The American Board of Emergency Medicine (ABEM) gathers extensive background information on emergency medicine residency programs and the residents training in those programs. We present the 2017 annual report on the status of US emergency medicine training programs.
Introduction
The American Board of Emergency Medicine (ABEM) gathers extensive information on emergency medicine residency programs and the residents training in those programs. Survey data are collected annually from all emergency medicine programs accredited by the Accreditation Council for Graduate Medical Education (ACGME). Selected parts of the data are reported in this article. †
† This report reflects the status of data contained in the ABEM Residency Training Information Survey as of February 22, 2017. Data accuracy is contingent on survey compliance of participating 2016-2017 programs.
Also included in this report is information on accredited emergency medicine–sponsored fellowship programs reported by the ACGME.ABEM has several reasons for collecting and disseminating information on emergency medicine programs, residents, and fellows. As the evaluating and certifying arm of the specialty, ABEM seeks to meet the following goals:
- ▪
Collect accurate and comprehensive information pertaining to residents and residency programs
- ▪
Disseminate information that will aid policymakers and educators in establishing guidelines to improve the quality of graduate medical education in emergency medicine
- ▪
Gather background information on residents and fellows to understand the diversity in training programs and among residents
- ▪
Facilitate hypothesis generation and support research related to emergency medicine training
- ▪
Support the interface between residents and ABEM to facilitate certification activities
This annual publication serves the specialty of emergency medicine and the medical community at large by serving as a reference tool for evaluating the status and growth of emergency medicine residency and fellowship training and informing decisions to enhance the quality of training for emergency physicians.
Methodology
ABEM annually surveys all ACGME-accredited US categorical residency programs, ABEM-approved combined residency programs, and ACGME-accredited fellowship programs. Categorical programs are residency programs in a single primary specialty such as emergency medicine. There are currently 2 types of emergency medicine categorical programs, based on the number of postgraduate years (PGYs) that residents are in the program: PGYs 1 to 3 and PGYs 1 to 4. ABEM-approved combined programs consist of PGY 1 to 5 and PGY 1 to 6 program formats. The ACGME-accredited fellowships range between 1 and 3 years long. Information about new residents, fellows, and their respective programs is annually collected from July through October. Information about all enrolled residents and fellows is verified from December through January.
ABEM asks programs for the following information about each of their residents and fellows:
- ▪
Name
- ▪
Date of birth
- ▪
Sex
- ▪
Country of birth
- ▪
Medical degree
- ▪
Location of medical school (United States, international)
- ▪
Year of medical school graduation
- ▪
Dates of residency
- ▪
Citizenship
- ▪
Previous internships or specialty training
- ▪
Ethnicity (not required)
Programs are also asked for the following information:
- ▪
Number of applications received
- ▪
Interviews
- ▪
Residents or fellows enrolled
ABEM also reports the following data provided by the ACGME:
- ▪
Approved positions
- ▪
Type of program
- ▪
Length of fellowship
- ▪
Date of accreditation
Additional information on resident demographics is obtained from comparison data derived from the Graduate Medical Education report that is published annually in the Journal of the American Medical Association (JAMA) . Data are used with permission.
Analyses are performed with academic year and calendar year. For the most part, analyses related to a residency or a fellowship program are conducted with the academic year (July 1 to June 30). Analyses related to residents or fellows are based on their status as of December 31, referred to as “calendar year.” For clarity, the use of academic or calendar year is specified for each analysis throughout the article.
Methodology
ABEM annually surveys all ACGME-accredited US categorical residency programs, ABEM-approved combined residency programs, and ACGME-accredited fellowship programs. Categorical programs are residency programs in a single primary specialty such as emergency medicine. There are currently 2 types of emergency medicine categorical programs, based on the number of postgraduate years (PGYs) that residents are in the program: PGYs 1 to 3 and PGYs 1 to 4. ABEM-approved combined programs consist of PGY 1 to 5 and PGY 1 to 6 program formats. The ACGME-accredited fellowships range between 1 and 3 years long. Information about new residents, fellows, and their respective programs is annually collected from July through October. Information about all enrolled residents and fellows is verified from December through January.
