CHAPTER 20. Burn Trauma
Heather McLellan
Competencies
1. Identify the pathophysiology of burn wounds.
2. Describe the initial assessment of the patient with burns.
3. Describe the management of the patient with burns during the transport process.
ETIOLOGY AND EPIDEMIOLOGY
A burn wound is an injury caused by the interaction of an energy form (thermal, chemical, electrical, or radiation) and biologic matter. Most burns are thermal: flame burns, scalds, or contacts with hot substances (Figure 20-1). Frostbite is often included in this category; however, no current statistics are available regarding its incidence rate.
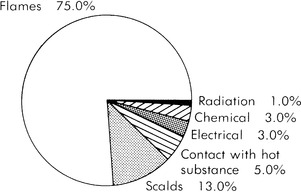 |
| FIGURE 20-1 Causes of burn injuries. |
Chemical injuries occur when the source of energy contacted is capable of causing tissue necrosis. Examples of necrosis-causing chemicals include strong acids, which cause coagulation necrosis from protein precipitation, and alkalis, which cause liquefaction necrosis.
Electrical burns occur when contact is made with a high-voltage current. The current itself is not considered to have any thermal properties while traveling through material of low resistance; however, the potential energy of the current is transferred into thermal energy when it meets resistance with biologic tissue and is dispersed throughout that tissue. This action is accomplished primarily by conduction.
Radiation injuries can be caused by both ionizing and nonionizing radiation. Radiation injuries make up a small percentage of burn injuries.
Approximately 700,000 individuals receive medical treatment for thermal burn injuries in the United States and Canada each year. 2,3 Of these, 40,000 need hospitalization, and 4000 die. 2,3,11 The World Health Organization estimates that 322,000 fire-related deaths occurred worldwide in 2002, with most of these in developing countries. 23 The survival rate from major burns has increased significantly and is now up to 94.4%. 2
Estimates are that 500 deaths per year can be attributed to electrical and lightning injuries. 2,3 Contact with electricity accounts for between 3% and 5% of all burns treated in the United States each year. All ages are affected, with the most common victims those who work with electricity professionally. The age group with the greatest electrical injury rate is infancy to 4 years of age. 2,3,11 These injuries are primarily caused by contact with exposed electrical cords and outlets. The second peak appears from ages 20 to 25 years. Those injuries occur predominately in the male population and are caused by work and industrial accidents. An estimated 150 people are killed by lightning each year in the United States. Most lightning injuries occur in the daytime hours of the summer and fall months. The outdoors enthusiast, athlete, camper, farmer, or golfer is more prone to lightning injury because of more frequent exposure to the elements. 2,3
PATHOPHYSIOLOGY OF BURN WOUNDS
The causes of burns may vary, but the local and systemic responses are generally similar. The extent of the injury is influenced by three factors: (1) the intensity of the energy source; (2) the duration of exposure to the energy source; and (3) the conductance of the tissue exposed. The relationship between the duration of exposure to and intensity of the energy source is significant in determining the magnitude of the injury. Increased intensity with increased exposure causes increased amounts of tissue damage. Conductance can be affected by the presence of hair, water content of the tissues, and thickness and pigmentation of the skin. Significant factors that determine severity of electrical injury are: (1) voltage and amperage; (2) resistance of internal body structure and tissue; (3) type and pathway of current; and (4) duration and intensity of contact. 8,24
For a better understanding of the pathophysiology of burn wounds, one must know the anatomy and functions of the skin. Skin is composed of two layers: the epidermis and the dermis. The epidermis, the outer layer, consists of the basement layer of cells that migrate upward to become surface keratin. The inner layer, the dermis, consists of collagen and elastic fibers and contains hair follicles, sweat and sebaceous glands, nerve endings, and blood vessels. Beneath the cutaneous layers is a layer of subcutaneous tissue that consists primarily of connective tissue and fat deposits; this layer overlies muscle and bone.
