
Wrist and Forearm Injuries
James R. Gardner and Carl R. Chudnofsky
Wrist injuries are among the most common emergency department (ED) complaints, are often difficult to accurately diagnose, and may result in decreased use of the associated hand if left undiscovered and untreated. Outcome depends on accurate assessment of the injury, appropriate initial management, and prompt recognition of those injuries that require immediate specialty consultation or outpatient referral.
To adequately diagnosis and treat wrist injuries a basic understanding of the underlying anatomy is crucial. The central portion of the wrist is composed of eight carpal bones connected by over 20 ligaments. With the exception of the pisiform (which is actually a sesamoid bone in the tendon of the flexor carpi ulnaris), the carpal bones lack direct muscular attachments. Instead, they function as a passive “intercalated” joint, whose movement is governed by muscles that originate on the radius and ulna and insert on the metacarpals.
To reduce this anatomic complexity, the wrist may be thought of in a simpler, more functionally oriented fashion. Specifically, the eight carpal bones may be grouped into four primary working units—the scaphoid, the lunate, the triquetrum, and the distal row (Fig. 40.1). Though it has important stabilizing functions, the pisiform may be neglected in this model, since it lies outside the plane of the other bones and is less important in defining wrist motion. The four bones of the distal row—the trapezium, trapezoid, capitate, and hamate—are tightly bound and for conceptual purposes, may be viewed as a single unit with the capitate at the center. The articulations of these four functional units, with each other and with the forearm, allow the bulk of wrist movement (1,2).
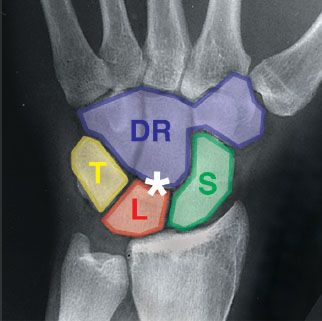
FIGURE 40.1 Key conceptual components of carpal anatomy. T, triquetrum; L, lunate; S, scaphoid; DR, distal row; *, space of Poirier. (Graphic overlay by Dr. Gardner J.R. X-ray from Moore KL and Agur A. Essential Clinical Anatomy. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2002. Courtesy of Dr. E.L. Lansdown, Professor of Medical Imaging, University of Toronto, Toronto, Ontario, Canada.)
The lunate and scaphoid bones attach to the radius, whereas the distal row attaches firmly to the metacarpals. The intracarpal ligamentous connections are arranged in an “oval” fashion; the distal row attaches to the scaphoid and triquetrum, which then attach to either side of the lunate. The central junction between the distal row and the lunate has no direct ligamentous attachments. This “space of Poirier” enhances mobility, but also provides a locus of anatomic instability when the wrist is injured (3).
While both the triquetrum and the scaphoid provide connection and rotation between the proximal lunate and the distal row, the scaphoid deserves particular attention. Unlike the relatively compact triquetrum, the scaphoid is an elongated bone that rotates through a wide arc during wrist movement. In addition, the scaphoid attaches directly to the radius, assuming significant load-bearing responsibilities. The scaphoid’s elongated shape and load-bearing function enhance its susceptibility to injury, making it the most frequently fractured carpal bone (4).
The forearm consists of the radius and ulna, although only the radius directly articulates with the carpal bones (the lunate and the scaphoid). The distal radius has three articular surfaces: the radiocarpal joint (RCJ), the distal radioulnar joint (DRUJ), and the triangular fibrocartilage complex (TFCC).
The RCJ is formed by a concavity in the distal radius where the scaphoid and lunate bones are seated. Radiocarpal ligaments originating on the radial styloid and on the edges of the RCJ concavity stabilize the radiocarpal connection. Fractures to these segments of the radius may destabilize the carpal bone complex.
The DRUJ is formed by a shallow concavity on the side of the radius where the ulna rests. The radius rotates about the ulna at this point.
The TFCC is a soft tissue complex located on the distal end of the ulna. It is composed of an articular disc that interposes between the ulna and the carpal bones, as well as ligamentous attachments that tether to the lunate and triquetrum distally and to the radius proximally. The proximal attachments serve to stabilize the DRUJ.
