Specialized Cervical Neuroanatomy
Chronic cervical pain arises primarily in the lower cervical vertebral motor segments from C5 to T1. One reason for this is that the strongest pathological anatomical changes are found here, because of the exceptional loading placed on the point of curvature at the cervico-thoracic junction. Another reason is that the spinal nerves, sympathetic plexus, and vertebral artery are found immediately adjacent to disorders of form and function within the vertebral motor segment.
Chronic headaches and dizziness also often arise from the head–neck junction. These are caused by joint capsule irritation, functional disorders, and deformations in the area of the atlanto-occipital and atlanto-axial joints.
There are seven cervical vertebrae and eight cervical spinal cord segments. As a result of developmental displacement, vertebral motor segments and spinal cord segments are not always found at the same level. The amount of displacement increases from cranial to caudal and is already clearly apparent in the lower cervical segments. In the lower cervical region, the spinal cord segments are found one vertebra higher up in relation to the spinous processes. The spinal nerve roots from C4 and downward run in an inferior and lateral direction until they pass through the intervertebral foramina. Segmental syndromes are named according to the affected spinal nerve root, the number of which also corresponds to the inferior vertebral body in the damaged vertebral motor segment. For example, in a C6 syndrome the C5/6 intervertebral disk is affected, in a C7 syndrome the C6/7 intervertebral disk and so on. The C8 nerve root exits via the C7/T1 intervertebral foramen (Fig. 7.1).
The precise identification of the affected segment is important for local treatment, cervical spinal nerve analgesia, and surgery. In the last few years it has been possible to determine the individual area of supply of each spinal nerve root in a purely empirical manner, as a result of discography, distension tests, and the many surgical interventions now being used in the diagnosis and treatment of cervical syndromes. Cervical-related nerve root irritation syndromes present mainly in amonoradicular form. Overlapping and mixed symptoms are possible when anastomoses are present under the spinal nerve, found partially inside the dural sac, and during the concurrent irritation of two or more nerve roots.
The C6, C7, and C8 nerve roots are most commonly affected. The dermatomes associated with nerve root irritation syndromes, radiating as far down as the hand, overlap in the upper arm and forearm (Fig. 7.2). All dermatomes have a posterolateral band of pain and paresthesia in the shoulder and upper arm in common. In the forearm, the C6 syndrome radiates more laterally and the C8 syndrome more medially. The C7 syndrome is found between the two (see Fig. 5.3).
Cervical Sympathetic Chain
The vertebral artery and the cervical sympathetic chain are found in the immediate vicinity of the uncovertebral region in the lower cervical vertebral motor segments. This is of particular clinical importance, as the close relationship explains why both can be affected during the process of aging and are considered possibly responsible for a complex neurovascular set of symptoms. The cervical sympathetic trunk is connected to the spinal nerves via the gray ramus communicans. It has three cervical ganglia responsible for the autonomic innervation of the head/neck region and the upper limbs. The upper ganglion encompasses the C1–C4 segments, the middle ganglion the C5–C6 segments, and the lower ganglion merges with the uppermost thoracic ganglion to form the stellate ganglion, encompassing the C7–T2 segments. The stellate ganglion is especially important as a major distributor. All efferent and almost all afferent sympathetic fibers coming from the head, neck, arm, and upper thorax run through this ganglion. Fibers travel cranially from here, including via the sympathetic arterial plexus of the vertebral artery.
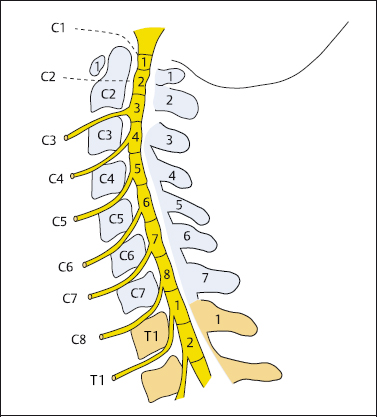
Fig. 7.1 Cervical spinal nerves and nerve roots. The spinal nerve roots from C4 downward run in an inferior and lateral direction until they pass through the intervertebral foramina. For example, the C5/6 intervertebral disk is affected in a C6 syndrome and the C6/7 intervertebral disk in a C7 syndrome.
