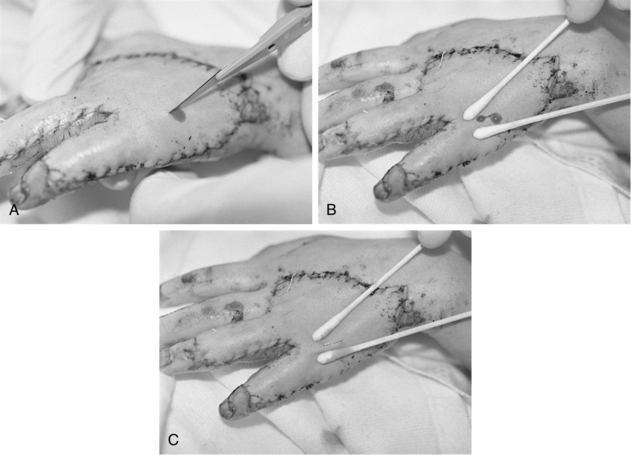
PROCEDURE 121 • Skin grafts, also called autografts, are sections of skin used to replace missing skin on a patient’s body. An autograft is created by taking a donor graft from one area of a patient’s body and transplanting it to a different area of the same patient’s body. It involves the surgical removal of a section of the epidermis and a portion of the dermis.1,8 This removal results in a new exposed wound area from which the donor graft was taken, called the donor site. The graft, a split-thickness skin graft (STSG), is applied over a clean, surgically excised wound that has been débrided of all nonviable tissue. • An autograft is the only permanent treatment that can heal a large, full-thickness wound. Autografts may also be used to heal partial-thickness wounds with faster closure of the wound. The original wounds may be from a variety of causes (burns, infections, traumatic injury, etc). • The autograft is harvested from an appropriate donor site on the patient’s body with a dermatome, a surgical instrument that shaves layers of skin at different depths to be grafted over the wound bed. • The STSG is commonly meshed (Fig. 121-1) so that it can be stretched to cover approximately 1.5 to 9 times more surface area than the original donor site. The ability to stretch the donor graft is important when there is a limited availability of suitable donor sites or when the wound area that requires grafting is extensive. Meshing the donor skin creates spaces, or interstices, that allow for fluid to escape, which can assist with graft adherence. • Negative-pressure wound therapy (NPWT) is a mechanical wound care treatment that uses controlled negative pressure (via a machine, tubing, and sealed dressing) to accelerate wound healing. NPWT can also be used to enhance incorporation of a STSG mesh graft. The NPWT dressing is placed over the graft during surgery. A nonadherent dressing is used as a barrier for the graft to protect the graft from trauma and decrease overgrowth of granulation tissue formation.1 • Nonmeshed grafts, or sheet grafts, are used on the face, hands, and some joints because of cosmetic and functional concerns related to appearance and increased shrinkage. • A sheet graft covers the same amount of surface area as the donor site. Pockets of serous fluid or blood tend to accumulate under these grafts (the interstices of meshed grafts allow the fluid to escape) and separate the graft from the wound bed, which is vital for blood supply, resulting in failure of the graft to adhere or “take” to the wound bed. Evacuation of this fluid is imperative. Sheet grafts on the face, neck, and hands are generally inspected within the first 12 to 24 hours to look for fluid collections or graft dislodgement. If the sheet graft has been in place for less than 48 hours and the fluid is near the edge of sheet graft, the fluid can be rolled to the edge and out (Fig. 121-2).2 Figure 121-2 A, A no. 11 surgical blade and cotton-tipped applicator are used to blade a new sheet graft. Note that the blade is held so that the tip of the cutting surface comes into contact with only the graft. B, Cotton-tipped applicators are rolled gently over the graft toward the slit to express fluid that has collected between the graft and the wound bed surface. When deblebbing thick grafts, adequate-sized slits are important to avoid recurring buildup of fluid, which may jeopardize graft survivability and result in scarring. C, Blebs tend to recur in the same place. Vigilance about deblebbing at least once every 8 hours until bleb formation ceases is advisable. Documentation of bleb formation and location ensures that the next caregiver is aware of graft sites in need of close monitoring. (From Carrougher GJ: Burn care and therapy, St Louis, 1998, Mosby.) • Caution should be used when evacuating fluid after vascularization of the graft begins to avoid disruption of the graft attachment endangering graft take. A more safe practice for removing fluid involves making a small nick in the sheet graft directly over the area of fluid accumulation and gently expressing the fluid through the hole. In either case, the fluid should be gently dabbed away with gauze dampened with sterile normal saline solution or sterile water.6 Seromas and hematomas tend to redevelop in the same areas, so careful charting should reflect location of any fluid pockets (blebs). Close monitoring of these areas should occur at least every 8 hours until bleb formation is no longer noted. • In the operating room, all nonviable tissue is surgically excised to create a wound bed able to support a skin graft (Fig. 121-3); therefore, the grafted area should be observed for bleeding for the first 24 hours. Figure 121-3 Meshed split-thickness skin graft covering the arm, with the remainder of the wound bed ready to be grafted. • The goals after a graft placement are to protect the wound bed from infection and desiccation and to ensure that no movement (shearing) of the graft occurs while it is becoming vascularized. Neovascularization begins within the first 24 hours of surgery as capillaries grow up into the graft, securing the graft permanently to its new site. Either a barrier dressing (e.g., Biobrane allograft [UDL Laboratories, Rockford, IL]) protects the wound (with or without a bulky dressing added), or a minimal nonadherent dressing (e.g., Xeroform [McKesson Brand, San Francisco]) is used with a bulky dressing over the grafted tissue to act as the barrier to infection, prevent drying and shearing. The newly grafted tissue must be well protected from shearing forces for 5 to 7 days to allow for graft adherence to the wound bed. With meshed skin grafts, the interstices of the autograft fill with granulation tissue and the epidermis of the autograft migrates over the granulation tissues. Successful grafting is often expressed as a percentage of graft “take,” or adherence and vascularization of the graft to the new site.1,5 • Cultured epidermal autografts, most frequently used with burn injuries, are commercially available and are an option when the patient does not have enough unburned tissue for donor sites to cover the burn in a reasonable period of time.1,7 Cultured epidermal autografts are grown from a sample of the patient’s own epidermal cells in a laboratory. However, the cost is prohibitive, the grafts are extremely fragile, and successful take of the graft is much more likely if the burn team has experience with this treatment.3 • The use of artificial skin and other options for wound coverage has expanded in recent years. Currently, the use of these wound coverings is limited to providing temporary wound coverage or allowing for dermal regeneration while waiting for suitable donor sites for definitive wound closure with autografting. • Allografts, also called homografts, are fresh or cyropreserved grafts from human donors. Allografts are the gold standard for temporary coverage of wounds. Allograft benefits include prevention of wound desiccation, promotion of granulation tissue, and decreased water and heat loss.1 • The use of Integra® Dermal Regeneration Template (Ethicon Endo-Surgery, Inc, Cincinnati, Ohio) has been shown to decrease length of stay (LOS) in severely injured burned adults.7
Skin Graft Care
PREREQUISITE NURSING KNOWLEDGE

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


121: Skin Graft Care

