Wound Management
Judd E. Hollander and Adam J. Singer
Nearly 9 million patients with traumatic lacerations are treated annually in emergency departments (EDs) in the United States (1). The ultimate goals are to restore the physical integrity and function of the injured tissue in a cosmetically pleasing manner and to reduce the risk of infection. Treatment of these wounds involves a series of decisions that determine the methods of evaluation, wound preparation, wound closure, and postoperative care most likely to help attain these goals.
CLINICAL PRESENTATION
Lacerations occur predominantly in young adults; the majority of patients with lacerations are males (2). Most wounds are located on either the head or neck (50%) or the upper extremity (35%), usually involving the fingers or hands. The most common mechanism of injury is application of a blunt force, such as bumping the head against a coffee table. Such contact crushes the skin against an underlying bone, causing the skin to split. Other causes of injury include sharp instruments, glass, and wooden objects (2). While mammalian bites continue to receive much attention, they are a relatively infrequent cause of puncture wounds and lacerations (2).
ED EVALUATION
Evaluation of the patient with a traumatic wound begins with an expeditious, comprehensive assessment of the patient. This assessment can be divided into primary and secondary surveys, following advanced trauma life support algorithms. Unless the wound compromises the ABCs, formal wound evaluation and management occur during the secondary survey and management phase of the trauma evaluation.
Proper wound management begins with a thorough patient history. It is important to determine hand dominance and occupation. Host factors such as the extremes of age, diabetes mellitus, chronic renal failure, obesity, malnutrition, and the use of immunosuppressive medications all increase the risk of wound infection and can impair wound healing. Wound healing can also be impaired in the presence of inherited and acquired connective tissue disorders. The tendency of patients to form keloids should be ascertained because the development of keloids can result in a scar with less than acceptable cosmesis. Black and Asian populations are more prone to keloid formation (3).
Identification of the mechanism of injury is essential to help ascertain the presence of potential wound contaminants and foreign bodies that might result in chronic infection and delayed healing (3). Failure to diagnose foreign bodies in wounds is a leading cause of litigation against emergency physicians. Missed tendon and nerve injuries and failure to prevent infection are other common wound-related causes of litigation. In patients with scalp lacerations, a history of loss of consciousness and any neurologic complaints should be obtained. In patients with hand injuries, a history of neurologic deficits should be obtained to help predict the presence of tendon or nerve injury.
A careful history can also predict the likelihood of foreign bodies. Most organic and inorganic components of soil potentiate infection. However, sand grains are relatively innocuous. The black dirt on the surface of highways appears to have minimal chemical reactivity.
Crush injuries that tend to cause greater devitalization of tissue are more susceptible to infection than are wounds resulting from the more commonly seen shearing forces. Impact injuries with low energy levels may not result in division of the skin; they can, however, disrupt vessels and produce a hematoma and ecchymosis.
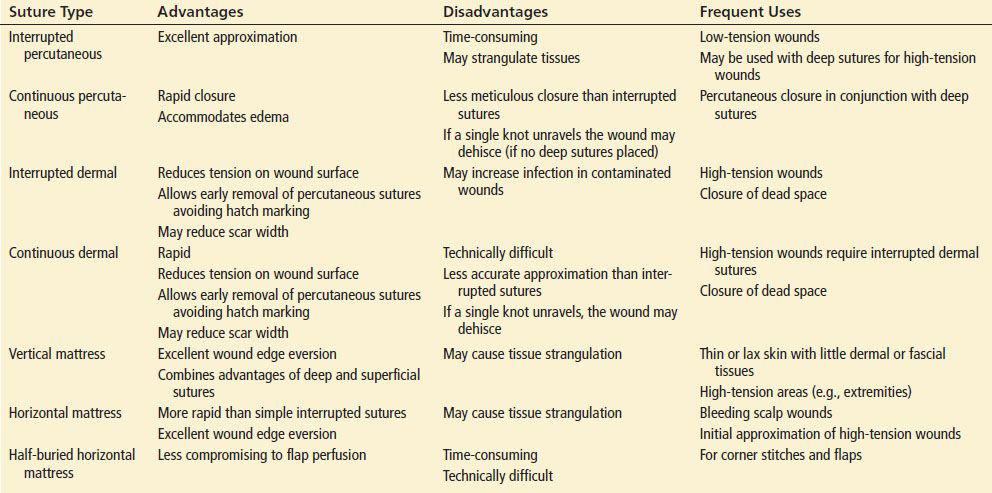
The presence of allergies to local anesthetics, latex, and antibiotics should be determined. The tetanus status of all patients should be assessed, and patients should receive immunization in accordance with current Centers for Disease Control and Prevention recommendations (Table 21.1). Before inspecting the wound, the emergency physician should question the patient regarding the time and mechanism of injury. The amount of time elapsed since the accident may influence treatment decisions.
