| 5 | The Spine: Anatomy, Nociception, and the Distribution of Pain Signals |
Terminology
The most common forms of acute and chronic pain originating from the spine arise from degenerative changes in the intervertebral disk and the corresponding secondary after-effects found in the vertebral motor segment. The medical conditions resulting from intervertebral disk degeneration are referred to as spinal syndromes and are subdivided according to their location into cervical, thoracic, and lumbar syndromes. The terms local cervical, thoracic, or lumbar syndromes are used when the symptoms are limited to the affected spinal region. When nerve root compression or pseudoradicular symptoms cause pain to radiate into the limbs, the syndrome is labeled cervicobrachialgia or sciatica of the lumbar spine. In the thoracic spine, the previous familiar name of intercostal neuralgia has been replaced by the term thoracic root syndrome.
All of the biomechanical and pathological anatomical changes in the intervertebral segment related to intervertebral disk degeneration are known as degenerative disk diseases. These include a loss of central pressure and the development of fissures and signs of wear, resulting in a loosening of the intervertebral disk. Spondylosis and osteochondrosis are bony reactions in individual vertebral parts. They are not a diagnosis; rather, they are simply a radiographic symptom of a loosened intervertebral disk.
The displacement of intradiscal mass with the formation of sequestra can be observed in intervertebral disk degeneration. When decidingwhich therapeutic approach to use, it is essential to identify whether the posteriorly displaced intervertebral disk tissue is only a protrusion, where the anulus fibrosus is still intact, or whether the sequestrum has moved outward as a result of the perforation of the outer border of the disk, taking the form of a prolapse or herniation.
Nociception and the Distribution of Pain Signals in the Spine
The individual nociceptive complexes are closely packed together within the spine: mechanical insults coming from the intervertebral disk, nociceptors in the posterior longitudinal ligament and zygapophyseal joint capsule, nociceptively changed afferent fibers in the spinal nerve, and the distribution of noxious signals in the spinal cord. The medical conditions observed, the so-called spinal syndromes, are correspondingly complex. Types of pain and spread appear that can be linked to the irritation of the different parts of the nociceptive system. Neuralgias occur where pain is projected into and felt in the area of distribution of a segmental nerve; the cause of this disorder is not to be found in the area of pain. Brachialgia and sciatica are typical examples of this. Neuralgia is differentiated from organ pain by its position: in organ pain, the location of the pain and the disorder itself are identical, as in the local cervical and lumbar syndromes.
In addition there are forms of pain, especially in the cervical spine, where sympathetic nervous system impairment also plays a role. In this case, the pain is constant and diffusively spread, and is associated with vasomotor trophic symptoms. Pain that is linked to a 24 hour rhythm or a hormonal cycle, or that occurs frequently in autonomically labile individuals, is likely dependent on the sympathetic nervous system. Despite a multitude of symptoms that cannot be precisely defined, most types of pain coming from the spine can be linked to a certain neural structure within the vertebral motor segment.
Pain-Sensitive Structures in the Vertebral Motor Segment
Human intervertebral disks do not posses nerve fibers. Sensitive nerve endings have so far only been found on the outermost edge of the anulus fibrosus at the posterior longitudinal ligament (Kuhlendahl 1950, Kuhlendahl and Richter 1952, Mulligan 1957, Mendel et al. 1992). These histological examinations have been experimentally confirmed by Smith and Wright (1958). During surgery they fastened thin nylon threads to different vertebral motor segment structures and to the nerve root. After the operation was completed, typical symptoms could be induced by pulling on the posterior anulus fibrosus and on the nerve root.
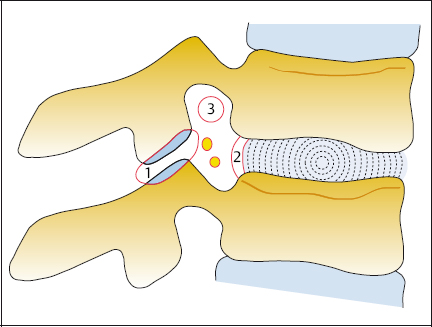
Kuslich and Ulstrom (1990) stimulated the different tissue structures in the vertebral motor segment during a lumbar intervertebral disk operation performed under local anesthetic, and registered the pain sensitivity. They found that pain could most easily be provoked on the skin and on the compromisednerve root, followedby the outer anulus fibrosus and the posterior longitudinal ligament. The ligamental attachments and the zygapophyseal joint capsules were less often sensitive to pain. The ligamenta flava, lumbar fascia, lamina, facet joint cartilage, and noncompromised nerve roots were completely insensitive to pain (Fig. 5.1).
