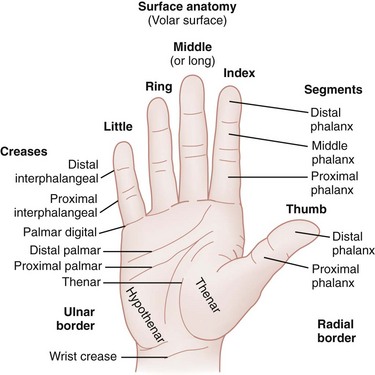
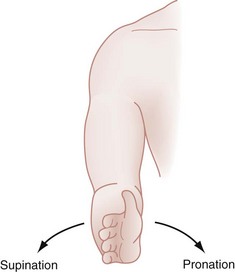
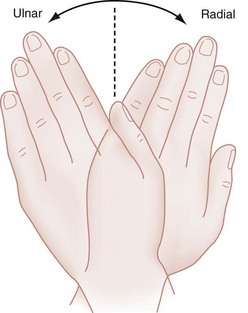
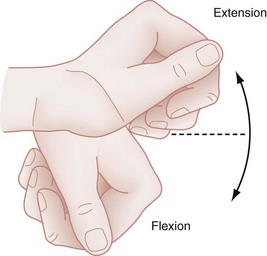
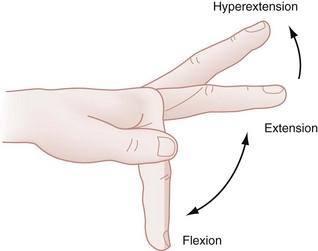
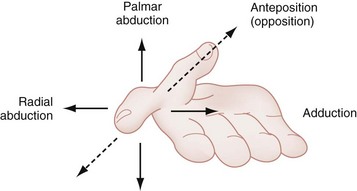
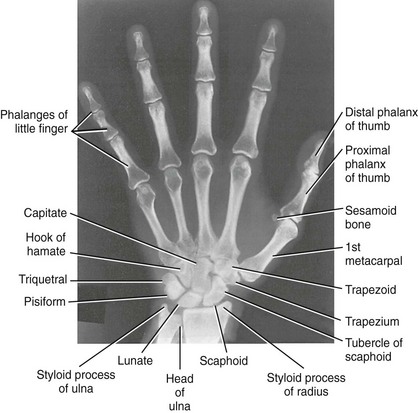
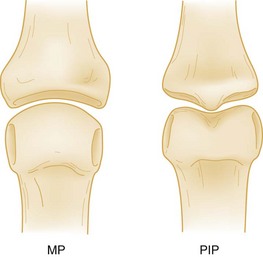
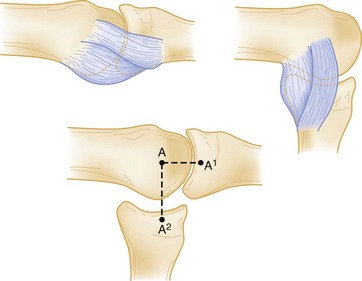
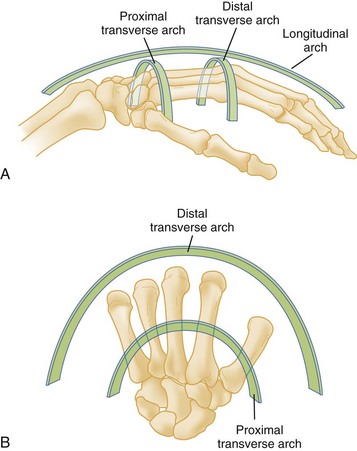
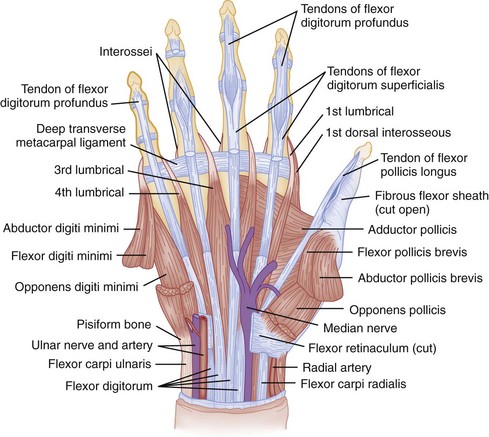
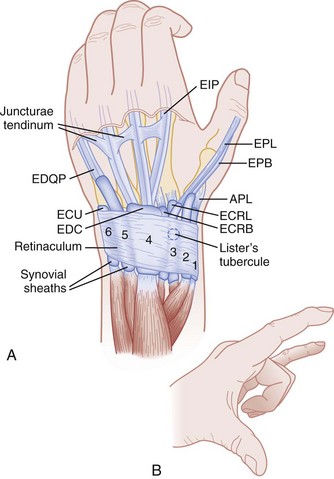
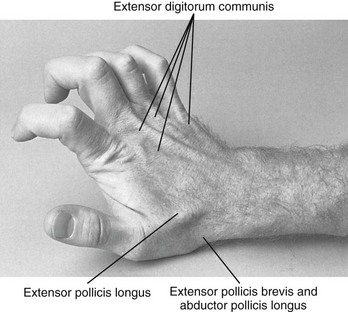
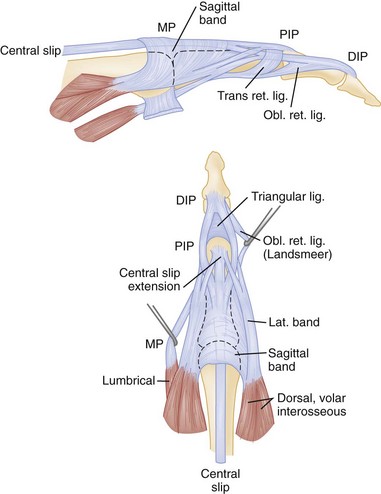
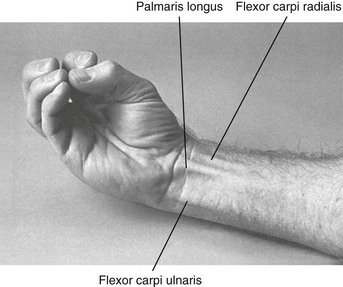
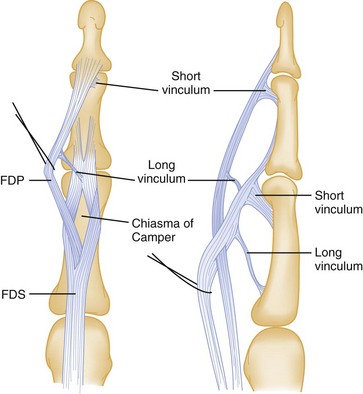
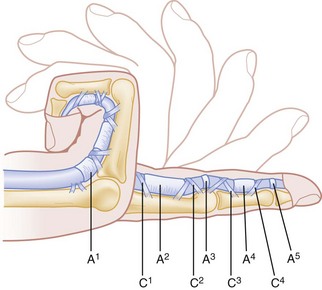
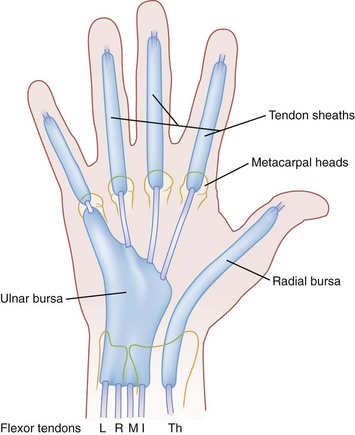
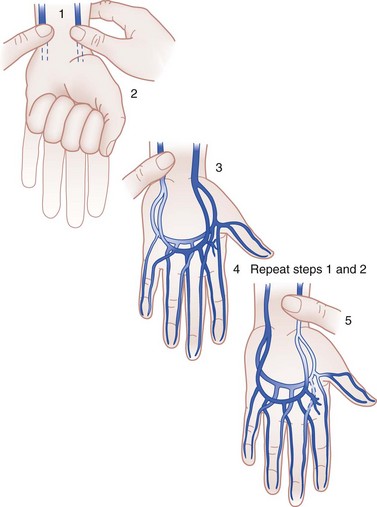
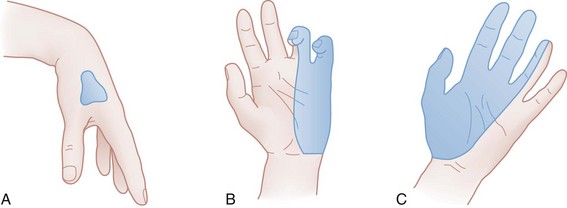
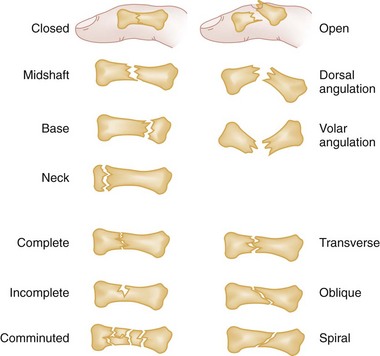
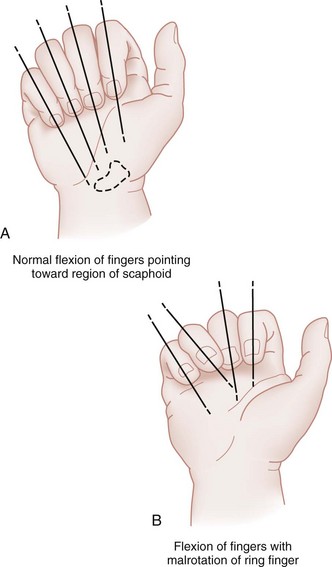
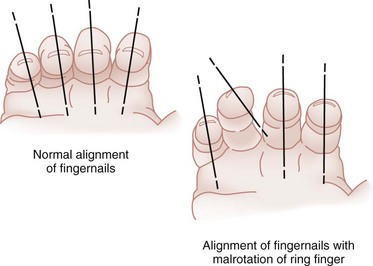
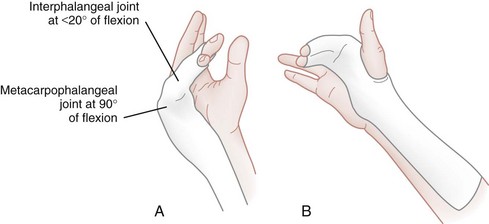
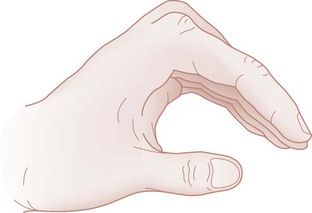
Chapter 50 Overall, hand injuries are reported to represent 5 to 10% of visits to an emergency department (ED), and approximately 6% of the patients have deep, significant injuries.1 Injuries have environmental, occupational, and recreational causes and are seen in all age groups. The spectrum of injury includes infections, lacerations, fractures, crush wounds, amputations, and burns. It is estimated that 10% of all patients with hand injuries require referral to a hand specialist, and most patients referred from EDs have fractures.2 The disability potential of hand injuries generally is high; such disability may involve loss of strength, flexibility, or sensation. According to available data, hand injuries account for 19% of lost-time injuries and for 9% of worker compensation cases.3 Approximately 3 to 4 million working days are lost each year as a result of hand injuries.4 Overall, hand and fingers are the most frequent body parts injured in the workplace and cared for in EDs.5 To avoid confusion, it is important that standard terminology for the surface anatomy of the hand be used (Fig. 50-1). The back of the hand and fingers is called the dorsal surface, and the palm side is called either the palmar or the volar surface. The borders of the hand are radial and ulnar. The five digits often are designated by numerals, but common names are preferable: I (thumb), II (index finger), III (long or middle finger), IV (ring finger), and V (little finger). Each finger has three joints: the metacarpophalangeal (MCP), the proximal interphalangeal (PIP), and the distal interphalangeal (DIP) joints. The thumb has an MCP joint and only one interphalangeal (IP) joint. There are proximal, middle, and distal phalanges in the fingers and only a proximal and a distal phalanx in the thumb. The thenar mass or eminence refers to the muscular area on the palmar surface overlying the thumb metacarpal. The hypothenar eminence is the muscle mass on the palmar surface overlying the little finger metacarpal. Hand and digit motion has been standardized and is illustrated in Figures 50-2 through 50-6. The carpometacarpal (CMC) joint is more mobile in the thumb than in the other fingers and is the key to the grasp and dexterity that characterize the human hand. Motions of this joint include palmar abduction (also called flexion), radial abduction, retroposition (extension), adduction, and opposition (see Fig. 50-6). The IP joints are essentially hinge joints and are capable of only two motions: flexion and extension. The hand has two skin surfaces, each with different functions. The skin of the palm is thick compared with the dorsal skin and is stabilized by fibrous connections on its deep surface. The skin creases in the palmar aspect of the hand are largely transverse and represent adherence between skin and underlying fascia, without intervening adipose tissue. These features facilitate flexion and limit the development of inflammatory edema in the palm.6 The other noteworthy characteristic of the palmar skin is the unique arrangement of epithelial ridges of the dermis that form cutaneous striations. These ridges have forensic importance in the pulp as “fingerprints” and play an important role in increasing friction for grasping objects.7 The dorsal skin is relatively thin and mobile, permitting motion of the various joints. As a path of least resistance, the dorsum of the hand also swells easily after inflammation or trauma, which may limit flexion of the MCP joints.7 In addition, infection in the palmar aspect of the hand may cause dorsal swelling; this finding can be misleading without a careful physical examination. The hand and wrist contain 27 bones: 14 phalangeal bones, 5 metacarpal bones, and 8 carpal bones (Fig. 50-7). The eight small carpal bones in the region of the wrist are strongly united to one another by ligaments. These bones form synovial joints and are arranged in two rows, proximal and distal, with four bones in each row. Together the bones of the carpus present a concavity on their volar surface, which is bridged by a strong membranous band, the flexor retinaculum. In this way, the bridge and the bones form a tunnel, known as the carpal tunnel, through which pass the median nerve and the long flexor tendons of the fingers. The IP joints are inherently more stable than the MCP joint by virtue of their bicondylar configuration, which gives a modified tongue-in-groove appearance (Fig. 50-8). The soft tissue supporting these joints includes the capsular ligamentous structures, which afford stability, and the tendinous structures, which generate mobility. The metacarpal and IP joints are stabilized on both sides by collateral