle caudally.
8. Carefully insert the needle into the lower half of the cricothyroid membrane, aspirating as the needle is advanced.
9. Aspiration of air signifies entry into the tracheal lumen.
10. Remove the syringe and stylette while gently advancing the catheter downward into position, taking care not to perforate the posterior trachea.
11. Oxygen can then be delivered in a variety of ways. Commercial jet insufflators are available for this purpose. Oxygen can also be supplied by attaching the adapter from a no. 3.0 endotracheal tube to the catheter and ventilating with a resuscitation bag. Finally, oxygen tubing can be cut with a hole toward the end of the tubing, which is then attached to the catheter hub. Once attached to an oxygen source of 50 psi or greater, oxygen can be delivered by occluding the hole with your thumb. Regardless of the oxygen delivery source, inspiration should be provided for 1 second while passive exhalation is provided for 4 seconds.
Complications of needle cricothyroidotomy include:
▪ Inadequate ventilation that leads to hypoxia and death.
▪ Aspiration (blood).
▪ Esophageal laceration.
▪ Hematoma.
▪ Posterior tracheal wall perforation.
▪ Subcutaneous or mediastinal emphysema.
▪ Thyroid perforation.
Needle cricothyroidotomy does not protect the patient’s airway from passive aspiration. Also, because of its limited lumen size, it is more effective in oxygenation than in ventilation. Needle cricothyroidotomy is a temporary measure until endotracheal tube placement or removal of the obstruction can be achieved.
SELECTED DIAGNOSES WITH RESPIRATORY DISTRESS IN THE PEDIATRIC POPULATION
Asthma
Asthma is the most common chronic illness in the pediatric population. The incidence rate of asthma continues to climb worldwide. A variety of environmental and immunologic factors appear to contribute to this increase.
Clinical Presentation
Expiratory wheezing is a hallmark finding in the patient with an acute asthmatic attack. In a severe asthma exacerbation, air exchange may be so limited that wheezing is not appreciated (e.g., silent chest). The patient also has sensitive but nonspecific signs of respiratory distress, including retractions, nasal flaring, cyanosis, accessory muscle use, and eventually altered mental status. Peak expiratory flow also is diminished and should be measured to gauge both acuity and patient’s response to therapy. Patient history may reveal past exacerbations that necessitated the use of home medications. The number and frequency of home treatments are important indicators of acuity. In addition, hospital admission, especially intensive care, is another important piece of history that should be collected in determination of the potential severity of the respiratory difficulty.
Treatment
The primary goals of asthma treatment are reversal of hypoxemia and control of contributing inflammatory responses. First-line therapy continues to be supplemental oxygen and the use of beta-adrenergic and anticholinergic aerosols. 18 The most common are Albuterol and ipratropium bromide delivered via a nebulizer.
The frequency of administration of these medications is a much-debated subject. As with any clinical intervention, patient response should be closely monitored. A key component of asthma therapy is the control of inflammation, which is now believed to contribute to chronic airway changes. Acute inflammation is controlled with steroid therapy.
Croup
Croup is the common term for a viral infection that affects the larynx but may extend into the trachea and bronchi.
Clinical Presentation
Patients generally present with a history of fever and coryza (cold symptoms). As the illness progresses, inspiratory stridor may be present as may a characteristic “barking” cough. If the inflammation extends to the bronchi, rhonchi and wheezing may also be present. Care must be taken to rule out epiglottitis and retropharyngeal abscess because the presentations can be similar. 8
Treatment
Treatment for croup is primarily supportive and centers on treatment of dehydration and the respiratory distress. In rare severe cases, upper airway edema or obstruction may necessitate endotracheal intubation for ventilation and airway protection. Medications include racemic epinephrine aerosols, intramuscular (IM) or oral (PO) dexamethasone, and prednisolone.
Epiglottitis
Epiglottitis is a rare but life-threatening bacterial infection of the epiglottis and surrounding structures. Epiglottitis has become increasingly rare with the advent of immunization for Haemophilus influenzae, which is the causative agent in 90% of epiglottitis cases. 8
Clinical Presentation
Epiglottitis is second only to croup as a cause for infectious stridor. The course of epiglottitis is differentiated from other presentations because of its abrupt nature. Symptoms often occur rapidly and cause parents to seek medical attention in 24 hours of the initial symptoms. Patients present with fever, stridor, labored respirations, and often drooling, because of supraglottic edema. The appearance of these children is also helpful in diagnosing of epiglottitis. They are often anxious and present in a classic tripod position, sitting forward with their arms supporting them with their jaws thrust forward. This position is assumed by the patient to increase air entry. Clinicians must recognize this presentation because of the life-threatening nature of airway involvement.