Anterior intervertebral disk puncture, e.g., during a cervical discography, is pain free, just as lateral puncturing during a lumbar discography is pain free. Pain and feelings of pressure are not felt during the administration of a contrast agent when the intervertebral disk is intact. When the intervertebral disk is protruding and already in contact with the nerve root, an increase in volume can result in a spreading pain. This is used diagnostically in the distension test. During a medial transdural lumbar disk puncture, patients report only a short, lumbago-like pain sensation in the back when the posterior longitudinal ligament or the posterior anulus fibrosus is punctured. In lumbar disk operations under local anesthetic it is also possible to elicit typical back pain by using a probe to place pressure on the posterior edge of the intervertebral disk.
Spinal Nerve
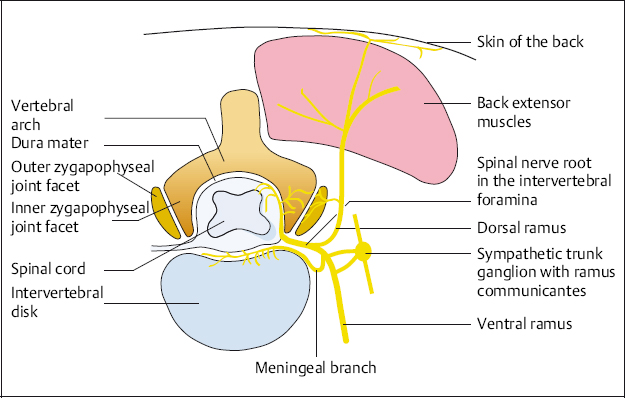
The spinal nerve consists of motor, sensory, and sympathetic components. After passing through the intervertebral foramen it divides into ventral and dorsal rami and a meningeal branch.
The ventral ramus is themostextensive. It supplies the anterior regions of the body and the limbs and is responsible for the dermatome-oriented nerve root syndrome.
The dorsal ramus supplies the skin and muscles of the back. In addition, it has extra branches running to the outer surface of the zygapophyseal joints and their capsules. The paired posterior branches can be seen alongside the vertebral column from the occiput to the coccyx. They pass through the fascia so as to reach the areas of skin that they supply. They are found relatively near the midline in the thorax (T1–T11). In the lumbar region (L1–L5) they are found lateral to the muscular bulge of the spinal extensors, and in the sacrum (S1–S4) paramedian over the posterior foramen.
The meningeal branch re-enters the spinal canal and then branches, supplying the inside section of the zygapophyseal joint capsule, vertebral periosteum, posterior longitudinal ligament, and the spinal cord meninges with efferent, afferent, and autonomic fibers (Fig. 5.2). The area surrounding the intervertebral foramen is a likely trouble spot for the development of pain in the vertebral motion segment.
This is especially the case in the lower sections of the cervical spine and lumbar spine. Here the vertebral foramina are enclosed by the zygapophyseal joints as well as the intervertebral segment; nociceptors and afferent fibers are found close to each other. The afferent fibers can develop into nociceptors when chronically irritated. A mechanical irritation of the sensitive fibers of the meningeal branch can occur in the zygapophyseal joint capsule, in the posterior longitudinal ligament, and in the spinal nerve root itself. Pain is induced by the displacement of intervertebral disk tissue with pressure on the posterior longitudinal ligament or on the spinal nerve root. These types of pain are described as primarily discogenic, or as symptoms originating from the intervertebral disk. In contrast, secondary discogenic pain originates from the zygapophyseal joints or from the back muscles.
NOTE
In the mechanical irritation of nociceptors and afferent fibers, the amount of deformation is not important. What matters is how quickly the deformation happens.
Even torsion scolioses, where the spine deviates considerably from the body’s axis, are symptom free when they have developed over many years. Nerve roots, ligaments, and zygapophyseal joint capsules are obviously able to adapt. On the other hand, a small posteriorly protruding intervertebral disk can cause the most severe symptoms when it appears suddenly and makes even minimal contact with the pressure-sensitive nociceptors in the posterior longitudinal ligament or in the nerve root.