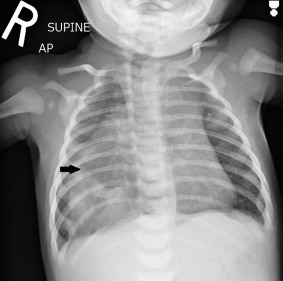
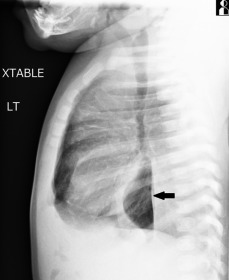
An 8-week-old term female infant presented to the emergency department with a 1-day history of multiple episodes of vomiting. The emesis began the day of presentation and it was nonbloody, nonbilious, and nonprojectile. She had decreased frequency of wet diapers, was more tired, but had no fever, runny nose, shortness of breath, or diarrhea. On physical examination, she was tired appearing and pale, but she had a strong cry and good perfusion and was easily consolable. Her abdomen was soft, nontender, and nondistended without organomegaly or palpable masses. On auscultation, she had faint scattered end-expiratory wheezing bilaterally, no increased work of breathing or respiratory distress, and a normal cardiac examination result. Chest radiographs were obtained and demonstrated an air- and fluid-filled structure in the right hemithorax, suggestive of a paraesophageal hernia ( Figures 1 and 2 ). An upper gastrointestinal contrast study confirmed the diagnosis ( Figure 3 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