The primary functions of skin include: (1) regulation of body temperature through dilation and constriction of the dermal and subcuticular vessels in response to environmental temperature; (2) protection against injury and bacterial invasion; (3) prevention of body fluid loss; and (4) sensory contact with the environment. A burn injury interrupts and compromises these functions.
Thermal Burn Injury
Responses of the body to thermal injury consist of varying degrees of tissue damage, cellular impairment, and fluid shifts. Locally, a brief initial decrease in blood flow to the area occurs, followed by a marked increase in arteriolar vasodilation. Release of toxic mediators of inflammation is activated with the burn, creating a complex circulatory dysfunction. These mediators include histamine, serotonin, kinins, oxygen free radicals, prostaglandins, thromboxanes, and interleukins. Although inflammatory activity is a necessary part of the healing process, excess production of mediators, especially oxidants and proteases, causes more capillary endothelial and skin cell damage. 10,13,17,20 This increases capillary permeability, particularly once the burned area reaches a size that is approximately 30% of the body surface area, which causes intravascular fluid loss and wound edema.
Hypoproteinemia that results from the increase in capillary permeability aggravates edema in the nonburned tissue. Myocardial contractility is thought to be decreased because of a release of tumor necrosis factor-alpha. Insensible fluid loss from the burn wound increases the basal metabolic rate and, along with fluid shift, leads to hypovolemia, hypotension, and inadequate end organ perfusion. 10,17
The decrease in circulating plasma causes an increase in hematocrit, which in turn can cause hemoglobinuria when the hemoglobin is filtered through the kidneys and can contribute to renal failure. Increased peripheral vascular resistance leads to a decrease in venous return to the heart, decreased cardiac output, impaired tissue perfusion, and a decrease in renal perfusion, which can also contribute to renal failure. 10,13,18
A decrease in splanchnic blood flow occurs, which increases the occurrence of mucosal hemorrhages in the stomach and duodenum. An increased risk of sepsis from bacterial translocation may also be seen as a result of diminished mucosal barrier function in the intestine. Patients with burns on more than 20% of the body surface area (BSA) can also have adynamic ileus, which can be of special concern for the patient transported by air at high altitudes.
Decreased immune response in both cell-mediated and humoral pathways increases the patient’s susceptibility to infection. 10,17 Thus, the transport team must take extra precautions to prevent further injury to the burn victim through exposure to contaminated environments.
Thermal burns and pregnancy should be considered in any female of the reproductive age group. The outcome of the pregnancy is determined by the extent of the mother’s burn injury. Spontaneous abortions can be anticipated with burns greater than or equal to 60% percent of BSA. The incidence rate of preterm labor or spontaneous abortion is reduced with adequate oxygenation, fluid resuscitation, and electrolyte imbalance correction. 2,3
Electrical Injury
Electrons flowing through the body produce injury by depolarizing muscles and nerves. They can also disrupt electrical rhythms in the brain and heart. Electrical energy is also converted to thermal energy when it meets resistance from tissues. Resistance is described as the degree of hindrance to electron flow. Those tissues that contain the most electrolyte media, nerves, blood vessels, and muscles transmit current most easily because they have the least resistance. Tissues, tendons, and fat are most resistant and do not allow conduction, which causes burning and surrounding deep muscle damage. The intensity of the electrical current that passes through victims shows a direct correlation to the tissue damage produced. 10,18,24
Voltage is defined as the force with which the electrical movement occurs. High-voltage injuries (>1000 V) and low-voltage injuries (<1000 V) are both common, and either type can cause death. High amounts of electrical voltage and amount cause more significant injury to the patient and result in tissue charring and extensive blistering. The type of current, alternating (AC) or direct (DC), can also determine the significance of injury. 10,18,24 Alternating current produces a tetanic contraction of muscles that “freezes” the victim to the source. This reaction is not seen with direct current; therefore, low-voltage AC exposure, such as to a household current of 110 V, can be more dangerous than a low-voltage direct current. The alternating current also has a greater potential to cause ventricular fibrillation from tetanic chest muscle contractions (Table 20-1).