ligaments and anteriorly by a palmar fibrocartilaginous “volar plate.” Because of anatomic differences between the metacarpals and phalanges, the IP collaterals are tight throughout the entire range of motion, whereas the collaterals of the MCP joint are tightest in flexion (Fig. 50-9). The IP joints are hinges, but the MCP joint has additional side-to-side mobility and rotational movement to facilitate efficient grasp.7 The clinical importance of these differences is that for minimization of the development of contractures after joint injuries, the preferred position of immobilization of the PIP joints is extension, whereas the MCP joints are more properly placed in flexion. The structure and arrangement of the metacarpals are noteworthy. The metacarpals participate in three arches: the proximal (carpal) and distal (metacarpal) transverse arches and the longitudinal arch6 (Fig. 50-10). The index and long finger metacarpals form a fairly immobile segment because of their ridged articulation with the carpals. The adjacent metacarpals are more mobile. This unique anatomy gives the human palm a longitudinal and transverse concavity when the thumb is alongside the index finger; however, this changes to an oblique gutter when the thumb is extended. The small bones of the child’s hand differ significantly from the bones of the adult and from other long bones because of the presence of an epiphysis or growth plate at one end of the bone. The phalangeal epiphyses and the thumb metacarpal epiphysis are located at the proximal end, and the finger metacarpal epiphyses are located at the distal end of the bone (Fig. 50-11). In boys the proximal phalangeal epiphysis appears at 15 to 24 months and fuses at 16 years. In girls it appears at 10 to 15 months and fuses at 14 years.8 The time of appearance and fusion is related to skeletal maturity and can be judged accurately until puberty from hand and wrist radiographs, because the sequence of development is age-specific.9 Intrinsic Musculature.: The intrinsic muscles of the hand include the muscles of the thenar and hypothenar eminences, the adductor pollicis, the interossei, and the lumbricals (Fig. 50-12). The thenar muscles cover the thumb metacarpal. This group includes the abductor pollicis brevis, opponens pollicis, and flexor pollicis brevis. These muscles originate in the flexor retinaculum and on the carpal bones and insert at the base of the first metacarpal and first proximal phalanx. They act in concert with the long flexors and extensors to carry the thumb through its intricate range of motion. The muscles are evaluated by palpation of the thenar eminence for contraction as the patient brings together the tips of the thumb and little finger. They also can be tested by asking the patient to place the dorsum of the hand on a flat surface and to raise the thumb up straight to form a 90-degree angle with the palm. The thenar muscles usually are innervated by the motor branch of the median nerve. In some cases they may be partially innervated by the ulnar nerve. The adductor pollicis arises from the index and middle finger metacarpals and inserts on the first proximal phalanx. This muscle is innervated by the ulnar nerve. Thumb adduction is tested separately by having the patient forcibly hold a piece of paper between the thumb and radial side of the index proximal phalanx. If the adductor pollicis is weak or nonfunctioning, the thumb IP joint flexes with this maneuver (Froment’s paper sign).10 In this evaluation, the two hands should be compared. Extensor Tendons.: The extensor tendons are on the dorsal side of the forearm, wrist, and hand. The nine extensor tendons cross the wrist joint dorsal to its axis of rotation, pass under the extensor retinaculum, and are separated on the dorsum of the hand by a series of six fibro-osseous canals or compartments. Figure 50-13 outlines the compartments and their contents. The fibrous roof of these compartments prevents the tendons from bowstringing dorsally during active finger extension, particularly when the wrist also is extended. In the third compartment, a single tendon, the extensor pollicis longus, arises from the deep muscles of the midforearm, passes around a bony prominence on the dorsum of the wrist termed Lister‘s tubercle, and inserts on the base of the distal phalanx of the thumb. This tubercle can be palpated just proximal to the wrist joint. The extensor pollicis longus forms the dorsal border of the anatomic snuffbox, and the abductor pollicis longus forms the volar border (Fig. 50-14). The floor of this area contains the radial artery and two carpal bones, the scaphoid and trapezium. The extensor pollicis longus functions to extend and adduct the entire first ray and extend and hyperextend the IP joint of the thumb. This muscle is evaluated by placing the hand flat on a table and having the patient lift only the thumb off the surface. Because the abductor pollicis brevis and the adductor pollicis add terminal extension, complete laceration of the extensor pollicis longus tendon may not eliminate the patient’s ability to extend the thumb.11 The tendons that extend the fingers—the extensor indicis proprius and the extensor digitorum communis—are in the fourth compartment. The extensor digitorum muscle divides into four tendons proximal to the wrist. In the dorsum of the hand, these tendons are joined distally by fibrous interconnections called juncturae tendinum which help stabilize them to their insertions in the extensor expansions of the index, middle, ring, and little fingers. The extensor digiti minimi is contained in the fifth dorsal compartment. Both the extensor indicis proprius and the extensor digiti minimi