TABLE 21.1
Recommendations for Tetanus Prophylaxis
Adequate wound examination should always be conducted in a field where bleeding has been controlled. One way to minimize the possibility of missing an injury to a vital structure is to start the wound examination with a careful neurovascular assessment of pulses, motor function, and sensation distal to the laceration. Finger tourniquets or a blood pressure cuff may then be used to obtain a bloodless field, but they should not be used for more than 30 to 60 minutes.
Moist areas of the body, such as the axillae, perineum, toe webs, and intertriginous areas, harbor millions of bacteria per square centimeter. Lacerations of the oral cavity are usually heavily contaminated with facultative species and obligate anaerobes. Wounds with fecal contaminants run a high risk of infection despite therapeutic intervention.
Wounds located on highly vascular areas, such as the face and scalp, are less likely to be infected than are wounds located in less vascular areas, such as the extremities (2). Lacerations of the scalp and face have a very low infection rate regardless of the intensity of cleansing (4).
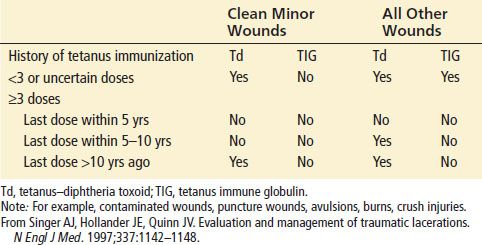
Wound location also contributes to the cosmetic appearance of the scar by affecting static and dynamic skin tensions (eFig. 21.1). Lacerations over joints are subject to large, dynamic skin tensions and will have a wider scar than will similar lacerations subject to less tension. Wounds that run perpendicular to the lines of minimal skin tension will also be prone to the development of wider and more visible scars.
eFIGURE 21.1 Langer lines of least skin tension.
eTABLE 21.1
Advantages and Disadvantages of the Common Wound-Closure Techniques
eTABLE 21.2
Characteristics of Nonabsorbable Sutures
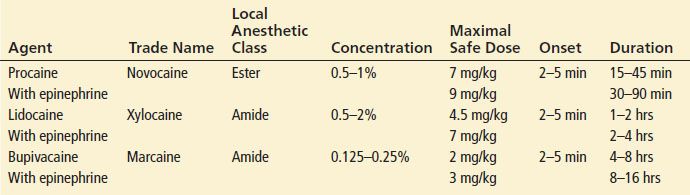
TABLE 21.2
Properties of Commonly Used Local Anesthetics

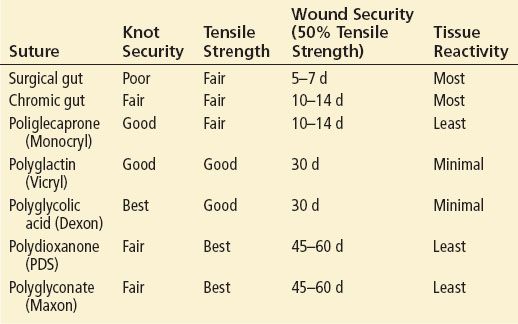
eTABLE 21.3
Characteristics of Absorbable Sutures
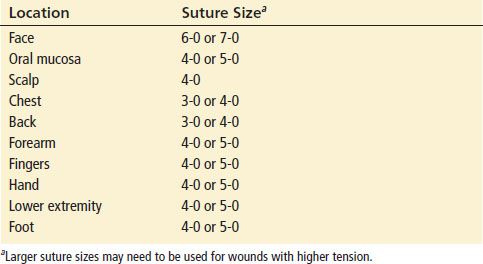
TABLE 21.3
Suture Selection Based on Anatomic Location
KEY TESTING
• The majority of lacerations require no diagnostic testing besides a history and physical examination.
• Depending upon the likelihood of a retained foreign body or fracture from the injury, radiography, ultrasound, or computerized tomography may be necessary.