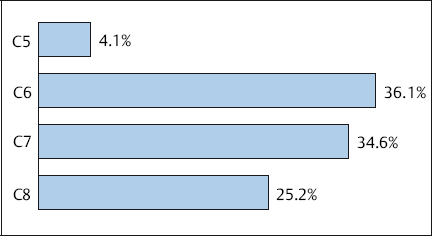
Fig. 7.2 The distribution of monoradicular CBS.
Studies by Hovelacque (1925), Wrete (1934), Kummer (1984), Kehr and Jung (1985), and Bogduk and colleagues (1988) have called attention to the entanglement of the cervical sympathetic chain, the cervical spinal nerve, and the vertebral artery. Sympathetic nerve fibers travel from all three cervical ganglia of the sympathetic trunk to the C4–C8 spinal nerves and partially encompass the vertebral artery (Fig. 7.3).
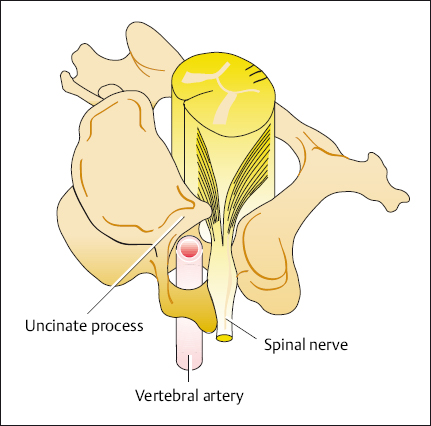
Fig. 7.3 The topographical relationship between the uncinate process, the vertebral artery, and the spinal nerve. Degenerative expansion of the uncinate process presses in on the spinal nerve and the vertebral artery, resulting in concurrent irritation of the sympathetic nervous system.
Basic Therapy for Cervical Pain
A wide range of methods is used to treat pain originating in the cervical spine. Polypragmasy is permitted during pain therapy because of the complex symptoms presented in the cervical syndrome. It is not the primary mechanical components alone that have to be treated: treatment is also required for secondary symptoms such as increased muscle tension, postural problems, and psychological changes. Causal and symptomatic treatment methods are administered in parallel.
When degenerative changes are already present, mechanical events are the primary cause of cervical syndromes. These events include sudden changes of position, hypermobility, and the protrusion or bending of intervertebral disks or bones. Causal therapy should always aim to combat one of these pathogenetic components. Secondary symptoms, such as increased muscle tension, postural problems, and psychological changes, must be treated alongside the primary mechanical components. Heat treatment, electrotherapy, massage, and analgesics should eliminate these secondary symptoms and disrupt the vicious circle of muscle tension caused by pain leading to more pain due to adaptive postures.
An important component of the treatment of cervical syndromes is the temporary use of a cervical collar, especially in the acute phase. Cervical collars prevent all movements that cause repeated mechanical irritation of the already irritated nerve root, the sensory receptors in the posterior longitudinal ligament, and the zygapophyseal joints from the first phase onwards. The neck posture can involuntarily cause pain during careless movements or when sleeping. In addition, the insulating collar accumulates body warmth in the shoulder/neck area and relaxes the muscles there.
Manual therapy primarily involves the use of manipulation with axial traction (Fig. 7.4a, b). When cervical manual therapy is primarily directed toward the zygapophyseal joint the thrust also affects the intervertebral disks, because the zygapophyseal joint and the intervertebral disk form a functional unit within the vertebral motor segment. Brief, firm traction forms the basis for almost all manual therapy techniques on the cervical spine and results in a reduction in intradiscal pressure. This in turn, has a suction effect that pulls any laterally or posteriorly displaced intervertebral disk tissue back into its original position. It is important, however, to consider the contraindications.