The interosseous membrane is a collection of fibrous bands that join the radius and ulna along their entire length. This membrane translates mechanical load from the radius onto the ulna, which in turn translates the load to the upper arm. Because of this tight membranous connection, injury to either forearm bone often results in a fracture of the other or causes a dislocation of either the distal or proximal joints (see Forearm Fracture–Dislocations below) (5).
The ulnar nerve and ulnar artery enter the volar aspect of the wrist next to the pisiform bone, running under the palmar carpal and pisohamate ligaments in a tissue space known as Guyon canal. The flexor retinaculum, which lies beneath the Guyon canal, forms the roof of the carpal tunnel. The carpal tunnel is the deepest volar space of the wrist and contains the median nerve, flexor pollicis longus, and all of the digital flexors. On the dorsal aspect of the wrist, the radial artery dives from its volar position in the forearm to run across the dorsal surface of the scaphoid and trapezium. It then circles back over the first metacarpal to form the deep palmar arch. The superficial branch of the radial nerve also crosses the dorsoradial aspect of the wrist, but unlike the radial artery it runs much nearer the surface, superficial to the fascial plane.
CLINICAL PRESENTATION
Patients with wrist injuries complain of varying degrees of pain, swelling, and limited range of motion in the wrist or forearm. Fractures of the distal radius or ulna may be confused with, or accompanied by, a carpal injury. The carpal bones in children are primarily cartilaginous; as such, carpal injuries are rare. Children are more likely to injure the weakest part of the wrist complex—the immature radial metaphysis or its epiphyseal growth plate. In contrast, the elderly more commonly injure the distal radius because of osteoporosis.
ED EVALUATION
Important historic information includes hand dominance; occupation and avocation; prior hand injuries and preinjury hand function; past medical history (e.g., diabetes mellitus, immunosuppression), including previous tetanus immunizations; and time, mechanism, and circumstances of injury. Mechanism of injury is particularly important, as the precise position of the hand and wrist during the injury help guide investigation and treatment.
On physical examination, surface anatomy should be used to identify and examine specific structures. The volar wrist crease marks the location of the proximal carpal bones and the flexor retinaculum. The EP should palpate the pisiform bone at the base of the hypothenar muscles just distal to the volar crease and the hook of the hamate in the soft tissue of the palm 1 cm distal and radial to the pisiform. On the dorsal side of the wrist the anatomic snuff box (ASB) is formed by the radial styloid proximally, the extensor pollicis brevis tendon radially, and the abductor pollicis longus tendon along the ulnar aspect. The scaphoid is palpated in the floor of this space. Moving in an ulnar direction from the radial styloid, a small bony prominence (the Lister tubercle), can be palpated on the dorsal radial surface. The scapholunate joint lies immediately distal to this prominence. With the hand in the neutral position, a small depression can be palpated midway between the base of the third metacarpal and the Lister tubercle. The capitate lies just distal to this depression. With wrist flexion, the depression disappears, and the lunate can be palpated proximally. The ulnar styloid is the largest bony prominence on the ulnar aspect of the wrist—the TFCC and triquetrum are located just distally (6).
It is important to note that damage to important underlying structures may occur despite innocuous-appearing surface wounds. Consequently, it is essential to explore lacerations and evaluate tendon function through a full range of motion. Neurovascular testing is best performed in the hand and is described in Chapter 41. The EP should always test neurovascular integrity before the instillation of local anesthetics.
Radiographs of the wrist and forearm should be obtained in all but the most trivial of injuries. On an adequately positioned posterior–anterior (PA) view (Fig. 40.2), the distal radius and ulna should not overlap, and the third metacarpal axis should be in line with that of the radius. The radial styloid should project between 9 and 15 mm beyond the DRUJ and should create an ulnar inclination of 15 to 30 degrees. A normal PA radiograph should also demonstrate three arcs outlining the carpal bones. The proximal and distal surfaces of the scaphoid, lunate, and triquetrum make up the two proximal arcs, whereas the distal third is formed by the proximal surfaces of the capitate and hamate in the midcarpal area. The carpal bones should be separated from one another by no more than 2 mm; increased intercarpal spaces imply ligamentous disruption and potential instability.