typically lie ulnar to their respective common extensor tendons. The dual extensor system for the index and small fingers gives these two digits extension independent of the other digits. The middle finger and especially the ring finger have considerably limited independent extension. The motion restriction is because of the juncturae, which also prevents retraction of the proximal tendon end after distal transection of an extensor. Complete severance of an extensor proximal to the juncturae can be associated with normal MCP joint extension.7 This extension occurs through the juncturae connections. The extensor digitorum communis tendons can be evaluated by asking the patient to straighten out all of the fingers. The function of the extensor indicis proprius can be isolated from the common extensors by asking the patient to make a fist and then to point the index finger. The extensor digiti minimi is examined by having the patient straighten the little finger while the hand is closed into a fist. The extensor mechanism of each digit is a complex interrelationship of muscle-tendon units of the long extrinsic extensor tendons and the intrinsic system (Fig. 50-15). The extensor expansion divides into a central slip that attaches to the middle phalanx and two lateral bands that join with the tendons of the lumbrical and interosseous muscles and attach to the base of each distal phalanx. The interossei and lumbrical muscles insert in the lateral aspects of the dorsal hood. Most of the power of the common extensors serves to extend the MCP joint. Distal digit extension is provided by continuation of the lateral band mechanism and the oblique retinacular ligament. Because of this complex anatomy, injuries involving the extensor mechanism require meticulous repair. Flexor Tendons.: The flexor tendons reside on the volar side of the forearm and cross the wrist joint volar to its axis. In general, 12 tendons function to flex the wrist and digits; three of them—the flexor carpi radialis, flexor carpi ulnaris, and palmaris longus—primarily flex the wrist and deviate the wrist radially or ulnarly (Fig. 50-16). The remaining tendons pass into the digits through the carpal tunnel. A single tendon, the flexor pollicis longus, inserts on the distal phalanx of the thumb, and two flexor tendons go to each remaining finger. The flexor digitorum superficialis (FDS) tendons bifurcate near the base of the proximal phalanges and surround the tendons of the FDP before inserting on the middle phalanges of the index, middle, ring, and little fingers (Fig. 50-17). The FDS flexes all the joints it crosses, including the wrist, PIP joints, and MCP joints. The profundus tendons lie deep to the superficialis tendons over most of their course in the forearm. At the level of the MCP joint, they perforate the superficialis tendon to emerge to a superficial position. They insert at the base of the distal phalanx and act primarily to flex the DIP joint and all joints flexed by the FDS. From the level of the MCP joint distally, the two flexor tendons become enclosed in a fibrous flexor sheath lined by synovium. Regions of thickening in this sheath form pulleys that help prevent bowstringing of the flexor tendons across the joint and assist smooth, effective flexion (Fig. 50-18). After observation, each muscle-tendon unit is tested with a functional examination. The flexor carpi radialis, palmaris longus, and flexor carpi ulnaris are tested together by having the patient flex the wrist against resistance while the examiner palpates the individual tendons. The tendon of the flexor pollicis longus attaches to the base of the distal phalanx of the thumb and flexes the thumb MCP and IP joints. This tendon is tested by having the patient bend the tip of the thumb against resistance. FDP function can be tested by having the patient flex the distal phalanx of each finger while the PIP is stabilized in extension by the examiner (Fig. 50-19). The FDS is tested individually by asking the patient to flex the PIP joint while the other fingers are held in extension to block the flexion produced by the profundus tendons (Fig. 50-20). This is a subtle but important distinction, because lacerations of the digital creases can easily damage one or more of the tendons or adjacent neurovascular bundles. The FDP is more commonly lacerated in the finger because of its paradoxically superficial position. Synovial Spaces.: Bursae are synovial sheaths that cover tendons as they pass through osseofibrous tunnels. They contain synovial fluid and serve two essential functions: They decrease friction during tendon movement, and they help supply nutrients to the relatively avascular tendons (Fig. 50-21). These sheaths also can provide pathways for spread of infection. Extensor tendons do not lie within definite sheaths and are afforded a greater resistance to infections. The synovial sheaths of the flexors in the index, middle, and ring fingers are enclosed from their insertion to approximately the level of the distal palmar crease. The sheath of the flexor pollicis longus extends from the tip of the thumb to the proximal volar wrist crease, where it communicates with the radial bursa in the palm and carpal tunnel. Similarly, the synovial sheath of the little finger communicates with the ulnar bursa. Clinical features of flexor tenosynovitis are caused by inflammation and distention of these synovial sheaths. Kanavel12 described the classic signs: a semiflexed posture of the digit, pain on passive extension of the digit, fusiform swelling, and tenderness of the synovial sheath. Arterial System.: The hands and the digits have a dual blood supply (Fig. 50-22). The major blood supply to the hand