In causal pain therapy cervical traction is carried out either manually or with the help of traction devices. Many types of apparatus are available for cervical traction, some more expensive than others. Gentle traction, easily measured, is possible with the use of a Glisson sling. Its use in clinics and practices is well established (Fig. 7.5). The sling must fit the head well, with no pressure being applied to the chin or the larynx. In traction of the cervical spine the correct positioning of the patient is also important, just as it is in physiotherapy treatment. Glisson traction of the cervical spine is usually carried out with the patient lying supine. Less force is required in this position than in a sitting position, as the weight of the head is eliminated. The direction of pull should not be along the body’s axis, but rather more anterior, in terms of a slight cervical kyphosis, and when possible in the direction of the relieving posture.
Behavioral Guidelines for Patients with Cervical Pain: Back School
The rules of back school also essentially apply for patients with recurring pain in the shoulder/neck region. Rule 1 is important: To keep moving the neck and to avoid remaining in the same posture, especially when the position is unfavorable. The range of movement should not be too large, however, in order to avoid unnecessary irritation of the nerve root and zygapophyseal joint capsule. Activities where the posture and line of vision remain constant should be interrupted as often as possible. This especially applies to reading, watching television, working on a computer, and driving. Movements that aggravate pain, such as cervical extension and rotation, should be avoided at all costs, especially when chronically recurring pain is present. (It is particularly hard to avoid rotary neck movements while parking a car parallel with the curb. If they have to do this, patients should turn their whole body as much as possible, and use the rear view mirrors.) The remaining behavioral guidelines are essentially orientated toward maintaining optimal neck posture with mild flexion. The behavioral guidelines for patients with cervical pain are summarized in Table 7.1.
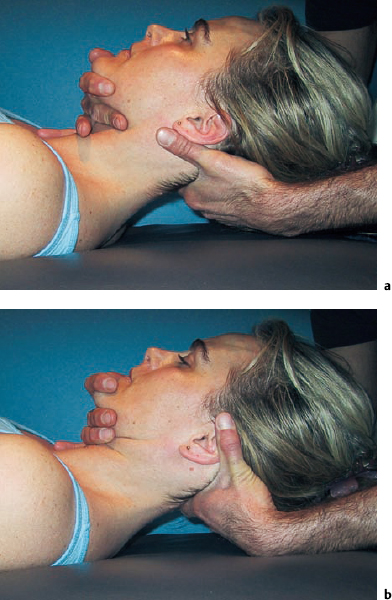
Fig. 7.4a, b Manual therapy for the treatment of pain originating in the cervical vertebral motor segments: Neural elements are relieved by traction in a neutral position (a) or in the direction of relief (b).
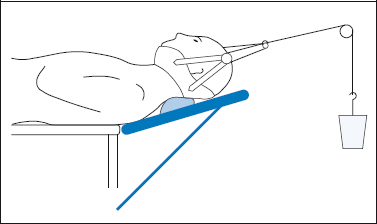
Fig. 7.5 Glisson kyphosis traction performed on the cervical spine as causal pain therapy.
In order not to further stimulate irritated cervical nociceptors and nerve roots, the only permissible movements are those that that allow a constant, nonvibratory, relieving neck posture in slight flexion. The best exercise is stationary cycling, ideally in front of a television screen placed to ensure a good head/neck position. Backstroke in a neck-relieving posture can also be permitted in the early stages of acute and chronic cervical syndromes.
|
Special Therapy for Cervical Pain
Local Cervical Pain Syndrome
By definition, local cervical syndromes are limited to the neck area, i. e., there is no radiation into the arms or head.
NOTE
In the local cervical syndrome, pain is felt at its origin. The clinical picture is therefore governed by nociception.
The nociceptors in the zygapophyseal joint capsules, the posterior longitudinal ligament, and the uncinate process are affected. The nociceptors at the cervical muscle insertions and the muscles themselves are secondarily involved. The causes are unstable segments and functional disorders in the cervical vertebral motor segments.
The pain is felt only in the shoulder/neck region and alters with changes in position, tense muscles, and limited mobility in the cervical spine. The symptoms can begin suddenly, e. g., when the head is abruptly turned, or they may increase gradually without a specific cause. During the subjective assessment, patients often mention chill and the effects of drafts among the precipitating factors. The patient can quite clearly localize where their pain is coming from during the examination. When the cranial cervical segments are affected, the pain lies within the area of supply of the dorsal ramis along the upper edge of trapezius, running from the occiput to the acromioclavicular joint.