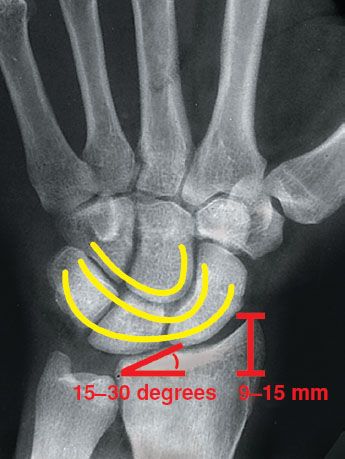
FIGURE 40.2 PA radiograph of wrist. Note 9 to 15 mm of radial styloid projection past the DRUJ, 15 to 30 degrees of ulnar inclination of the distal radius, three smooth arcs outlining the carpal bones, and no more than 2 mm of separation between carpal bones. (Graphic overlay by Dr. J.R. Gardner. X-ray from Moore KL and Agur A. Essential Clinical Anatomy. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2002. Courtesy of Dr. E.L. Lansdown, Professor of Medical Imaging, University of Toronto, Toronto, Ontario, Canada.)
On an adequately positioned lateral projection (Fig. 40.3), the palmar edge of the pisiform should lie between the scaphoid and capitate. The normal volar tilt of the radius is between 10 and 15 degrees and the radius, lunate, and capitate are arranged in a straight line (their axes should not vary by more than 10 to 20 degrees). The lunate appears as a “cup in a saucer” articulating with the distal radius, and the articular surfaces of the three bones create neatly overlapping “C”s. The scaphoid and lunate axes should form an angle of 30 to 60 degrees (the scapholunate angle); an angle of more than 70 degrees is abnormal and suggests scapholunate dissociation (7).
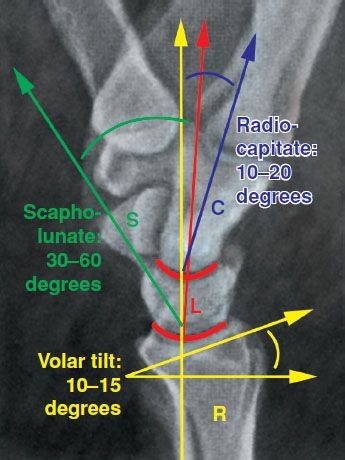
FIGURE 40.3 Lateral radiograph of wrist. Note 10 to 15 degrees of volar tilt of the distal radius (R); smooth “C”-shaped articulations between the radius, lunate (L), and capitate (C); 10 to 20 degrees of axial variance between the radius and capitate; and 30 to 60 degrees of axial variance between the scaphoid (S) and lunate. (Graphic overlay by Dr. Gardner JR. X-ray courtesy of Dr. E. Becker, University of Toronto, Toronto, Ontario, Canada.)
Oblique radiographs project the pisiform and triquetrum away from the other carpal bones making identification of fractures to these bones easier. Additional radiographic views (e.g., scaphoid view, carpal tunnel view) may be helpful in certain cases; however, CT imaging is increasingly being utilized to evaluate more subtle or complex injuries.
KEY TESTING
• Wrist x-rays (PA and lateral views; other views as needed)
• Forearm and elbow x-rays, if indicated
• Evaluate for ligamentous instability
• Evaluate for tendon disruption
• Evaluate for associated neurovascular compromise
ED MANAGEMENT
During evaluation, the EP should temporarily immobilize, elevate, and apply ice packs to the injured wrist. Analgesics should be administered to control pain and intravenous antibiotics administered for open fractures and dislocations and for severely contaminated or infected wounds. The EP should provide tetanus immunization as needed (see Chapter 21) and cover open wounds with sterile, moist gauze pending radiographs, surgical consultation, or wound closure.
Carpal Fractures
Carpal fractures account for 8% to 19% of all hand and wrist injuries. They are far more common in adults than in pediatric patients in whom the carpal bones remain largely cartilaginous. If not recognized and properly treated, carpal fractures may lead to significant disability, including arthritis, nonunion, loss of function, and avascular necrosis (AVN).
