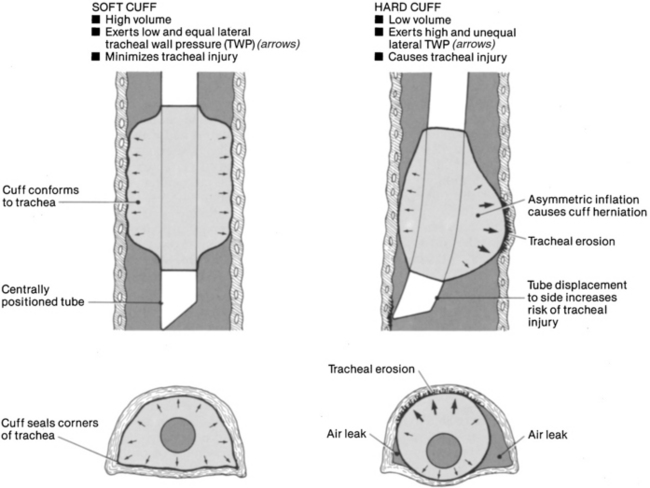
PROCEDURE 13 • The tracheal tube cuff is an inflatable balloon that surrounds the shaft of the tracheal tube near its distal end. When inflated, the cuff presses against the tracheal wall to prevent air leakage and pressure loss from the lungs. • Appropriate cuff care helps prevent major pulmonary aspirations, prepare for tracheal extubation, decrease the risk of inadvertent extubation, provide a patent airway for ventilation and removal of secretions, and decrease the risk of hospital-acquired infections. • Although a variety of endotracheal and tracheal tubes exists, the most desirable tube provides a maximum airway seal with minimal tracheal wall pressure, with a high-volume low-pressure cuff (Fig. 13-1). This cuff has a relatively large inflation volume that requires lower filling pressure to obtain a seal (<25 mm Hg or 34 cm H2O). Note: 1 mm Hg = 1.36 cm H2O, or 1 cm H2O = 0.74 mm Hg. • High-volume low-pressure cuffs allow a large surface area to come into contact with the tracheal wall, distributing the pressure over a much greater area. The older cuff design (low-volume high-pressure) may require 40 mm Hg (54.4 cm H2O) to obtain an effective seal and is undesirable. • The amount of pressure and volume necessary to obtain a seal and prevent mucosal damage depends on tube size and design, cuff configuration, mode of ventilation, and the patient’s arterial blood pressure. • A variety of devices are available to measure cuff pressures, including bedside sphygmomanometers, special aneroid cuff manometers, and electronic cuff pressure devices. Ideally, the cuff pressures should be between 20 and 25 mm Hg and still meet the goals of cuff use. Tracheal capillary perfusion pressure is 25 to 35 mm Hg for patients with normotensive conditions. Lower cuff pressures are associated with less mucosal damage but also are associated with silent aspiration, which has been shown to be more prevalent at cuff pressures less than 20 mm Hg.1,6,8 • Two techniques, minimal leak technique (MLT) and minimal occlusion volume (MOV), are used to inflate and monitor air in the cuff. • Each technique has distinct advantages. MLT decreases tracheal mucosal injury and assists in mobilizing secretions forward into the pharynx. MOV is used if the patient needs a seal to provide adequate ventilation or is at risk for aspiration.4,8 • Although rare since the use of high-volume low-pressure devices became common, the adverse effects of tracheal tube cuff inflation include tracheal stenosis, necrosis, tracheoesophageal fistulas, and tracheomalacia. These complications may be more likely to occur in conditions that adversely affect tissue response to mucosal injury, such as hypotension. Two major mechanisms are mainly responsible for airway damage: tube movement and pressure. Duration of intubation also plays a significant role.4,8
Tracheal Tube Cuff Care
PREREQUISITE NURSING KNOWLEDGE
 The MLT involves air inflation of the tube cuff until any leak stops; then, a small amount of air is removed slowly until a small leak is heard on inspiration. Problems with this technique include difficulty maintaining positive end expiratory pressure (PEEP), aspiration around the cuff, and increased movement of the tube in the trachea during cuff deflation.2,4,5,7,8 Aspiration may be prevented with deep pharyngeal suctioning before use of the MLT.
The MLT involves air inflation of the tube cuff until any leak stops; then, a small amount of air is removed slowly until a small leak is heard on inspiration. Problems with this technique include difficulty maintaining positive end expiratory pressure (PEEP), aspiration around the cuff, and increased movement of the tube in the trachea during cuff deflation.2,4,5,7,8 Aspiration may be prevented with deep pharyngeal suctioning before use of the MLT.
 The MOV consists of injection of air into the cuff until no leak is heard, then withdrawal of the air until a small leak is heard on inspiration, and then addition of more air until no leak is heard on inspiration.2,4,5,7,8
The MOV consists of injection of air into the cuff until no leak is heard, then withdrawal of the air until a small leak is heard on inspiration, and then addition of more air until no leak is heard on inspiration.2,4,5,7,8
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


13: Tracheal Tube Cuff Care