Treatment
The focus of treatment with epiglottitis is rapid recognition and treatment of airway obstruction. Patients in extremis must have the airway controlled before any other intervention, including laboratory work and intravenous access. Before dealing with these patients, creation of a well-defined epiglottitis algorithm is crucial. A lateral neck radiograph may be helpful in delineating epiglottitis from the much more common causes of stridor and respiratory distress. If endotracheal intubation is indicated, the support from anesthesiologist or ear, nose, and throat (ENT) staffs is invaluable. Use of the operating room with inhalation induction and rapid access to tracheostomy equipment is the optimal method of airway control. In situations without this support, endotracheal intubation should only be undertaken by staff capable of securing the airway, surgically if necessary. Airway control before transport is best for the patient with epiglottitis. Current antibiotic recommendations include cefuroxime, cefotaxime, and ceftriaxone. 18
All patients with epiglottitis need intensive care admission.
Foreign Body Aspiration
Aspiration of foreign bodies into the respiratory system can create difficult diagnostic challenges. Aspiration into the upper airway may be immediately life threatening with obvious clinical symptoms, whereas aspiration into the lower respiratory tract may have varying degrees of severity. Sixty-five percent of lethal aspirations occur before the age of 2 years, and special consideration for education should be given to parents of these children. Foods most frequently associated with aspiration are hot dogs, candy, nuts, and grapes.
Upper Airway Aspiration
Clinical Presentation
Patients with upper airway foreign body aspiration generally present in severe respiratory distress. The history includes rapid onset of stridor, tachypnea, and in some cases, total airway obstruction.
Treatment
Complete airway obstruction should be managed initially with basic life support (BLS) measures, such as the Heimlich maneuver in older children and chest thrusts in infants. If the child’s condition is apneic, attempts at ventilation should also be provided. Failure of BLS measures should be followed by laryngoscopic visualization and attempts at removal. Unresolved total upper airway obstruction is an indication for needle or surgical cricothyroidotomy, depending on the child’s age.
Lower Airway Aspiration
The majority of lower airway foreign body aspirations occur in children under 3 years of age. The difficulty in treatment of these aspirations is the wide range of presentations and the difficulty in imaging nonradioopaque objects. A high index of suspicion must be maintained for at-risk age groups (6 months to 3 years) with respiratory distress.
Clinical Presentation
As stated previously, presentations can range from essentially asymptomatic to severe respiratory distress. A careful history is often helpful in diagnosis. Common presentations include new-onset coughing and wheezing. Less than half of these events are diagnosed on the day of aspiration. If sought, a history of a recent choking or aspiration episode is usually found in 75% of cases.
Treatment
If an object is found with radiographic or if a strong likelihood of aspiration is found by history, bronchoscopy with removal of the aspirated object is the standard of care for these patients.
Bronchiolitis
Bronchiolitis is a lower respiratory tract infection (primarily viral) that is one of the more common causes of new-onset wheezing in children. Respiratory syncytial virus (RSV) is the causative agent in most cases, but Haemophilus parainfluenzae and Mycoplasma pneumoniae have also been isolated.
Clinical Presentation
Wheezing is the most common presenting symptom, often with an accompanying 2-day to 5-day course of coryza and cough. These patients are often tachypnic, with respiratory rates reaching 80 to 100 breaths/min in some cases. Nonspecific signs of respiratory distress such as nasal flaring and intercostal retractions are also present. Most cases occur in the winter months, with the majority of infections in children from ages 2 to 8 months. Apnea in children younger than 3 months is also characteristic of RSV infections. 8
Treatment
Once other causes for wheezing have been ruled out (asthma, foreign body aspiration, pneumonia), care is generally supportive. Supplemental oxygen, antipyretics, and adequate hydration are all helpful for patients in mild distress. Children may benefit from nebulized albuterol aerosols and oral albuterol solution. Oral albuterol solutions are not indicated for patients who do not respond to aerosol therapy. Corticosteroids are not indicated for the treatment of bronchiolitis. Patients in severe distress who are unresponsive to therapy may need intubation and mechanical ventilation. 8
Pneumonia
Pneumonia, an inflammation of the pulmonary parenchyma, can be caused by a variety of bacterial, fungal, and viral agents. Discussion of all of the causative agents is beyond the scope of this module, so this process is discussed in general terms.
Clinical Presentation
Bacterial pneumonia generally has a rapid onset with accompanying high fevers, chills, and cough. The patient with bacterial pneumonia may also have grunting respirations, decreased breath sounds, and tachypnea, which are all nonspecific signs. Viral pneumonia, in contrast, has a more gradual onset over 2 to 4 days with cough coryza and low-grade fevers. Patients with viral pneumonia may also have rales, grunting respirations, tachypnea, and decreased breath sounds. In truth, bacterial and viral pneumonia are difficult to distinguish based on clinical examination results alone. Leukocytosis over 15,000/mm is a more predominant finding in bacterial pneumonia and weighs against a viral diagnosis. 9,10 A chest radiograph can be helpful in diagnosis. Bacterial pneumonia often shows a lobar consolidation, whereas viral pneumonia causes hyperaeration or diffuse interstitial infiltrate without consolidation.