As noted previously, scaphoid fractures are the most common carpal bone fractures (60% to 80%). The injury is most often caused by an axial load or “fall-on-an-outstretched-hand ” (FOOSH), with the main impact on the thenar eminence. Patients usually complain of pain in the radial wrist, particularly with pressure or movement. Tenderness on palpation of the ASB is a common feature. Examining the wrist in ulnar deviation brings the scaphoid up from the floor of the ASB, making it easier to assess. Scaphoid loading (applying axial pressure on the thumb) elicits pain in many patients (eFig. 40.1).
The blood supply to the scaphoid is notoriously fragile, entering the bone distally via small branches off the radial artery. As a result, scaphoid fractures have an increased risk of proximal AVN, nonunion, and pseudoarthrosis (4).
Isolated lunate fractures are relatively rare; they occur more commonly in association with other wrist injuries. Given the anatomic location of the lunate in the space of Poirier, the application of significant force to the lunate is more likely to produce a perilunate or lunate dislocation (see Carpal Ligamentous Injury below). Patients will complain of pain in the middle of the wrist and axial loading of the third metacarpal causes pain. Examination reveals tenderness over the lunate.
Like the scaphoid, the blood supply to the lunate enters distally, giving these injuries a high incidence of AVN (known as Kienböck disease), nonunion, and subsequent carpal instability. Patients with Kienböck disease present with pain localized in the area of the lunate, stiffness, occasional swelling, and marked loss of grip strength; a history of significant wrist trauma is often lacking. Plain radiographs demonstrate sclerosis and collapse of the lunate.
Trapezium fractures are often due to a direct blow to the thumb or forced dorsiflexion. There is tenderness at the ASB and thenar eminence; decreased thumb pinch strength secondary to pain is another diagnostic clue. These fractures are often intra-articular and can extend distally, where they are analogous to a Bennett or Rolando fracture of the thumb metacarpal (see Chapter 41, “Hand Injuries”).
Nondisplaced scaphoid, lunate, or trapezium fractures are treated with immobilization in a thumb spica splint and timely follow up with a hand surgeon. Immediate consultation should be obtained for open and/or unstable fractures, fractures with displacement of ≥1 mm, and those associated with other wrist fractures or dislocations.
On the ulnar side of the wrist, triquetrum fractures are most often dorsal avulsion fractures due to a FOOSH, or they occur when rotation of the hand is suddenly resisted, causing the hamate or ulnar styloid to forcefully impact the triquetrum. Patients complain of dorsal wrist pain and are maximally tender just distal to the ulnar styloid. Dorsal triquetrum fractures are best seen on lateral or oblique radiographs of the wrist with the hand in slight pronation (a “triquetral view”) where the fractured fragment appears as a small piece of bone dorsal to the triquetrum. Triquetrum body fractures are less common and imply significant force. They are frequently accompanied by other fractures and/or ligamentous injuries.
Though rare, hamate fractures usually present with sudden pain to the ulnar wrist when a swinging motion (i.e., golf club, bat) has been abruptly interrupted. Pain is maximal over the hamate, which is located 1 cm distal and just radial to the pisiform. Pain is also often noted in the fourth and fifth fingers with active grasp or when flexion is resisted. The hook is fractured much more frequently than the body of the hamate; hook fractures are best demonstrated on a “carpal tunnel” view.
For both triquetrum and hamate fractures, the EP should carefully assess the integrity of the ulnar nerve and artery. Fractures of the hamate hook in particular may be associated with compression of Guyon’s canal. Treat uncomplicated fractures of the triquetrum or hamate with volar splinting in the neutral position and close hand surgery follow-up. Fractures that are unstable, displaced, open, or associated with other wrist injuries or neurovascular compromise require immediate specialty consultation.
Fractures of the pisiform, capitate, and trapezoid are extremely rare. Capitate fractures bear mention for two reasons: The capitate has a distal blood supply, placing it at risk for AVN, and the fracture is often missed owing to the more obvious surrounding bony and ligamentous injuries that frequently accompany it. The EP should splint these injuries in a short-arm thumb spica with the wrist in slight dorsiflexion and the thumb immobilized to the IP joint and be sure to consult with a hand specialist prior to discharge (8,9).