ED MANAGEMENT
Aseptic Technique
The use of sterile gloves makes common sense, despite the lack of clinical evidence supporting their use (5,6). Though the practice of universal precautions is recommended in all patients, double gloving is recommended when caring for patients who can transmit serious infections (human immunodeficiency virus or hepatitis) to the healthcare provider.
Latex Allergy
Severe reactions in latex-sensitive individuals have resulted in fatalities. Populations that appear to be at increased risk for allergic reactions to latex include patients who have undergone multiple operations, patients with atopic disease, children with spina bifida, and medical personnel with frequent latex exposures.
Wound Examination
Wound examination should always be conducted under optimal lighting conditions and with bleeding in the field controlled. Wound examination should begin with a neurovascular assessment of pulses, motor function, and sensation distal to the laceration.
Bleeding should be controlled with direct pressure. When lacerations continue to bleed despite reasonable pressure, placement of a sphygmomanometer cuff proximal to the injury, with inflation to a pressure greater than the patient’s systolic blood pressure, will help contain bleeding to allow proper examination. Palpation of the bones adjacent to the injured site may detect tenderness, a defect, or instability consistent with an underlying injury. Radiography should be used to detect fractures. Detection of an open fracture will dictate a change from usual management because it will require the administration of systemic antibiotics and may require irrigation in the operating room. Wounds occurring adjacent to a joint should be carefully evaluated for joint violation. If in doubt, sterile fluid should be injected into the joint, and the physician should look for communication to verify violation of the joint space.
Amputated parts should be cared for as outlined in the chapters on hand injuries and replantation emergencies (Chapters 41 and 47). Digits should be covered with a protective saline-soaked dressing, placed within a waterproof bag, and then placed in a container of ice water for preservation and consideration of future reattachment.
Complicated injuries involving most open fractures, joint penetration, flexor tendon injuries, nerve injuries, or arterial injuries are often treated in the operating room. In most other cases, wound repair will occur in the ED.
The ultimate appearance and function of a scar can be predicted by the static and dynamic skin tensions on the surrounding skin (see eFig. 21.1). The most aesthetically pleasing scar occurs when the long axis of the scar is parallel to the direction of minimal tension, because the static skin tensions continually pull on the wound edges even after wound closure. The ultimate width of the scar is proportional to the magnitude of the static skin tensions.
An appreciation of the effects of various dynamic tensions can be used to determine the need for tension-relieving absorbable sutures in addition to the nonabsorbable skin closure.
Wound Anesthesia
Most lacerations will require some form of anesthesia prior to wound closure. All visibly contaminated wounds and wounds that will require anesthesia for closure should receive anesthesia prior to cleansing so that adequate mechanical removal of bacteria, soil, and other debris can be more readily accomplished.
Local Infiltration
The most common form of anesthesia for traumatic injuries is local infiltration. Unfortunately, local anesthesia is painful. To reduce the pain associated with local infiltration, several strategies can be employed. The addition of sodium bicarbonate to lidocaine (pKa, 7.9) in a 1:9 ratio increases the ratio of uncharged to charged ions and results in more rapid diffusion of anesthetic agent into nerve endings. It reduces the pain associated with local infiltration without altering the ability of host defenses to prevent infection (7). The use of warm anesthetic solutions, small needles, slow rates of infiltration, injection through the wound edges in noncontaminated wounds, and pretreatment with topical 4% tetracaine or lidocaine, epinephrine, and tetracaine (LET) are additional strategies that can be used to decrease the pain of infiltration (3,8).
For injection of local anesthesia, a 27- to 30-gauge needle attached to a 10-mL syringe should be used. The needle should be passed into the wound edge rather than the intact skin because wound edge injections are less painful. Full anesthesia to pinprick is present 5 to 6 minutes after subdermal injection. The local anesthetic agent should be instilled slowly to decrease the pain that accompanies tissue infiltration. The needle should be passed through the dermal tissue initially; then the anesthetic agent can be injected as the needle is slowly withdrawn. This technique minimizes distention and pain by providing a potential space for the anesthetic solution. Aspiration of the syringe before injection is recommended to prevent inadvertent intravascular injection.
Because the duration of local anesthesia induced by bupivacaine is nearly four times longer than that of lidocaine, bupivacaine (0.25%) should be used when longer durations of anesthesia are desirable (Table 21.2).