| mAmps | Effect |
|---|---|
| 1-2 | Tingling of skin |
| 15-20 | Muscle tetany: the “let go” current |
| 50-90 | Respiratory arrest (if directed through the medulla) |
| 90-250 | Ventricular fibrillation (if the myocardium is transversed) |
The current pathway is critical because it may determine the severity of injury. Current passing through the head and thorax involves the respiratory center or heart and is likely to produce instant death. Current passing from hand to foot may not affect the respiratory center but may damage the heart. From the entry point, the electrical current follows the path of least resistance, causing one or more tracks of damage. The energy collects at the grounding point, causing significant tissue necrosis, and subsequently causing an explosive exit through the skin. 10,24 The mortality rate of hand-to-hand current passage is reported to be 60%; hand-to-foot current passage is 20%; and foot-to-foot current passage is 5%. Direct current has been noted to leave a discrete exit wound (Figure 20-2), whereas alternating current tends to be more explosive (Figure 20-3).
 |
| FIGURE 20-2 Exit wound from direct current. |
 |
| FIGURE 20-3 Exit wound from alternating current. |
With electrical injury, flame burns occur as the result of the ignition of clothing or other items by the current. These wounds could be severe when the victim is unconscious and has a long exposure to the flame. The ignition of clothing usually occurs with high-voltage injuries that are greater than 350 to 1000 V. Frequently, high-voltage injuries cause combinations of all types of electrical burns, and determination of the proper course of therapy may become difficult. 10,17,18,24
As electrical current passes through the body, severe dysrhythmia may occur. Ventricular fibrillation is frequently induced as a 60-cycle alternating current passes through the ventricles. Direct current injuries predominantly result in asystole by depolarizing the entire myocardium. In addition to those fatal rhythms, other dysrhythmia may occur, such as atrial fibrillation, sinus bradycardia, ventricular and atrial ectopy, supraventricular tachycardia, bundle branch block, and first-degree and second-degree block. Coronary artery spasm, coronary endarteritis, and direct myocardial injury are thought to be the cause of this dysrhythmia. Damage to the myocardium, including myocardial rupture, is also a result of an electrical injury. These injuries are believed to be caused by the heat generated by the current. Myocardial damage manifests itself in the same manner as the injury induced by ischemia.
The skull is a common entry point of electrical current; thus, the brain stem is often affected, which can lead to respiratory arrest and potential cerebral hemorrhage or edema. 8,24 Nervous system tissue is an excellent conductor of electrical current, so central nervous damage is not uncommon. Effects of electrical injury to the central nervous system are manifested by unconsciousness, seizures, disorientation, or amnesia. Other neurologic complications that have been identified are spinal cord injuries, particularly those associated with electrical current traversing a hand-to-hand or head-to-foot course, and local nerve damage with peripheral neuropathies. Incomplete spinal cord transection is a common delayed lesion caused by damage to the spinal cord by the heat of the electrical current or by blunt trauma from falls or severe tetanic contractions of the muscles surrounding the cord. Headaches, cerebellar dysfunction, optic atrophy, ascending paralysis, and transverse myelitis are neurological sequelae that are delayed. 8,24
Extensive necrosis over vessels resulting from electrical injury may precipitate delayed hemorrhage from large blood vessels. Arterial thrombosis, deep vein thrombosis, and abdominal aortic aneurysms may also result. A major vessel that has been only partially damaged may cause difficulty with homeostasis in open or newly closed wounds. Injuries to the abdominal cavity commonly identified after electrocution are submucosal hemorrhages in the bowel, liver failure, pancreatitis, nausea and vomiting, paralytic ileus, and various forms and degrees of ulcerative disease. 8,24
Long bone fractures and dislocations and vertebral fractures are caused by the rigorous tetanic muscle contractions that occur. Bilateral scapular fractures have been reported from exposure to a 440-V, 60-cycle current passing briefly through a person’s upper extremities. Amputations have also been the result of severe muscle contractions caused by high-voltage electrical injuries. 8,10,24
Immediate burns to the eyes, optic atrophy, and the development of cataracts are not uncommon, particularly if the entrance or exit wounds appear on or around the head. Cataracts may develop unilaterally or bilaterally and occur as soon as 4 months or as late as 3 years after the injury.