Occult Carpal Fractures
Studies have shown that 23% to 36% of patients with concerning examination findings after wrist trauma (e.g., ASB tenderness, significant wrist pain, or swelling) will have fractures that are not appreciated on initial x-rays (10,11). Consequently, the diagnosis of “wrist sprain” should be made with trepidation. About one-third of occult fractures involve the scaphoid; less-common sites include the distal radius, other carpal bones, and proximal metacarpals. MRI has been touted as the gold standard for diagnosis in such cases. Nevertheless, in the hands of an experienced radiologist, CT has also been found to have excellent sensitivity (95% to 100%) and negative-predictive value (12,13).
Traditional therapy for suspected occult fractures has been immobilization and close outpatient follow-up for repeat examination and plain radiographs. Recently, advanced imaging (e.g., MRI, CT) in the ED has been advocated as a more accurate and possibly more cost effective treatment option (14). Until definitive studies are performed, therapy for occult fractures is best guided by institutional policies, local practice, or personal preference.
Carpal Ligamentous Injury
Injuries to the carpal ligaments range from partial tears (“sprains”) to complete disruption accompanied by carpal dissociation or dislocation. As with carpal fractures, most ligamentous injuries are caused by a FOOSH mechanism. In 1980, Mayfield et al. (15) observed that such ligamentous injuries tend to develop in a predictable pattern that begins radially and proceeds in a circular fashion around Poirier’s space as more force is applied.
In Mayfield’s model, the proximal scaphoid ligaments are the first to be damaged, causing scapholunate dissociation. This leads to forward flexion and radial displacement of the scaphoid. Because of the resulting unopposed action of the triquetrum, the lunate and distal row rotate dorsally. This pattern is known as dorsal intercalary segment instability (DISI) (eFig. 40.2).
Clinically, patients complain of wrist pain, dorsal swelling, and wrist weakness. They may also note an unpleasant snapping sensation with wrist movement. However, overall range of motion may be preserved and the injury may appear relatively minor.
The PA wrist x-ray demonstrates widening of the scapholunate joint to >2 mm (“Terry Thomas sign”) (Fig. 40.4), as well as foreshortening of the scaphoid as it rotates into forward flexion causing the appearance of the “scaphoid ring” sign. On the lateral view, the scapholunate angle increases to >60 degrees, while the axis of the lunate becomes angled dorsally to the axis of the radius. Of note, isolated rupture of the scapholunate ligament may occur without causing these radiographic findings—the presence of such changes means that secondary supporting ligaments have been torn as well (16).
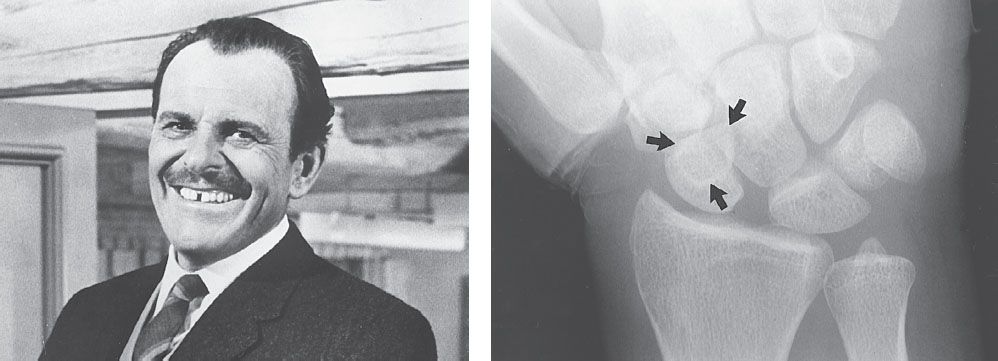
FIGURE 40.4 Scapholunate dissociation. Note the widened scapholunate space (“Terry Thomas” sign) and the foreshortened scaphoid with a “scaphoid ring” sign (arrows). Adjacent is British comedian Terry Thomas and his famous teeth. (Courtesy of the Bettmann Archive.)