ABEM asks programs for the following information about each of their residents and fellows:
- ▪
Name
- ▪
Date of birth
- ▪
Sex
- ▪
Country of birth
- ▪
Medical degree
- ▪
Location of medical school (United States, international)
- ▪
Year of medical school graduation
- ▪
Dates of residency
- ▪
Citizenship
- ▪
Previous internships or specialty training
- ▪
Ethnicity (not required)
Programs are also asked for the following information:
- ▪
Number of applications received
- ▪
Interviews
- ▪
Residents or fellows enrolled
ABEM also reports the following data provided by the ACGME:
- ▪
Approved positions
- ▪
Type of program
- ▪
Length of fellowship
- ▪
Date of accreditation
Additional information on resident demographics is obtained from comparison data derived from the Graduate Medical Education report that is published annually in the Journal of the American Medical Association (JAMA) . Data are used with permission.
Analyses are performed with academic year and calendar year. For the most part, analyses related to a residency or a fellowship program are conducted with the academic year (July 1 to June 30). Analyses related to residents or fellows are based on their status as of December 31, referred to as “calendar year.” For clarity, the use of academic or calendar year is specified for each analysis throughout the article.
Results
In academic year 2016-2017, there are 201 accredited US categorical emergency medicine residency programs. One hundred ninety-one categorical programs were surveyed by ABEM in 2016; 10 programs were not surveyed because their date of accreditation was after December 2016. Twenty-three combined training programs were also surveyed; one program was not surveyed because they will not begin training residents until July 2017. All surveyed programs, categorical and combined, submitted the requested program and resident information. The ACGME reports that there are 121 accredited emergency medicine–sponsored fellowship programs, with a total of 271 filled positions.
Emergency Medicine Residency Programs
Programs were first endorsed in the early 1970s by the Liaison Residency Endorsement Committee, and the ACGME began to accredit emergency medicine residency programs in 1981. Figure 1 illustrates the change in number of residency programs since the 1974-1975 academic year by program format type. The PGY 2 to 3 format ended in 1986-1987 because a 36-month residency was first required in 1988. The PGY 2 to 4 format was discontinued in 2011-2012. During the 2015-2016 academic year, there was an increase in residency programs because of the implementation of the Single Accreditation System (SAS). Under this agreement, residency training programs approved by the American Osteopathic Association (AOA) can become accredited by the ACGME. Of the 201 accredited US categorical emergency medicine programs, 152 (76%) have a PGY 1 to 3 program format and 49 (24%) have a PGY 1 to 4 program format. The numbers of PGYs 1 to 3 and 1 to 4 increased this year by 17% and 29%, respectively. This reflects both an increase in allopathic programs and the addition of the osteopathic programs under the SAS.
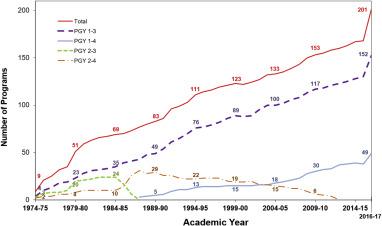
Table 1 illustrates the path from ACGME-approved positions through applications and interviews to enrolled residents during the last 5 years. Applications and interviews are the number reported by programs for the academic year. Last, the table contains the number of enrolled first-year residents, which increased 16% from calendar years 2012 to 2016.