Vasoconstrictors such as epinephrine can be used as adjuncts to the local anesthetic agents. They will reduce bleeding and oozing within the laceration, which will make exploration and closure easier to accomplish. The addition of epinephrine also delays systemic absorption and increases the therapeutic window. Clinical studies have not found that the vasoconstriction associated with epinephrine use results in differences in infection rates. While traditionally these agents have been avoided in fingers, toes, and the penis owing to the risk of vasospasm and subsequent necrosis, more recent evidence suggest that their use is safe (9).
Regional Anesthesia
When the nerve supply to a wound is easily accessible, a regional nerve block is a valuable alternative to local anesthesia. The use of regional nerve blocks will prevent distortion of the wound edges, facilitating approximation and increasing the likelihood of an excellent cosmetic result. Regional nerve blocks can be accomplished by only one or two needle passages through skin proximal to the injury site. Regional nerve blocks of the supraorbital, infraorbital, and mental nerves are useful for facial lacerations; however, they are more painful and less reliable than local infiltration (10). Median, radial, and ulnar nerve blocks may be useful for lacerations of the hand. Digital or metacarpal nerve blocks can be used for finger lacerations. Regional nerve blocks can also be used for lacerations of the feet. Field blocks can be considered for more proximal extremity injuries.
A 27- or 25-gauge needle is preferred to a 30-gauge needle for a regional nerve block, because either one is more resistant to deflection during passage through tissue. The duration of sensory analgesia can be significantly prolonged when epinephrine (1%) is added to the anesthetic solution. When the needle puncture site is the mucous membrane, anesthetizing the mucous membrane with a topical anesthetic agent makes the introduction of the needle painless.
Topical Anesthesia
Topical anesthesia eliminates needle use and the risk of inadvertent needle sticks while allowing the application of painless anesthesia. Various combinations of lidocaine (1% to 4%), adrenaline (1:1,000 to 1:2,000), and tetracaine (0.5% to 2.0%) are as effective as eutectic mixture of local anesthetic cream (EMLA) (11,12). An EMLA has a slower onset of action, is more expensive than LET, and is not approved for use on injured skin; therefore, it is not recommended for use in the ED.
Preparation of Skin
Removal of the hair surrounding a laceration may facilitate meticulous wound closure. Because many bacteria normally reside in hair follicles, shaving the hair prior to repair may increase wound infection rates. Reduced damage to hair follicles may be achieved by using hair clippers instead of a razor. Removal of the eyebrow hair should be avoided because it does not always grow back. Additionally, the presence of hair serves as a guide to approximation of wound edges during laceration repair.
The skin surrounding the wound should either be cleansed with normal saline or disinfected with an iodophor (such as Betadine) or chlorhexidine; the physician should avoid contacting the wound itself with disinfectant. A recent study in the operating room demonstrated significantly reduced wound infection rates after skin preparation with chlorhexidine (13). Although these agents can reduce the bacterial concentration on intact skin, they appear to damage wound defenses, making the wound more susceptible to development of infection. Consequently, any contact of these agents with the wound should be avoided.
Debridement
Appropriate debridement is an important factor in the management of contaminated wounds. Retained devitalized soft tissue, fat, muscle, and skin can damage wound defenses and increase the likelihood of infection through the promotion of bacterial growth and the inhibition of phagocytosis. Identification of the exact limit of devitalized tissue in wounds may be difficult. Evaluation of the color, consistency, contraction, and circulation is useful.
In some anatomic sites, such as the trunk, debridement is best accomplished by complete excision of the skin and deep tissues. Heavily contaminated wounds with serpiginous defects in these regions can be converted to clean wounds by more generous tissue excision. When a heavily contaminated wound contains specialized tissues, such as the nerves or tendons that perform important physical functions, complete excision often is not feasible. In such instances, mechanical wound cleansing followed by excision of all fragments of tissue that are not clearly viable is indicated.
The benefits of debridement must be weighed against the consequences of excision of the tissue. Debridement of skin and underlying tissue leaves a significant soft tissue defect that makes reapproximation more difficult.