is from the radial and ulnar arteries. The radial artery lies on the anterior aspect of the radius in the distal part of the forearm. It continues around the lateral side of the wrist onto the dorsum of the hand by passing deep to the tendons of the abductor pollicis longus and the extensor pollicis brevis. On entering the palm, the radial artery terminates as the deep palmar arch. The ulnar artery enters the hand anterior to the flexor retinaculum on the radial side of the ulnar nerve and pisiform bone. The artery gives off a deep branch and then continues into the palm as the superficial palmar arch. This complex arterial arch system anastomoses and sends branches to the individual digits and the deep palmar spaces. Because of extensive collateralization, the hand usually survives even if both vessels are transected at the wrist.13 The circulation of the hand is evaluated by palpation of the radial and ulnar arteries on the volar aspect of the wrist, by assessment of the color and warmth of the skin, and by testing of capillary refill. Because “normal” findings vary among patients, the injured hand should be compared with the unaffected side. Although Allen’s test is an imperfect predictor of vascular compromise, it is commonly used to determine the patency of the arteries supplying the hand and the contributions to the circulation of the hand derived from each of the major vessels. The radial and ulnar arteries are compressed by the examiner at the wrist (Fig. 50-23). The patient opens and closes the hand repeatedly to exsanguinate it and then maintains a relaxed position. The radial artery is released. If the palm and fingers fill immediately with blood, the radial artery is patent, with good collateral flow into the ulnar artery system. To evaluate the ulnar artery, the same steps are repeated, but the ulnar artery is released. This method also can be used on a single digit to help evaluate the patency of each digital artery to that finger. Unilateral digital artery injuries may be well tolerated owing to adequate collateral circulation from the uninjured side. Bilateral digital artery injuries, although rare, tend to have poor outcomes.13,13a,13b Venous and Lymphatic Systems.: The veins generally follow the arterial pattern in the deep system. The abundant dorsal, superficial veins are more extensive than the deep system and drain most of the blood from this region. The lymphatic vessels essentially follow the veins, with most lymph flowing into channels in the dorsal subcutaneous space. This vascular anatomy and the laxity of the dorsal skin account for palmar infections causing swelling on the dorsum rather than on the palmar surface of the hand. Motor Innervation.: The radial nerve (formed from nerve roots C6 through C8) passes through the supinator muscle and enters the dorsal aspect of the wrist between the radial styloid and Lister’s tubercle. At this level, the nerve has a purely sensory function. Its important motor function is to innervate the dorsal extrinsic muscles in the forearm, which extend the wrist and MCP joints and abduct and extend the thumb. No intrinsic muscles in the hand are innervated by the radial nerve. Motor function in this nerve is tested by having the patient extend the wrist against resistance. Proximal injury to the radial nerve causes a condition known as wristdrop: The fingers are held in flexion at the MCP joints, and the thumb is adducted (Fig. 50-24A). The ulnar nerve (C7, C8, and T1) passes through the flexor carpi ulnaris muscle in the forearm and lies ulnar to the artery and superficial to the flexor retinaculum. It enters the hand at the wrist through the ulnar tunnel, or Guyon’s canal. The ulnar nerve innervates the hypothenar muscles, the seven interosseous muscles, the lumbrical muscles to the ring and little fingers, and the adductor pollicis. Innervation of the flexor pollicis brevis is variable. In the forearm, the flexor carpi ulnaris and the ulnar half of the FDP also are innervated by the ulnar nerve. Loss of motor function of the ulnar nerve results in inability to pinch a piece of paper tightly between the thumb and the index finger. A late characteristic of distal ulnar damage is Duchenne’s sign, manifested by clawing of the ring and little fingers (see Fig. 50-24B). The ring and little fingers are hyperextended at the MCP joints by the extensor digitorum communis (radial nerve) and flexed at the IP joints by the FDP (intact proximal ulnar nerve). In addition, the interosseous and hypothenar muscles are atrophied. The median nerve enters the forearm through the pronator teres muscle. At that level, it innervates that muscle, the flexor carpi radialis, the FDS, the radial part of the FDP, the flexor pollicis longus, and the pronator quadratus. The branch of the median nerve that innervates the last three muscles is called the anterior interosseous nerve. The median nerve enters the hand through the carpal tunnel accompanied by the nine extrinsic flexor tendons of the digits. The thenar motor branch (recurrent median nerve) innervates the abductor pollicis brevis, the opponens pollicis variably, and the flexor pollicis brevis. Common digital branches innervate the lumbrical muscles to the index and long fingers. Injury to this nerve occurs most commonly at the level of the wrist, by laceration or by compression in the carpal tunnel. Motor function is tested by having the patient appose the thumb to the index digit. Injury to the median nerve in the upper forearm or at the elbow usually results in weakness or absence of flexion of the index finger distal phalanx, the middle phalanx, and the thumb and weakness of thumb abduction and opposition. With passage of time, the