For the pregnant patient, the hand-to-foot pathway of current invariably passes through the fetus. The amniotic fluid and abundant uteroplacental vascularity have a low resistance to current flow, and the fetus becomes an easy victim of electrical injuries. Regardless of how slight the injury may appear, the mother must be transported to a hospital in which extensive fetal monitoring can be done.
Acute renal failure is a complication that results from direct damage to the kidney by the electrical current or blunt trauma to the kidney or from myoglobinuria. Myoglobin is released as a result of extensive muscle necrosis, and myoglobinuria is proportionate to the amount of muscle damage incurred. 18
ASSESSMENT
The assessment of the patient with burn injuries begins with the ABCDEs of the primary assessment. Burn wounds are often dramatic in appearance and can lure the transport team’s attention away from more immediate life-threatening problems.
The subjective assessment includes as thorough a history as circumstances permit. The history should include the mechanism and time of the injury and a description of the surrounding environment, such as injuries incurred in an enclosed space, the presence of noxious chemicals, the possibility of smoke inhalation, and any related trauma. The time of the injury is especially important in the calculation of fluid resuscitation. Information regarding tetanus immunization status should also be obtained with the history. 12
Thermal Burns
Assessment of a thermal burn includes estimating the burn size and depth, associated inhalation injuries, and calculation of fluid resuscitation needs. The size of a burn wound is most frequently estimated with the rule of nines12 method, which divides the body into multiples of 9% (Figure 20-4). A more accurate assessment can be made of the burn injury, especially for pediatric patients, with a Lund and Browder chart, 12 which takes into account growth changes (Figure 20-5). For estimating scatter burns, a fairly accurate approximation can be made with the patient’s entire palm size to represent 1% of the total BSA and visualization of that palm over the burned area. Use of electronic assessment tools is becoming popular because these tools not only increase the accuracy of assessment but also enhance continuity of care as they are easily transmitted to each level of caregiver. 15,25
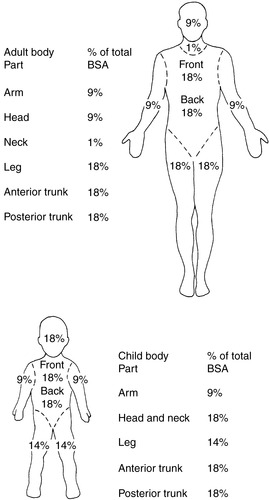 |
| FIGURE 20-4 Rule of nines. |
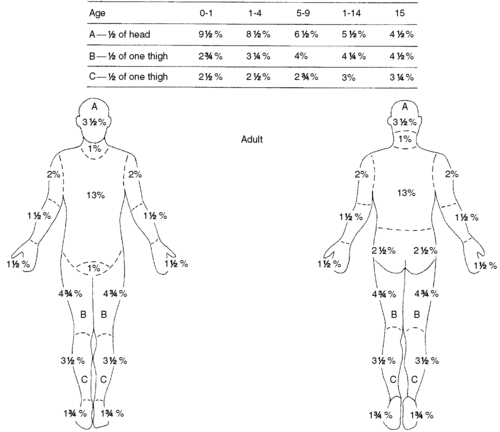 |
| FIGURE 20-5 Lund and Browder method for calculating percentage of burned body surface area. |
Primarily, the temperature of the burning agent, the duration of exposure, and the conductance of the tissue involved determine the depth of a thermal burn wound. Initially, the estimation of injury depth is difficult.