| Academic Year | ACGME-Approved Positions | Applications | Interviews | Enrolled First-Year Residents |
|---|---|---|---|---|
| Program format 1–3 | ||||
| 2012–13 | 1,374 | 75,007 (nr=11) | 13,503 (nr=12) | 1,374 |
| 2013–14 | 1,428 | 83,667 (nr=11) | 14,812 (nr=11) | 1,403 |
| 2014–15 | 1,455 | 90,330 (nr=9) | 15,821 (nr=8) | 1,426 |
| 2015–16 | 1,547 | 97,344 (nr=12) | 16,957 (nr=12) | 1,476 |
| 2016–17 | 1,658 | 119,130 (nr=10) | 19,299 (nr=9) | 1,592 |
| Program format 1–4 | ||||
| 2012–13 | 476 | 25,313 (nr=3) | 4,846 (nr=3) | 476 |
| 2013–14 | 483 | 29,538 (nr=0) | 5,415 (nr=0) | 480 |
| 2014–15 | 500 | 30,664 (nr=1) | 5,647 (nr=1) | 500 |
| 2015–16 | 532 | 31,382 (nr=5) | 5,736 (nr=5) | 536 |
| 2016–17 | 576 | 39,230 (nr=6) | 6,678 (nr=7) | 555 |
Figure 2 presents the geographic distribution of accredited US categorical emergency medicine training programs by region within the United States. ACGME regions 5, 6, and 7 account for more than 53% of all emergency medicine residency programs.

The full list of current ACGME-accredited US categorical residency training programs in emergency medicine is contained in Appendix 1 . Appendix 2 has the number of programs and residents currently training by state.
Overview of Residents in Emergency Medicine
As of December 31, 2016, there were 6,633 residents enrolled in ACGME-accredited US categorical emergency medicine programs, with 4,458 (67%) in PGY 1 to 3 programs and 2,135 (32%) in PGY 1 to 4 programs. In addition, 40 residents are completing their PGY 2 to 4 program format.
From January 1, 2016, to December 31, 2016, there were 1,850 residents who graduated from emergency medicine programs. Figure 3 presents the trend in the number of residents and graduates during the past 5 calendar years. During this 5-year period, there has been a 17% overall growth rate in the number of residents enrolled in emergency medicine.
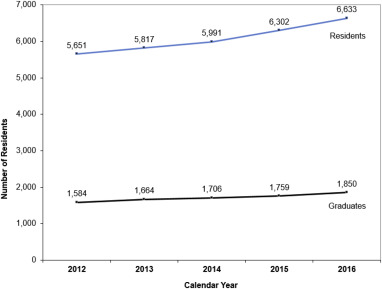
Table 2 contains the distribution of emergency medicine residents enrolled in each program type by their level within the program. Residents across both formats (PGYs 1 to 3 and 1 to 4) are fairly evenly distributed across levels, with slightly larger numbers in the first year and slightly smaller ones in each format’s final year.
| Level | PGY 1–3 | PGY 1–4 | Total |
|---|---|---|---|
| 1 | 1,589 | 546 | 2,135 |
| 2 | 1,475 | 529 | 2,004 |
| 3 | 1,394 | 541 | 1,935 |
| 4 | N/A | 519 | 519 |
| Total | 4,458 | 2,135 | 6,633 ∗ |
∗ Forty residents are completing their PGY 2 to 4 program format. This includes 11 residents in level 1, 13 residents in level 2, and 16 residents in level 3.
In each of the previous 5 years, physicians transferred in and out of emergency medicine categorical and combined programs. The numbers of residents transferring out of emergency medicine across categorical and combined programs were 47 in 2012, 33 in 2013, 31 in 2014, 42 in 2015, and 31 in 2016. The numbers of residents transferring into emergency medicine across categorical and combined programs were 42 in 2012, 29 in 2013, 38 in 2014, 41 in 2015, and 44 in 2016.
Figure 4 presents the composition of residents by sex and calendar year. In 2012, residents were 38% women and 62% men. In 2016, residents were 35% women and 65% men. The percentage of women residents steadily decreased during this period because the increase in proportion of men residents (23%) has outpaced that of women residents (8%).
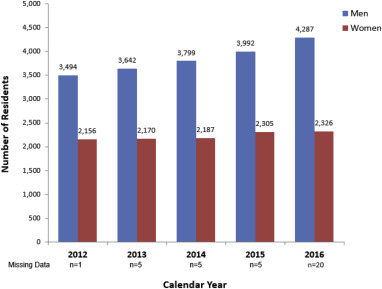
Figure 5 presents the distribution of age for residents for calendar year 2016. The median age that year was 31 years, with 59% (N=3,921) of residents aged between 27 and 30 years. As Figure 6 illustrates, the ethnic composition of residents during the past 5 calendar years has had little change, with the largest percentage of residents categorizing themselves as white (65%) and the second largest as Asian or Pacific Islander (12%).