muscles of the thenar eminence atrophy, leaving the hand with a flattened and “apelike” appearance (see Fig. 50-24C). Sensory Innervation.: The typical distribution of the sensory nerves to the hand is shown in Figure 50-25. Because some overlap occurs between various sensory nerves, it is preferable to test sensation in the areas least likely to have dual innervation. The anatomic area of least ulnar variation and overlap is the volar tip of the little finger. The median nerve exclusively innervates the volar tip of the index finger. The dorsal first web space is entirely within the radial nerve distribution. Several methods exist to assess sensation. Two-point discrimination is one such method, although both the accuracy and objectivity of this test have been called into question.14 An uninjured hand is able to distinguish two points that are 2 to 5 mm apart at the fingertips and 7 to 10 mm apart at the base of the palm. The dorsum of the hand is the least sensitive region, with a normal threshold at 7 to 12 mm. Two-point threshold distances wider than these ranges indicate impaired sensory function.14 The threshold and two-point discrimination tests may be of limited value in children, patients with heavily calloused fingertips, uncooperative patients, comatose patients, patients in severe pain, or suspected malingerers. In such patients, submerging the hand in water and observing the skin for the development of wrinkles has been offered as a way to diagnose nerve impairment because denervated skin will not wrinkle.15 The fingertip generally is defined as the area distal to the insertion of the flexor profundus and extensor tendons (Fig. 50-26). The pulp is the tissue of the fingertip between the volar skin and the distal phalangeal bone. The fingertip is well padded by adipose tissue and is covered by highly innervated skin that is tethered to the distal phalanx by a series of fibrosepta. The dorsal skin is thinner and less vascularized than the volar skin. Sensation is supplied by nerves that travel with arteries bilaterally along the radial and ulnar aspects of the fingers. The arteries branch to form volar anastomoses or arches similar to those in the palm. Dorsal branches supply the nail bed and matrix. The nail bed complex is important in providing additional stabilization of the palmar soft tissues against compression and shear forces. The nail grows from the nail matrix along the nail bed and is firmly adherent to the bed. It is now believed that the entire nail bed is active in the generation and migration of the nail. As new nail forms, it glides forward over the nail bed at a rate of approximately 0.5 to 1.2 mm per week (toenails grow much more slowly). The nail itself is a hard, firm, and relatively translucent structure; the underlying vascular tissue showing through gives the nail its pink appearance. A smooth nail bed is essential to normal function. If the nail bed sustains injury that is not repaired accurately, granulation tissue forms scar that impedes normal nail production and growth. The result may be a split or absent nail that is cosmetically unappealing and sometimes functionally debilitating.16 The initial evaluation of an acutely injured hand is crucial because it affords the best opportunity for accurate assessment of the extent of damage and for restoration of altered anatomy.17 Evaluation of any hand injury should begin by obtaining the historical facts of the patient’s age, occupation, hand dominance, and previous hand impairment or injury. In traumatic injuries, elapsed time since the injury, mechanism of injury, posture of the hand at the time of injury, and treatment before arrival in the ED all are useful data. In nontraumatic problems, pain, swelling, sensory change, contracture, timing of symptoms, presence of similar symptoms in other extremities, aggravating or alleviating factors, and functional impairment are useful historical points. A review of the medical history and a review of systems complete the evaluation. After a detailed history is taken, the entire extremity should be exposed and evaluated when the hand is examined. A system of priorities, based primarily on threat to ultimate function, should direct the sequence of the examination. In order of priority, the examination includes evaluation of vascular and neurologic integrity, skin cover, skeletal stability, and joint and tendon function (Box 50-1). The general appearance of the hand should be noted, with focus on its color, presence of swelling or edema, and any abnormal posture or position. In traumatic injuries, the precise area of maximal tenderness should be localized. Rotational, angular, and shortening deformities should be noted with regard to direction and extent. Angular deformity may be seen best with the fingers in full extension. Rotational deformity is best observed during digital flexion. Digital or wrist block anesthesia may be helpful in some cases to accurately assess fracture deformity and stability during digital motion and, if necessary, stress testing. Open wounds should be assessed with regard to location, relationship to skin creases, direction and viability of skin flaps, extent of skin loss, degree of contamination of the wound, and extent of soft tissue injury. The examiner should have good light, adequate exposure, and a nearly bloodless field for a thorough evaluation. The complete examination also may require an evaluation of active shoulder motion, elbow motion, and pronation and supination of the forearm and assessment of the contralateral hand. Despite the development of numerous new and sophisticated imaging techniques, plain radiography remains the most important imaging modality