Shock
Those who cannot remember the past are condemned to repeat it.
—George Santayana (1863-1952)
HISTORIC CONCEPTS OF SHOCK
From the latter half of the nineteenth century through the twentieth century, the concepts and definitions of shock have been varied and often considered mutually exclusive (Table 2.1). During the first half of the twentieth century, the advocates of hypovolemic hypoperfusion as the principle etiology of shock (e.g., Blalock and Wiggers) vigorously opposed the advocates of circulating toxins as the mechanism (e.g., Cannon) (1, 2, 3, 4). As the twenty-first century has proceeded, this same advocacy continues, but the necessity of exclusivity has dissipated.
The concept of shock that will be emphasized in The Clinical Handbook for Surgical Critical Care also has a historic underpinning. In 1872, Samuel D. Gross offered the analysis that during shock “… the machinery of life has been rudely unhinged …”—a formulation that allows for a coalescence of etiologies rather than strict separation (5).
Today, shock can be considered a manifestation of total body cell metabolic disturbance— an unhinging of life machinery most vigorously manifested by decreased total body oxygen consumption. The principle etiologies of this alteration are still connected to the twentieth-century debate. Too little oxygen delivery and too much inflammatory toxin both are capable of producing shock. In fact, these two processes are not mutually exclusive, but are characteristically additive threats to cell function. Simply stated, hypoperfusion begets inflammation, and inflammation begets hypoperfusion (Table 2.2).
Shock from severe hypoperfusion and severe systemic inflammation is the cause of death and/or multisystem organ failure in surgical critical illness. Understanding these mechanisms of cell metabolic threat can augment all features of surgical critical care evaluation and management (Where is the hole? How do I plug the hole? Why is the hole there?). Therefore, repeating the history of shock concepts from Gross through Cannon, Blalock and Wiggers to more modern contributors like Gann and Rivers can prove more a reward than a condemnation (6, 7).
SHOCK AND DECREASED OXYGEN UTILIZATION
Decreased Oxygen Delivery
Oxidative phosphorylation is the primary metabolic process whereby mammalian cells produce cellular energy and heat. Ninety percent of oxygen utilization occurs in the mitochondria and ATP production accounts for 80% of oxygen consumption (8). While deficits in arterial oxygen saturation and blood hemoglobin concentrations can limit oxygen delivery to cells, most often a reduction in blood flow (hypoperfusion) is responsible for diminished oxidative phosphorylation. When total body oxygen delivery is sufficiently compromised, total body oxygen consumption must decrease, a condition termed “delivery-dependent oxygen consumption” Figure 2.1, (9). The inflection point where the increasing consumption curve levels off has been termed as the “critical” oxygen delivery state of that preparation. Oxygen consumption that is delivery dependent and below critical is associated with evidence of cellular energy deficits (e.g., lactic acidosis and hypothermia) (10, 11).
In 1942, Cuthbertson described metabolic alterations following tissue injury and linked the combination of hypothermia and decreased oxygen consumption to a reduction in cell vitality, which he termed as the “Ebb Period” or “Ebb Phase.” Most of The Ebb Period was secondary to “tissue asphyxia” and associated with a high mortality rate (12, 13).
When minute by minute oxygen delivery is insufficient to meet oxidative phosphorylation demands, this is termed an oxygen deficit. When the deficit continues over many minutes, then the product of deficit and minutes is termed as the oxygen debt. Global hypovolemic hypoperfusion (decreased cardiac output from decreased intravascular volume) is the most
common cause of oxygen debt and the Ebb Period of shock. The magnitude of this debt has been directly correlated with mortality and organ failure risk (14, 15, 16).
common cause of oxygen debt and the Ebb Period of shock. The magnitude of this debt has been directly correlated with mortality and organ failure risk (14, 15, 16).
Table 2.1 Common Concepts of Shock – Early 20th Century | |
|---|---|
|
|
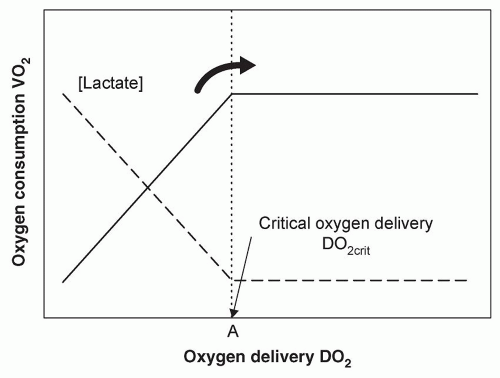 Figure 2.1 A schematic representation of oxygen consumption and oxygen delivery depicting the point when consumption becomes delivery-dependent DO2crit. Source: From Ref. 10. |
Cytopathic Hypoxia
After the cell injury associated with the Ebb Period and oxygen debt, normalization or augmentation of the circulation typically results in an increase in oxygen consumption and heat production that Cutherbertson termed as the “Flow Period” (also called the “Flow Phase”); this is a circumstance associated with improved survival as documented over the last several decades (12, 17). While oxygen consumption greater than basal does not preclude mortality, the inability to increase oxygen consumption following improved oxygen delivery is highly lethal and akin to failure to emerge from the Ebb Period (17, 18, 19, 20). This alteration in cell metabolism has been termed “cytopathic hypoxia,” whereby mitochondrial oxidative phosphorylation is
impaired by mechanisms such as inhibition of pyruvate dehydrogenase, nitric oxide inhibition of cytochrome A and A3, as well as alterations in the enzyme poly(ADP-ribose) polymerase (21). The most common clinical association with this deficit in cell oxygen utilization is severe systemic inflammation (18, 21).
impaired by mechanisms such as inhibition of pyruvate dehydrogenase, nitric oxide inhibition of cytochrome A and A3, as well as alterations in the enzyme poly(ADP-ribose) polymerase (21). The most common clinical association with this deficit in cell oxygen utilization is severe systemic inflammation (18, 21).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