When the lower cervical motor segments are irritated, a neuralgic-type component may also be present if pain between the shoulder blades is mentioned. This is mediated by the dorsal ramus. As well as the typical tender points, there is some noticeable tension in the entire shoulder and neck musculature and cervical mobility is limited. When an acute pain syndrome is present, an immediate motor reaction occurs and the patient adapts their posture with a slight amount of cervical flexion and head rotation. This posture should not be changed, as it represents a protective reflex which aims to prevent further irritation of the nociceptors.
 Pain Therapy for Acute Local Pain Syndromes
Pain Therapy for Acute Local Pain Syndromes
Pain should be treated immediately to prevent it becoming chronic. Peripherally acting analgesics block nociceptors and the distribution of pain signals at the source of pain. This treatment primarily involves the use of NSAIDs administered per os or as an infusion, when necessary. At the same time, local infiltration of the zygapophyseal joints, facet infiltration, and the infiltration of muscle insertions at the occiput, the edge of the scapula, and the acromioclavicular joint is recommended. The application of cold in the acute phase and heat for more enduring symptoms can be used in addition. Depending on the main focus of symptoms, these interventions can be supplemented by manual therapy, with traction in the direction of relief; the temporary use of a cervical collar so as to avoid neck positions that aggravate pain, especially at night; concomitant psychological therapy; and postural and behavioral training (back school) starting as soon as possible.
All methods are justified that relieve the patient’s acute pain and do not disrupt the patient’s normal way of life, i. e., patients should be able to sleep and to carry out activities of daily living, even if they may be slightly restricted. From this point of view, it is obvious that all methods that generally sedate the patient (central analgesics) or depend on bed rest are inappropriate. Interventions that affect the nociceptive region locally are the focus of attention.
Treating physicians should use the methods that they are most familiar with, so long as they fulfill the prerequisites mentioned (Table 7.2).
| Analgesics (NSAIDs) |
| Cervical collar (at night) |
| Cold (heat) |
| Local infiltration (trigger points, facet infiltrations) |
| Manual therapy (traction) |
| Heat |
| Local injections |
| Movement therapy |
| Back school |
| Progressive muscle relaxation |
| Exercise program |
 Pain Therapy for Chronic Local Pain Syndromes
Pain Therapy for Chronic Local Pain Syndromes
The indication that pain is becoming chronic is that it endures for weeks or months. Patients are unable to rest, especially at night. This in turn soon results in the development of associated psychological symptoms. The character of the pain changes, and as the disorder progresses further it is constantly present. Initially the pain is precisely located at the occiput and between the scapulae. It later develops into a diffuse pain that extends over the entire shoulder/neck region. The constant tension in the trapezius, levator scapulae, and rhomboid muscles causes insertion tendopathies at the occiput, the upper border of the scapulae, and the acromioclavicular joint. As the shoulder is secondarily involved in this process via the proximal muscles of the upper limb, chronification of pain can also occure here, and may even become an independent pain disease. The cervical sympathetic trunk is irritated at the uncovertebral region and acts as the primary mediator for the autonomic reaction, which takes the form of local paresthesias, circulatory disorders, and feelings of warmth/cold.
The clinical symptoms and the associated psychological symptoms change when the cervical syndrome pain is present for weeks or months on end. The chronic pain becomes the focus of attention and requires preferential treatment. Therapy primarily includes the use of heat treatment, exercises, and local infiltration at the sources of pain. Analgesics should be administered sparingly when chronic pain is present.
The primary aim of treatment for a chronic cervical syndrome is to break the vicious circle of pain–cramped muscles–adaptive posture–pain. Originally, the increased muscle tension was useful; however, it becomes independent via the vicious circle as the chronically recurring cervical syndrome progresses. This results in pain caused by constant muscle tension and insertion tendopathies Table 7.3 Massage, electrotherapy, infiltration of muscles using local anesthetics, and general muscle-relaxing measures are ideal for breaking the vicious circle at the muscular level. Progressive muscle relaxation according to Jacobson (1938) is the primary intervention.