for the hand and wrist. The standard radiographic series of the hand should include a posteroanterior, a true lateral, and an oblique projection (Fig. 50-27). With correct positioning, the bones do not overlap on the film, allowing complete evaluation of each area for visualization of fractures, subluxation, dislocation, deformities, and retained radiopaque foreign bodies.18 On a hand series, the wrist is not properly positioned for radiographic examination, and vice versa; if the patient has injuries to the hand and wrist, separate radiographic series should be obtained. For an adequate posteroanterior view, the forearm and hand should be fully pronated so that the palm rests flat on the film. This view forms the basis for all assessments but is poor at showing fractures of the articular surface of the metacarpal head. The lateral view normally is a radioulnar projection and is made by positioning the palm and forearm at 90 degrees to the film with the fingers splayed. This view is essential to show displacement of fracture fragments and joint dislocations. If the projection is not a true lateral view, joint dislocation, avulsion fractures, or fractures through the articular surface of the base of the phalanx may be overlooked. The oblique view is obtained with the hand and forearm pronated at 45 degrees to the film. It is particularly useful for assessing dislocation of the MCP and CMC joints and fractures at the base of the metacarpal bones. When injury is confined to the distal end of a single digit, radiologic evaluation should be limited to that digit, but the same projections are used (Fig. 50-28). Special views are used to diagnose specific injuries. The standard views of the hand do not give true posteroanterior and lateral projections of the thumb because the plane of the thumb is at 90 degrees to that of the fingers. Separate posteroanterior and lateral views of the thumb should be requested. The posteroanterior projection of the thumb is obtained with the hand and forearm hyperpronated so that the dorsal surface of the thumb and the thumb metacarpal rests flat on the film. The lateral view is obtained by pronating the hand and forearm to allow the lateral surface of the thumb to lie on the film. Stress views are used most often to rule out ligamentous injury to the first MCP joint. Localized widening of the joint space or subluxation may indicate a significant collateral ligament injury. Plain radiographs taken in multiple projections can help detect and localize soft tissue foreign bodies. Whether an object can be visualized will depend on its composition, configuration, size, and orientation. Many foreign bodies encountered in the ED, including almost all glass, are more dense than soft tissue and can be readily seen on plain radiographs.19 Plastic and wood foreign bodies are notable exceptions, with many of these objects being radiolucent. The bones of the hand are the most commonly fractured bones in the body. Radiologic evaluation of significant hand injuries is mandatory. Any hand injury that causes swelling should be evaluated radiographically with a minimum of three views. Although the classification of hand fractures is difficult and at times confusing, it generally is done according to the nature and site of the fracture line and whether the fracture is open or closed (Fig. 50-29). In general, transverse fractures have a stable configuration. Spiral, oblique, and comminuted fractures are unstable. The degree of displacement also is an indicator of potential fracture instability. Fractures of inherently unstable configuration may be stable if they are nondisplaced or only minimally displaced because the periosteum is undamaged or minimally disrupted. Displacement is defined by the deformity it creates and can result in rotation, angulation, shortening, or a combination of these fractures. Although shortening has an adverse effect on muscle tension, the hand accommodates more easily to this component of deformity than to others.18 Pathophysiology and Clinical Features Fractures of the distal phalanx are the most common fractures of the hand. They occur most often as a result of crush or shearing forces, usually as a sports-related injury in children and adolescents, industrial accidents in adults, or accidental falls in elderly persons.20 Distal phalangeal fractures are classified as extra-articular fractures (longitudinal, transverse, and comminuted) or intra-articular fractures. The most common location for these fractures is the distal tuft (Fig. 50-30). Because the mechanism of injury is usually direct trauma, tuft fractures often are comminuted and usually are associated with soft tissue injury to the nail, nail bed, and nail matrix.21 Supporting fibrous septa that radiate from the bone to the skin prevent displacement of fracture fragments and act to contain soft tissue swelling, contributing to the severe pain that can accompany these fractures. Examination typically reveals tenderness and swelling over the distal phalanx, including the pulp. Treatment of most fractures of the distal phalanges is directed toward the accompanying soft tissue injury. Closed tuft fractures need only symptomatic treatment with elevation (to reduce swelling) and analgesics. Fracture immobilization is rarely necessary; however, a short volar splint or hairpin splint (Fig. 50-31) is recommended for 2 to 3 days to protect the tip of the finger from further trauma and allow swelling without constriction. Immobilization should not include the PIP joint. Transverse shaft fractures with angulation or displacement may be irreducible because of interposition of soft tissue. Closed reduction may be attempted with dorsal traction