Table 3 presents ethnic composition and sex comparisons for several specialty areas of medicine in the previous academic year (2015-2016). The comparisons are made with boards of various sizes, including specialties that represent the original American Board of Medical Specialties (ABMS) sponsoring boards of emergency medicine. The comparison data are derived from the Graduate Medical Education report that is published annually in JAMA and are used with permission. JAMA reports ethnicity with slightly different categories than those on the ABEM residency program survey. Comparisons between Table 3 and Figure 6 will also differ because of a difference in data sources, recency of the data, and the collection window (academic year 2015-2016 versus calendar year 2016, respectively). Figure 6 represents a slightly more recent data collection.
| Specialty | Emergency Medicine No. (%) | Family Medicine No. (%) | Internal Medicine No. (%) | Obstetrics and Gynecology No. (%) | Orthopedic Surgery No. (%) | Pediatrics No. (%) | Psychiatry No. (%) | Surgery, General No. (%) |
|---|---|---|---|---|---|---|---|---|
| Ethnicity | ||||||||
| Black | 289 (5) | 812 (8) | 1,379 (6) | 495 (10) | 141 (4) | 527 (6) | 371 (7) | 470 (6) |
| American Indian/Alaskan Native | 12 (<1) | 32 (<1) | 15 (<1) | 9 (<1) | 8 (<1) | 10 (<1) | 15 (<1) | 22 (<1) |
| White | 4,316 (73) | 6,159 (59) | 10,787 (46) | 3,442 (68) | 2,786 (77) | 5,359 (62) | 2,808 (54) | 5,518 (66) |
| Asian | 888 (15) | 2,427 (23) | 9,166 (39) | 724 (14) | 475 (13) | 2,039 (24) | 1,497 (29) | 1,598 (19) |
| Native Hawaiian/Pacific Islander | 1 (<1) | 22 (<1) | 15 (<1) | 4 (<1) | 1 (<1) | 7 (<1) | 5 (<1) | 10 (<1) |
| Multiracial † | 183 (3) | 305 (3) | 465 (2) | 163 (3) | 99 (3) | 227 (3) | 143 (3) | 205 (2) |
| Other/unknown | 227 (4) | 602 (6) | 1,837 (8) | 224 (4) | 107 (3) | 492 (6) | 314 (6) | 489 (6) |
| Hispanic origin ‡ (not included in count) | 442 (7) | 889 (9) | 1,852 (8) | 506 (10) | 197 (5) | 778 (9) | 440 (9) | 707 (9) |
| Total Resident Physicians (does not include Hispanic origin) | 5,916 | 10,359 | 23,664 | 5,061 | 3,617 | 8,661 | 5,153 | 8,312 |
| Sex | ||||||||
| Male | 3,735 (63) | 4,692 (45) | 13,441 (57) | 855 (17) | 3,083 (85) | 2,330 (27) | 2,402 (47) | 5,148 (62) |
| Female | 2,181 (37) | 5,667 (55) | 10,223 (43) | 4,206 (83) | 534 (15) | 6,331 (73) | 2,751 (53) | 3,164 (38) |
| IMG | 330 (6) | 3,319 (32) | 9,270 (39) | 601 (12) | 62 (2) | 1,684 (19) | 1,622 (31) | 1,305 (16) |
∗ Source: Adapted from Brotherton SE, Etzel SI. Graduate medical education, 2015-2016. JAMA . 2016;316:2291-2310. Copyright © 2016. American Medical Association. All rights reserved.
† “Multiracial” refers to residents who have self-identified as more than one race.
‡ Following the US Census Bureau, the National GME Census asked for race and Hispanic ethnicity in 2 separate questions. A person of Hispanic ethnicity can be of any race.