Exercise Program
The exercise program for chronic cervical pain syndromes includes all movements that occur distant to the cervical spine and, if possible, do not cause axial vibration in the vertebral column. Suitable activities include stationary cycling, swimming in a neck-relieving posture, and all exercises carried out supine or in a reclined sitting posture. Jogging and road cycling are not initially recommended because of the vibrations associated with these activities. The same applies to housework and gardening, as involuntary quick cervical extension and rotation movements take place during these activities.
All types of sport that involve movement above head level must be treated with caution: e. g., tennis, volleyball, badminton. It is possible to start playing tennis by initially playing at the baseline without serving overhead, for example. Sport physiotherapists can provide specific instructions.
Psychological Components of the Chronic Cervical Syndrome
Several psychological factors act together in chronic cervical pain. The disorder is in close proximity to the CNS, which makes patients very concerned and anxious. Catastrophic thinking arises, for example, with thoughts of permanent disability and the threat of paraplegia. These thoughts are reinforced when physicians show patients radiographs of bony growths or—even worse—MRI images with posterior protrusions which are pressing on the spinal cord or may do so in the future.
On the other hand, trivializing or ignoring pain and pain-aggravating factors is also inappropriate. The sensitized nociceptors in the shoulder and neck region are irritated by even the slightest of inappropriate postures in extension and rotation. When patients wake up in the night with their neck involuntarily positioned in a hyperlordotic and rotated posture, the primary problem is not a psychological one. Stress modulates the vicious circle of pain and muscle contraction, playing an important role in the chronic cervical syndrome. Patients often report that their pain intensifies when they are stressed at work or in their private life. They feel more pain in the neck muscles, and more superiorly in the form of a tension headache. The increased frequency of neck pain and headaches, combined with the patient’s reduced ability to cope with stressful situations, often leads to an increasingly depressive mood. To prevent or disrupt this development, the patient should begin a muscle relaxation program before it is too late.
When the pathological muscle tension has eased, the use of exercises is appropriate when they are carried out carefully and in the pain-free range of movement. Postural and behavioral training during back school dictate that all movements and postures that can result in new nociceptive input must be completely avoided. In chronic cervical syndromes this is especially important for cervical extension and rotation movements. Chronic pain may continue to develop when the shoulder/neck region is exposed to cold or in the presence of psychological stress.
Pain Therapy for the Cervicobrachial Syndrome
Radiating pain in the arm that can be allocated to a specific dermatome indicates the presence of a neuralgic clinical picture. The ventral ramus of the spinal nerve is primarily affected. Cervicobrachial syndrome (CBS) is provoked either by an intervertebral disk prolapse or by hard, bony constrictions at the uncinate process. Bony constrictions occur significantly more often. The combination of segmental instability and uncovertebral osteophytes is of clinical importance.
The clinical symptoms generally appear gradually and are governed by a dermatome-related brachialgia that is position dependent. The afferent fibers in the spinal nerve have to first be converted to nociceptors. Night-time pain that is accompanied by a feeling of numbness and ants crawling along the dermatome is characteristic of this disorder. A chronically recurring progression is typical. The syndrome can be accentuated by external factors (e. g., acceleration injuries of the cervical spine) and a constantly maintained unfavorable posture (e. g., working at a desk, watching television).
The C6 syndrome involves pain radiating down to the thumb. In some cases the biceps tendon reflex is weakened. Radiation into the middle finger with possible weakness in the triceps and the triceps reflex, combined with thenar muscle atrophy, is characteristic of the C7 syndrome. In the C8 syndrome, pain radiates along the medial side of the hand. Sometimes a motor disorder of the finger flexors and the muscles of the hypothenar eminence may be present.
CBS is a primary chronic disorder. The conversion of a primary conducting nerve to a nerve with a nociceptor function already represents chronification.
The longer the condition remains, the less chance there is that simple interventions such as manipulation, traction, or a nerve root block can improve the pain rapidly. The constant nerve irritation leads to secondary symptoms with motor and autonomic reactions. Over time, central changes occur in the perception and processing of pain. In some cases, characteristics such as different positions affecting pain levels and the day–night pattern are no longer seen: Pain is felt permanently. Associated psychological symptoms appear. As in the local pain syndrome, chronification noticeable in the secondary muscle tension, insertion tendopathies, and the maladaptive postures found in the shoulder/neck/arm region.