on the distal fragment followed by immobilization with a volar splint and repeat radiographs for documentation of position. If this approach is unsuccessful, referral to a hand surgeon is indicated for Kirschner wire fixation.21 Distal phalanx fractures generally are uncomplicated; however, distal phalanx fractures that appear innocuous can result in prolonged morbidity, especially if associated with soft tissue crush injury. In a long-term follow-up series, DaCruz and associates22 showed that at 6 months 31% of tuft fractures had not healed radiographically and 70% of all patients had bothersome symptoms, including numbness, hyperesthesia, and cold sensitivity. Trauma to the nail bed may result in abnormal nail growth despite exact tissue approximation. Failure to recognize and extricate an entrapped nail bed in the fracture site may result in nonunion of the fracture. Osteomyelitis from open fractures is a rare but potentially serious complication. Pathophysiology and Clinical Features Because the anatomy, mechanism of injury, and treatment for proximal and middle phalangeal fractures are similar, these fractures are discussed together. The proximal phalanx has no tendinous attachments. Fractures in this region have a typical volar angulation resulting from forces exerted from the extensors and the interosseous muscles. The middle phalanx has two important insertions. The tendon of the FDS divides and inserts along nearly the entire volar surface of the phalanx, and the extensor tendon inserts on the proximal dorsal base of the middle phalanx. Because of this alignment, fractures at the base of the middle phalanx usually result in dorsal angulation, and fractures at the neck of the middle phalanx usually result in volar angulation.23 The mechanism of injury often determines the nature of the fracture; a direct blow is more likely to cause a transverse or comminuted fracture, whereas a twisting injury more often results in an oblique or spiral fracture. Associated injuries may include contusion or transection of digital nerves, vascular disruption, and tendon rupture. Intra-articular fractures include condylar fractures; comminuted fractures; dorsal, volar, or lateral base fractures; fracture-dislocations; and shaft fractures involving the joint. Extra-articular fractures involve the neck, shaft, or base of the phalanx. Although most phalangeal fractures may be easily seen, condylar fractures and displaced neck fractures are not always apparent on anteroposterior radiographs; oblique views may be needed to identify them.24 Rotational deformities are difficult to determine by radiologic study but may appear on the lateral view as discrepancies in the diameter of the shaft at the fracture site. Skeletal alignment can be assessed radiographically, but rotational alignment should be judged clinically by the relationship of the finger to adjacent normal fingers (Fig. 50-32). Symmetrical flexion of adjacent injured and normal fingers at their MCP and PIP joints is the best possible guide to accurate rotational alignment of the injured segment.23 Normally, all of the fingers of the closed fist except the thumb should point to the scaphoid. Alternatively, when the fingers are loosely flexed, the nails of opposing digits should lie in the same parallel plane (Fig. 50-33). The uninjured hand should be used for comparison. Similar to metacarpal fractures, phalangeal fractures require precise anatomic alignment to ensure a good result because of the intimate relationship of the flexor and extensor tendons to the phalanx.23 Appropriate treatment selection depends on accurate assessment of fracture stability. The angle of the fracture is an important factor in determining this stability. Transverse fractures usually are stable, whereas oblique fractures are inherently unstable. It also is important to ascertain whether the fracture has been impacted or displaced and what deforming forces are acting on it. If there is any question of the fracture’s stability, the digit should be anesthetized, and stress should be applied. Reduction of phalangeal fractures usually is not necessary because most are stable and nondisplaced.17 Patients with such fractures should be started on early protected motion as soon as pain subsides (within the first 3 to 5 days). Protection is provided by taping the injured digit to an adjacent, larger normal finger proximally, a form of dynamic splinting. This technique, known as “buddy-taping,” encourages the patient to move the finger and use the hand as normally as possible while the fracture heals (Fig. 50-34). If the fracture is displaced or unstable, it is not suitable for dynamic splinting. In general, treatment depends on the type of trauma and the ability to achieve a stable reduction. Phalangeal fractures that are satisfactorily managed by closed reduction can be immobilized by several methods. In such cases it is advisable to immobilize the wrist and the injured finger. Specific types of immobilization include circular cast, the Böhler method of incorporating a cast with an outrigger, gutter splints, and anterior and posterior splints (Fig. 50-35). The period of immobilization of phalangeal fractures should not exceed 3 weeks, to prevent stiffness and to minimize disability. In addition to temporary immobilization, ED management includes ice for comfort, elevation, analgesics, and referral for follow-up care. Repeat radiographs in 7 to 10 days are recommended to ensure that no delayed displacement has occurred. Unstable fractures that cannot be reduced by closed manipulation and maintained with external splinting require internal fixation. Midshaft transverse fractures tend not to be amenable to closed