Contraindications
As with all local injections, inflammatory bacterial changes around the injection site (e. g., infected sebaceous glands) and open wounds are contraindications for spinal injection therapy. Systemic infections that are either acute or have only recently subsided (e. g., urinary tract infections, tonsillitis, common colds) should also be absent. When such infections are clinically suspected, further diagnostics should exclude these infections before starting on the planned injection therapy.
Because of the possible danger of infections occurring or flaring up again, it is important to ensure completed secondary healing following surgey on the intervertebral disk, epidural abscesses, and spondylitis.
Known hypersensitivity to local anesthetics is another contraindication for minimally invasive spinal therapy. Any suspicion that substances will provoke an allergic reaction should be checked in advance.
The general contraindications to the use of steroids should also be kept in mind. The side effects of glucocorticoids are related the main actions of the drug (see Chapter 4, “Multimodal Medication Concomitant Therapy”) and the administration of a single dose does not usually cause dangerous adverse effects. When the medical history shows that patients who require long-term treatment have conditions such as osteoporosis, diabetes, glaucoma, or ulcers, IRAP treatment, for example, can be used as an alternative to steroids (see Chapter 4, “Interleukin-1 Receptor Antagonist Protein”).
Orthopedic injection therapy is also contraindicated for patients with neurological seizure disorders, spinal cord diseases, or severe cardiovascular disorders because it may require intrathecal administration, with sudden drops in blood pressure. Any injections near the spine are contraindicated for patients with internal diseases such as severe conduction defects, decompensated heart failure, or blood coagulation disorders.
Patients who are taking anticoagulants such as Warfarin (Coumarin) should be put on low-dose heparin before minimally invasive spinal therapy is undertaken. The intake of thrombocyte aggregation inhibitors such as aspirin or ticlopidine (Tyklid), is also a contraindication. Patients should be taken off this medication at least a week before having any injections near the spine, in consultation with the general practitioner.
| Local and/or systemic infections |
| Open wounds |
| Known hypersensitivity to local anesthetics |
| Steroid contraindications |
| Neurological seizure disorders |
| Spinal cord diseases |
| Severe cardiovascular disorders |
| Severe conduction defects |
| Decompensated heart failure |
| Blood coagulation disorders |
| Concurrent blood-thinning medication (aspirin, coumarin, etc.) |
| Absence of the prerequisites for injection therapy (emergency equipment, monitoring facilities, dedicated injection room, etc.) |
The environment plays an important a role in keeping the patient calm (Grifka et al. 1999). The treatment room should be a sterile environment, suitably equipped for all of the injection therapy procedures (Geiss 2002, Mutter et al. 2002).
After therapy patients should be specially monitored, so that any disorders of vital functional can be recognized in time and prevented. Equipment for venous access, oxygen supply, intravenous drips, and resuscitation must be available in case injection-related complications arise (Table 6.1).
Patient Information
The physician’s duty to provide information to the patient is founded on the professional code of conduct. From a legal point of view, every type of medical intervention used for diagnoses or treatment potentially represents illegal bodily harm. The patient’s consent is required to justify the intervention. Patients have the right to be informed in an understandable and complete manner, during a personal discussion with their treating physician, about the clinical picture of their symptoms and the interventions proposed for diagnosis and treatment. Information can be divided into three categories, relating to diagnosis, disease progression, and risks. Information about the diagnosis is preparation for explaining the treatment itself. The explanation of disease progression should inform the patient about the likely further development of symptoms if the intended intervention is carried out, and if it is not. Alternative treatment possibilities should be described at this stage. An explanation of the risks involved, i. e., the probability that the intervention will be unsuccessful and the possible consequences of the planned treatment, is central to in the physician’s duty in providing information.
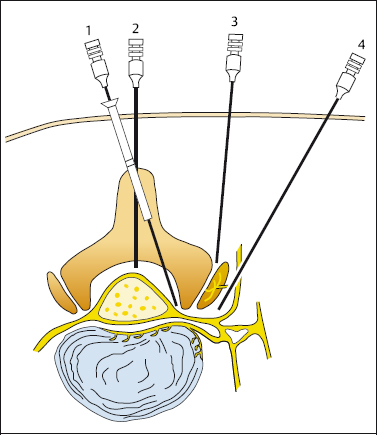
Informative discussions, recorded in writing, are established clinical practice. Drawing a simple sketch to describe the planned intervention can dramatically improve patients’ understanding of the intended therapy. The sketch can be added to the consent form.