The pain therapy used to treat CBS is not just directed toward the peripheral nociception. It aims, in addition, to affect the transmission and processing of pain signals. Local injection treatment with cervical spinal nerve analgesia is central in pain therapy for CBS.
It makes sense to directly tackle the source of pain at the intervertebral foramina or the uncovertebral region in acute as well as chronic cervical root irritation syndromes. To stop chronification, or interrupt the process at the spinal nerve root, daily spinal nerve analgesia is required for the first 10 days (including weekends). After the injection, patients should be placed in a position that relieves the affected part of loading for at least 30–60 minutes, ideally using Glisson traction. Further treatment is supplemented by physiotherapy with exercises starting in the pain-relieving position, electrotherapy, heat treatment, and progressive muscle relaxation exercises. The local injection treatment includes not only cervical spinal nerve analgesia at the affected segment, but also the infiltration of secondary sources of pain, e. g., at the border of the scapula, the occiput, and the deltoid muscle. The use of acupuncture is also established in the treatment of CBS. Outpatient and inpatient treatment plans are described in Chapter 13.
Treatment of Cervical Headaches (Cervicocephalic Syndrome)
A cervicocephalic syndrome (CCS) is a cervical syndrome accompanied by headache, dizziness, and sometimes dysphagia, hearing, and visual disorders. Headaches can be provoked by the stimulation of nociceptors in the zygapophyseal joints, neck muscles, and muscle insertions.
Possible sources of irritation include malpositioned joints at the head/neck junction, deviations of the cervical spine from the body axis, displacement of vertebrae, and constriction of the vertebral artery by lateral bony growths on the uncinate processes of C4–C7. The convergence of nociceptive afferents in the dorsal horn of the spinal cord or in the inferior trigeminus nerve nucleus can cause radiating facial pain, especially in the forehead, eye, and temple regions. The main clinical symptoms are persistent, chronically recurring headaches. The headaches are neuralgic in nature and have a chronic character right from the start. Predominant symptoms include headaches and dizziness that are position dependent, being worse when the neck is extended and rotated, in addition to the symptoms associated with the local cervical syndrome. This disorder is also described as cervical migraine because of the presence of severe headaches. In addition to the migraine-like ipsilateral headaches which radiate into the forehead, bilateral neuralgic headaches with an ipsilateral emphasis located at the back of the neck are also observed (Table 7.4).
The type of therapy to be used is dictated by the etiology and pathogenesis of the cervical headache. Headaches originating directly from the head itself are primarily treated by the administration of analgesics. In contrast, cervical headaches can be relieved simply by a change of posture and slight flexion of the neck. This position is adopted as the starting position for further physiotherapy and manual therapy interventions. Heat treatment to stimulate the circulation in the shoulder/neck region, electrotherapy, and progressive muscle relaxation are also used.
The source of pain is in the uncovertebral region of the lower cervical vertebral motor segments, so the use of cervical spinal nerve analgesia, with 8–10 injections at C7 and C8, is recommended. When the headache is felt more on one side, the injections are administered on the affected side. In the case of symmetrical headache, the injections are administered alternately on both sides.
A suitable exercise program conducted within the pain-free range of cervical movement is important, combined with the appropriate postural and behavioral training taught in back school. The inpatient and outpatient treatment plans used for CBS also fundamentally apply to the treatment of headaches arising in the cervical spine (see Chapter 13).
| Unilateral emphasis |
| Posture dependent |
| Episodic, short-term appearance |
| Local cervical syndrome symptoms are present at the same time |
Pain Therapy for the Posttraumatic Cervical Syndrome
An important application in pain therapy is the treatment of acceleration injuries of the cervical spine, often known as whiplash injuries.
NOTE
The symptoms arising from an acceleration injury of the cervical spine are identified as a posttraumatic cervical syndrome (PTCS). Whiplash is only one of the possible causes of symptoms. PTCS can arise from any type of force that causes comparatively severe bending or compression of the cervical spine.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