reduction; similarly, spiral oblique fractures and intra-articular fractures are inherently unstable and require surgical fixation if a significant portion of the articular surface is involved.25 Intra-articular fractures of the proximal metaphysis of the middle phalanx that have extreme comminution may require treatment in static or dynamic traction or external fixation with or without ancillary Kirschner wire fixation.25 Malunion is the most common bony complication of phalangeal fractures and may result from malrotation, volar or lateral angulation, or shortening. Malrotation usually is seen after oblique or spiral fractures of the proximal and middle phalanges and may require osteotomy through the phalanx or metacarpal for correction. Volar angulation of proximal phalangeal fractures greater than 25 to 30 degrees results in pseudoclawing. This deformity makes use of the hand awkward and is esthetically unacceptable. Other potential complications include diminished motion resulting from tendon adhesions and stiffness of the PIP joint after intra-articular fractures with incongruity.23 The hand can adjust functionally to dorsal angulation in the metacarpal equal to its motion at the CMC joint, plus 10 to 15 degrees in some patients. Because the index and middle fingers are immobile at their CMC joints, they may accommodate only 10 to 15 degrees of dorsal angulation. The ring finger usually has 20 to 30 degrees of mobility at its CMC joint and may accommodate 40 to 45 degrees of dorsal angulation. The small finger generally has 30 to 50 degrees of motion at its base and may accommodate 50 to 70 degrees of dorsal angulation. Finger metacarpals may tolerate 10 to 15 degrees of lateral angulation and 3 to 4 mm of shortening. Rotational deformity, most commonly seen in spiral and oblique fractures, is poorly tolerated. A small amount of rotational deformity can translate into a substantial digital overlap when the fingers are closed to form a fist. Just 10 degrees of malrotation may cause as much as 2 cm of overlapping (scissoring) of the fingers during flexion.17 Surgical intervention is indicated with 2 to 3 mm of shortening, 1 mm of articular surface step-off, greater than 25% articular involvement, or any degree of malrotation.23 Pathophysiology.: Fractures of the metacarpal head are rare. They usually occur as a result of direct trauma or crush injury and typically are comminuted.21 These fractures occur distal to the attachment of the collateral ligaments. Physical examination reveals tenderness and swelling over the involved MCP joint. Pain is increased if axial compression is applied along the extended digit. The presence of lacerations over the metacarpal heads is significant and suggests the possibility of an open fracture potentially caused by human bite injury. Diagnostic Strategies: Radiology.: Although routine radiographic imaging of the injured hand reveals most fractures, the metacarpal heads can be difficult to assess because of overlap on the lateral view. In such cases in which clinical suspicion of a fracture exists and the initial radiographic appearance is normal, the Brewerton “ball-catcher’s” view may be helpful.26 This view is obtained with the digits in 65 degrees of flexion at the MCP joints and the x-ray beam angled 15 degrees radially, projecting the metacarpal heads in profile. Occasionally, computed tomography also may be required to evaluate accurately the degree of displacement of intra-articular fractures at the MCP level. Management.: Emergency management of closed metacarpal head fractures consists of elevation, ice for comfort, analgesics, and immobilization of the hand in the “safe” or functional position, which balances the forces of the intrinsic muscles. In this position, shown in Figure 50-36, the wrist is extended 20 degrees, the MCP joints are flexed to 90 degrees, and the PIP and the DIP joints are extended. Referral to a hand surgeon for management and follow-up evaluation is required in all cases. Because these are intra-articular fractures, displacement by more than 1 to 2 mm predisposes the patient to a poor result; however, little consensus has been reached regarding optimal definitive treatment.27 Lacerations or puncture wounds over the dorsum of the MCP joint associated with a metacarpal head fracture should be considered open until proven otherwise. Such injuries often are caused by a clenched-fist injury and are highly contaminated wounds. Emergent consultation with a hand surgeon for operative débridement and irrigation is recommended. Prophylactic coverage with a cephalosporin is routinely recommended, although patients with highly contaminated wounds should receive penicillin with a β-lactamase inhibitor and an aminoglycoside.28 Several studies have found preoperative wound cultures to be of no value in predicting the risk of infection or identifying the likely pathogen, and some clinicians have abandoned their use.29,30
Hand
Perspective
Epidemiology
Principles of Disease, Functional Anatomy, Physiology, and Examination of the Hand
Structural Framework
Skeleton
Muscle and Tendon Function
Blood Supply
Nerve Supply
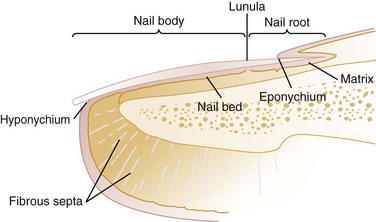
Fingertip
Nail
Clinical Features: Signs and Symptoms
Diagnostic Strategies: Radiology
Mechanisms of Injury and Management
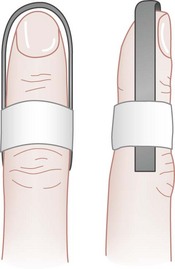
Distal Phalanx Fractures
Management
Complications
Proximal and Middle Phalangeal Fractures
Management
Complications
Metacarpal Fractures
Metacarpal Fractures of the Index, Middle, Ring, and Little Fingers
Metacarpal Head Fractures
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Hand
Only gold members can continue reading. Log In or Register to continue