Treatment
Treatment involves supportive measures with appropriate antibiotic therapy for bacterial infections. Dehydration and hypoxia are common complications of pneumonia, so adequate intake, whether oral or intravenous, and supplemental oxygen may be essential. Antipyretics lower fevers and increase patient comfort. Drugs most commonly used in children for antipyretics include acetaminophen and ibuprofen. 18
Sensitivity to these drugs should be determined before administration. Currently, little data exist on the lower age limits for ibuprofen therapy, so caution should be used in younger children (<6 months). The practice of alternating these medications in patients is also being investigated. Supplemental oxygen for children in distress is indicated. As with other respiratory illnesses, some children may need intubation and mechanical ventilation, depending on the severity of pulmonary dysfunction. Streptococcus pneumoniae and H. influenzae remain the major bacterial causes for pediatric pneumonia. Medication therapy is dependent on the causative microorganism.
Children who need hospital admission for pneumonia include5:
▪ Children <1 year old.
▪ Patients with respiratory compromise.
▪ Patients with pleural effusion.
▪ Patients with pneumatocele.
▪ Patients with failure to respond to antibiotic therapy.
▪ Patients with dehydration.
Congenital Heart Disease and Metabolic Acidosis
Two other causes of acute respiratory distress in children that may be encountered by the transport team are congenital heart disease and metabolic acidosis.
Congenital Heart Disease
Because of varying rates of closure of the ductus arteriosus, clinical presentations of respiratory distress from congenital heart disease can be seen anywhere from a few days to 6 weeks after birth. The list of both cyanotic and acyanotic lesions that can cause respiratory distress in newborns is too lengthy for discussion in this chapter. Cardiac processes should be kept on the list of differential diagnoses for children in this age group. 5
Metabolic Acidosis
Tachypnea from metabolic acidosis is a common clinical finding in pediatric patients. Respiratory buffering of acidosis may be the most obvious clinical finding in these situations. Tachypnea without an obvious cardiac or respiratory source should be further investigated to rule out metabolic acidosis. 5
Causes of metabolic acidosis in children include:
▪ Diarrheal dehydration (most common cause).
▪ Diabetic ketoacidosis.
▪ Renal failure (acute or chronic).
▪ Inborn errors of metabolism.
▪ Poisons (salicylate, ethanol, methanol, ethylene glycol).
▪ Lactic acidosis (hypoxia, sepsis, shock).
▪ Hyperalimentation.
▪ Enteric fistulas.
▪ Ureterosigmoidostomy.
▪ Drugs (e.g., mafenide [Sulfamylon], ammonium chloride, amphotericin, acetazolamide).
▪ Dilution (rapid volume expansion).
Identification and management of the cause of the acidosis must occur quickly. Supplemental oxygen including intubation and mechanical ventilation may be necessary during the acute treatment phase of these disorders.
PEDIATRIC TRAUMA
Outside of the immediate perinatal period, trauma and accidents continue to be the leading cause of death in all pediatric age groups. Although this section focuses on specific injuries and treatment, education aimed at the prevention of these avoidable injuries should always be the focus for emergency care providers and transport team members.
Physiologic and Psychologic Considerations
Pediatric patients have several unique physiologic, psychologic, and anatomic characteristics that must be considered when dealing with the acutely injured child.
Size and Body Surface Area
Because of children’s smaller size and surface area, energy from traumatic injuries imparts more force per unit of body area. The relative lack of body fat, the decreased elasticity of connective tissue, and the close proximity of internal organs to surface tissue all increase the potential for multiple injuries in this population. Increased body surface area also lends itself to increased thermal loss. Hypothermia becomes a major clinical concern. 1.2.3.4.5.6. and 7.
Skeletal Structure
Incomplete calcification of the child’s skeleton predisposes children to underlying soft tissue and organ injury without obvious overlying bony deformity. Multiple growth centers in the pediatric skeleton may also have clinical implications in care. Skeletal fractures in children, especially in the thorax, should heighten clinical suspicion of a high-energy injury with resultant trauma to underlying structures. 1.2.3.4. and 5.
Psychologic
Children of different ages present with different emotional and developmental needs. Familiarity with these issues allows the clinician to tailor the clinical approach and anticipate the patient’s needs. Injuries and stress may cause regression in psychologic behavior, which in turn can complicate clinical management.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






