Anatomy
Knowledge of the anatomy of the cerebral cortex, with sensory and motor loci, is important for assessing focal sensory and motor deficits. However, many etiologies of depressed mental status in surgical critical illness (e.g., diffuse axonal injury, brain hypoperfusion, narcosis) produce global alterations in cortical function that may or may not be associated with localized findings. Important for assessing altered mental status is an understanding of the anatomy of the reticular activating system (RAS), a diffuse group of neurons that extend along the central brainstem from the medulla to the thalamus (
Fig. 9.1). RAS is stimulated by every major somatic and special sensory pathway and serves to activate the cerebral cortex. Since the RAS arises in the brainstem, knowledge of the anatomy of the brainstem is useful for evaluating the status of the RAS.
The brain is enclosed in a hard, rough chamber, which, while being protective, can be responsible for direct or “counter coup” injury (
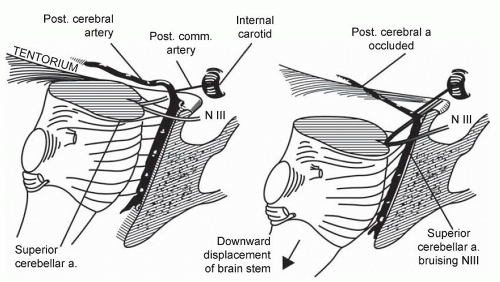
Fig. 9.2). The medial temporal lobe is positioned close to the midbrain, the path of the third cranial nerve and cerebral blood vessels (
Fig. 9.3). Particularly, medial displacement of the temporal lobe is likely to interrupt first the function of the third cranial nerve, then the midbrain, and, subsequently, larger areas of the brainstem (
Fig. 9.4).
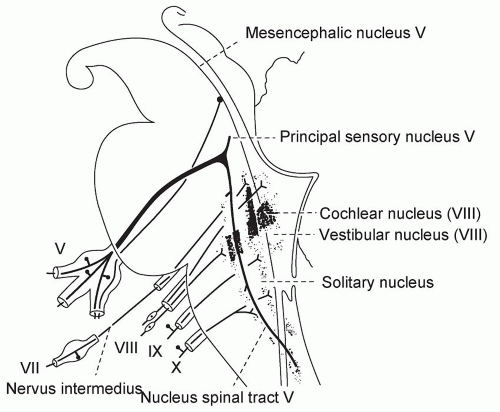
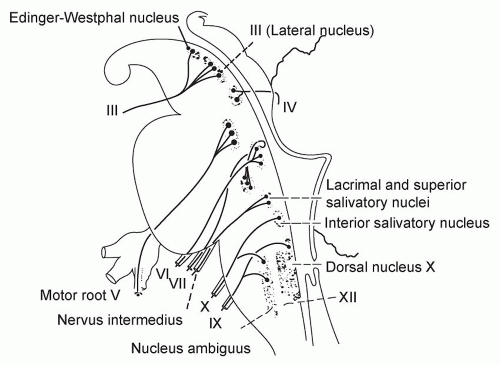
The brainstem is divided into midbrain, pons, and medulla (
Figs. 9.5 and
9.6). Brainstem nerves that are valuable to evaluate include the following: (
1) the third for innervation of the medial rectus and parasympathetic innervation to the pupil; (
2) the fifth for sensation to the cornea; (
3) the seventh for motor to the eyelids; (
4) the sixth for innervation of the lateral rectus; (
5) the eighth for innervation of the vestibular apparatus; (
6) the medial longitudinal fasciculus connecting the eighth to sixth and third; (
7) the course of the sympathetic nervous system through the entire brainstem.
Consciousness requires cortical function and is not lost unless cortical function is diffusely diminished. Diffusely diminished cortical function may result either from direct, global disruption of cortical function or from disruption of the RAS in the brainstem. Since the cortex is more sensitive to metabolic disturbances than the brainstem (i.e., hypoglycemia, hypoxia), “cortical coma” is more likely to be “metabolic,” whereas “brainstem coma” most often is secondary to pressure on or structural damage to the brainstem (
1).
Physiology of Cerebral Blood Flow, Oxygen Metabolism, and Intracranial Pressure
The brain requires a continuous supply of oxygen and glucose to support the aerobic glycolysis necessary to maintain the integrity of brain neurons. The brain is proportionally more sensitive to decreased delivery of oxygen than decreased delivery of glucose. The cerebral metabolic rate of oxygen (CMRO2) is a useful measure of brain metabolism and is calculated as follows:
Where, CBF = cerebral blood flow; C = oxygen content; a, v = arterial, venous, respectively.
In adults who are awake, CBF approximates 50 ml/100 g tissue at PaCO
2 of 40 mm Hg. CMRO
2 is about 3.2 ml/100 g under these conditions. CMRO
2 may increase with activities such as seizures and decrease with drug-induced coma. Usually, CBF adjusts to meet alterations in
CMRO
2. However, severe brain injury may lead to disruption of the autoregulation of CBF such that too much or too little CBF may be supplied for the metabolic demands of the brain.
CBF is primarily determined by cerebral perfusion pressure (CPP), which is the difference between mean arterial pressure (MAP) and intracranial pressure (ICP), as well as the arteriolar vascular resistance in the brain tissue. Therefore, CBF will increase if CPP increases and/or arteriolar resistance decreases, and it will decrease if CPP decreases and/or arteriolar resistance increases.
When CBF falls sufficiently such that more oxygen cannot be extracted (<23 ml/100 g), then CMRO2 will decrease. First, the synaptic function ceases and then cell death ensues unless the normal metabolic demand of brain cells is reduced.
The equation for CMRO2 shown above can be rearranged to the following:
This demonstrates that alterations in the arteriovenous content are secondary to alterations in CMRO
2 or CBF or both. Alterations in a-v saturation rather than the content have been argued to more accurately reflect brain oxygen status, especially when venous oxygen saturation is
low, indicating increased oxygen extraction. Continuous measurement of jugular oxygen saturation (SjvO
2) has been used as a monitor of global cereberal oxygen delivery and consumption, especially in patients with TBI. Normal jugular venous oxygen saturation is 55-71%. Values <50% are usually secondary to decreased delivery rather than increased consumption (
2,
3,
4).
Direct measurement of brain tissue pO
2 (PbtO
2) is also under investigation as a cerebral metabolism monitor. Normal brain pO
2 is in the range of 37 mm Hg, with severe hypoxia identified by values of 8 mm Hg or less. PbtO
2 may be influenced by regional as well as global reductions in CBF (
4).
ICP (normally <15 mm Hg) is determined by the following variables: cerebrospinal fluid (CSF) volume, cerebral blood volume (CBV), and brain cell volume (
Table 9.2). The measurement of ICP and use of CPP as well as oxygen-related monitors to manage severe head trauma are discussed in the section on “Head Trauma”.