Table 4 illustrates the distribution of various degree types earned by residents. During the past 5 years, the percentage of residents with DO degrees has increased slightly, with the relative proportion of MD degrees decreasing.
| Calendar Year | MD | DO | Other Degrees ∗ | |||
|---|---|---|---|---|---|---|
| No. | (%) | No. | (%) | No. | (%) | |
| 2012 | 4,891 | (87) | 691 | (12) | 69 | (1) |
| 2013 | 5,042 | (87) | 718 | (12) | 57 | (1) |
| 2014 | 5,210 | (87) | 723 | (12) | 58 | (1) |
| 2015 | 5,327 | (85) | 923 | (15) | 52 | (1) |
| 2016 | 5,477 | (83) | 1105 | (17) | 51 | (1) |
∗ Bachelor of medicine, bachelor of surgery, PhD, or a combination of these.
Table 5 presents the origin of birth and medical training status of residents during the past 5 years. Since 2012, foreign- and US-born resident numbers have increased by 19% and 16%, respectively.
| Academic Year | Foreign Born | US Born | ||
|---|---|---|---|---|
| No. | (%) | No. | (%) | |
| IMG | ||||
| 2012 | 146 | (38) | 241 | (62) |
| 2013 | 139 | (43) | 188 | (57) |
| 2014 | 144 | (42) | 199 | (58) |
| 2015 | 146 | (42) | 204 | (58) |
| 2016 | 145 | (39) | 229 | (61) |
| USMG | ||||
| 2012 | 603 | (12) | 4,603 | (88) |
| 2013 | 645 | (12) | 4,783 | (88) |
| 2014 | 670 | (12) | 4,926 | (88) |
| 2015 | 696 | (12) | 5,142 | (88) |
| 2016 | 745 | (12) | 5,372 | (88) |
Figure 7 presents the geographic location of residents currently training in ACGME-accredited US categorical emergency medicine training programs by the American Medical Association’s designated regions. A majority of residents (54%) are concentrated in regions 5, 6, and 7. More information at the state level is available in Appendix 2 .
Combined Programs
Table 6 contains data that ABEM collects from the various combined emergency medicine programs. In calendar year 2016, the combined training programs had the following numbers of residents enrolled: emergency medicine/internal medicine (N=123), emergency medicine/pediatrics (N=38), emergency medicine/internal medicine/critical care medicine (N=18), and emergency medicine/family medicine (N=20). Across all combined programs, there has been a 14% increase in the number of residents enrolled since 2012. A new combined training program in emergency medicine/anesthesiology will begin training residents in the 2017-2018 academic year. More information in regard to the state-level distribution of residents and combined residency programs is available in Appendix 3 .
| Calendar Year | Emergency Medicine/Family Medicine | Emergency Medicine/Internal Medicine | Emergency Medicine/Internal Medicine/Critical Care Medicine | Emergency Medicine/Pediatrics | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Men | Women | |||||||||
| No. | (%) | No. | (%) | No. | (%) | No. | (%) | No. | (%) | No. | (%) | No. | (%) | No. | (%) | |
| 2012 | 9 | (53) | 8 | (47) | 70 | (63) | 41 | (37) | 10 | (91) | 1 | (9) | 15 | (42) | 21 | (58) |
| 2013 | 11 | (58) | 8 | (42) | 71 | (63) | 42 | (37) | 11 | (73) | 4 | (27) | 16 | (46) | 19 | (54) |
| 2014 | 11 | (55) | 9 | (45) | 72 | (64) | 40 | (36) | 12 | (63) | 7 | (37) | 18 | (49) | 19 | (51) |
| 2015 | 12 | (57) | 9 | (43) | 80 | (69) | 36 | (31) | 14 | (64) | 8 | (36) | 18 | (46) | 21 | (54) |
| 2016 | 12 | (60) | 8 | (40) | 87 | (71) | 36 | (29) | 13 | (72) | 5 | (28) | 18 | (47) | 20 | (53) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