Burn wounds typically present in a bull’s-eye pattern, with each ring representing a different zone of intensity. A superficial partial-thickness injury, formerly known as a first-degree burn, involves the epidermis and is represented by the outermost ring, the zone of hyperemia. This type of injury is usually red in appearance, is painful, and heals in 7 to 10 days. 10,12,17,20
A deep partial-thickness injury, formerly known as a second-degree burn, involves both the epidermis and dermis. This burn is seen as the middle ring and is called the zone of stasis, which is potentially viable tissue, despite the heat injury. This wound is characterized by reddened skin that is wet or blistered, is painful, and generally heals in 14 to 21 days. However, these diagnostic signs can be misleading because a full-thickness burn is possible under a blister. 10,12,17,20
Full-thickness injuries are the center ring, called the zone of coagulation. These injuries, formerly known as third-degree injuries, encompass wounds that consist of both dermal layers and extend into the subcutaneous tissue. Subdermal burns destroy both layers of tissue and extend into fat, tendon, muscle, and bone. Full-thickness injuries are charred and leathery in appearance or white and waxy, with thrombosed vessels that are easily visible under the surface. 10,12,17,20 They are painless because of destruction of sensory nerves, with no epithelial growth for healing. These wounds necessitate grafting.
Inhalation Injuries with Thermal Burns
The three types of identifiable inhalation injuries are: (1) asphyxiation from carbon monoxide poisoning; (2) supraglottic injury, which is primarily thermal in nature; and (3) infraglottic injury, which is primarily chemical. Inhalation injuries are the primary cause of death at the scene of a burn injury, and they contribute significantly to the overall morbidity and mortality rates of burn patients. 9,10,14,17
Carbon monoxide intoxication occurs because the affinity for carbon monoxide to hemoglobin is markedly greater than that of oxygen (approximately 12 times greater); therefore, the carbon monoxide displaces the oxygen and binds with the available hemoglobin to form carboxyhemoglobin, with resultant hypoxia. The signs and symptoms of carbon monoxide poisoning include pink to cherry-red skin, tachycardia, tachypnea, headache, dizziness, and nausea. Carboxyhemoglobin levels are helpful to determine the management approach for these patients. Levels of 0 to 15% rarely cause symptoms and may be normal, especially for a heavy smoker. Levels of 15% to 40% cause varying amounts of central nervous system disturbances, such as confusion and headache. Levels greater than 40% can cause mental depression and coma. Any patient with suspected carbon monoxide injury should be given 100% oxygen. 9,10,14 The treatment of carbon monoxide poisoning is discussed in both Chapter 24, Pulmonary Emergencies, and Chapter 30, Toxicologic Emergencies.
Supraglottic injury should be suspected when facial burns, singed facial hair, or carbonaceous sputum are present. Other signs and symptoms of upper airway injury include presence of redness or blistering in the posterior pharynx, stridor, wheezing, bronchorrhea, or any other sign of respiratory difficulty. Absence of these signs and symptoms initially does not exclude the possibility of inhalation injury because upper airway edema may not be present until after the onset of fluid resuscitation.
Infraglottic injury is often more difficult to ascertain because the injury is progressive in nature. It is caused by the inhalation of the particulate byproducts of combustion. It is manifested by an increase in both pulmonary vascular resistance and pulmonary capillary permeability, which causes pulmonary edema. The primary symptom is hypoxemia that is resistant to oxygen therapy. Inhalation injuries are unpredictable in onset. Any patient with suspected inhalation injuries should be closely observed for 24 hours for onset of respiratory complications. Some experts advocate fiber optic bronchoscopy or xenon ventilation-perfusion scanning to identify inhalation injury earlier. 9,10,14,17
Electrical Injuries
If the patient actually becomes part of the circuit, they may incur direct contact burns. These wounds may appear devastating, and they frequently resemble a crush injury rather than a burn (Figure 20-6). The most common point of entry is the hand or skull, and the most common exit site is the feet. The sizes of these entrance and exit wounds are no real indicator of the amount of damage done to internal tissue. When the current leaves the body on its course to the ground, arc burns occur. 8,24 The arcing current produces extremely high energies, ranging from 3000 °C to 20,000 °C. Wounds are deeper because the heat intensity is closer to the body. Deep partial thickness and full thickness thermal burns may be indistinguishable when the heat source is more distant from the body.
 Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|