Assessment for Foreign Bodies
Metal, bone, teeth, pencil graphite, certain plastics, glass, gravel, sand, some fish bones, some wood, and some types of aluminum are visible on plain radiographs. Almost all glass fragments 2 mm or larger are visible on radiographs (14). If the wound was caused by metal or glass and no foreign body is found on wound exploration or on plain films, it is unlikely that a foreign body exists. Computed tomography (CT) and magnetic resonance imaging (MRI) are useful for identifying and locating objects that have densities similar to soft tissue. Sonography may also be useful, particularly for wooden foreign bodies.
Cleansing the Wound
The two basic methods of wound cleansing are hydraulic forces (irrigation) and direct contact (scrubbing).
Irrigation
Some debate exists over both the optimal method of irrigation and the preferred solution. The efficacy of wound irrigation is correlated with the pressure at which the irrigant is delivered to the wound. High-pressure irrigation (>7 pounds per square inch) successfully cleans wounds of small particulate matter, such as bacteria and soil. Such cleansing has reduced the infection rate of experimentally contaminated wounds. In contrast, low-pressure syringe irrigation, even with large volumes of fluid, demonstrates negligible capability for removing small particles (bacteria) but removes large particulate matter, such as detached devitalized tissue.
High wound impact pressures can be easily obtained using a 30- to 60-mL syringe and a 19-gauge needle or Zerowet splash shield (15). However, it must be noted that sustained high- pressure irrigation can result in tissue damage. As a result, at very high pressures, infection rates may actually increase.
For relatively clean wounds in highly vascularized areas containing loose areolar tissue, such as the eyelid, high pressures should be avoided. In fact, high-pressure irrigation has not been found to offer any advantages for cleansing clean, noncontaminated facial lacerations (4). Conversely, high-pressure irrigation is clearly indicated for contaminated wounds of the lower extremity. The choice of irrigation solution is relatively straightforward. Normal saline compares favorably with more expensive, less readily available alternatives. Because of their tissue toxicity, detergents, hydrogen peroxide, and concentrated forms of povidone–iodine should not be used to irrigate wounds. Irrigation of wounds with tap water results in comparable infection rates versus irrigation with sterile saline (16). Irrigation volume should be individualized based on patient characteristics and such wound characteristics as location and etiology. Use of a device designed to reduce splatter will minimize the healthcare provider’s risk of exposure to potentially infectious materials.
Scrubbing
Direct scrubbing of the wound with gauze or a sterile surgical brush helps remove both bacteria and particulate matter, which potentiate the risk of wound infection. However, scrubbing also contributes to the tissue damage and reduces the ability of the wound to resist infection. Therefore scrubbing should be reserved for highly contaminated wounds.
Use of Drains
The potential benefits of the use of surgical drains in a clinical setting must be weighed against its harmful effects. Drains evacuate potentially harmful collections of pus and blood from wounds. When no definite localized fluid collection exists, drains must be considered prophylactic, and their potentially harmful effects become more important. The general use of drains is not indicated in the management of most wounds in the ED.
Open Wound Management
The technique of wound closure largely depends on whether the wound has lost tissue and the risk of wound infection. With primary closure, the wound is immediately closed. Primary closure results in a reduction in healing time in comparison with other closure methods. It also may reduce the bleeding, inconvenience, and discomfort often associated with open wounds. Secondary wound closure, in which the wound is left open and allowed to close on its own, is particularly well suited for highly contaminated or infected wounds. Though this method may reduce the risk of infection, it is relatively slow and uncomfortable. Delayed primary (or tertiary) closure combines the advantages of both primary and secondary closures. The wound is left open for a period of 3 to 5 days, after which it may be closed if no infection supervenes. For wounds with associated significant tissue loss, grafts or flaps are often required to close the defect. These procedures are usually performed in the operating room.
Though there is a direct relationship between the time interval from injury to laceration closure and the risk of subsequent infection, the length of this “golden period” is highly variable (3). A study of forearm lacerations found that closure within 4 hours had a lower infection rate than later closure (17). A large series of pediatric patients (2,834 patients) with lacerations did not find a difference in infection rate for lacerations closed within or >6 hours from the time of injury (18). Facial lacerations healed well regardless of the time to closure. In contrast, trunk and extremity lacerations exhibited lower rates of healing if they were closed more than 19 hours from the time of injury (63% to 75%) as compared to earlier (75% to 91%) (19).
On the basis of these data, it seems appropriate to consider each laceration separately, taking the time from injury until presentation into account, along with laceration location, degree of contamination, risk of infection, and importance of cosmetic appearance, before deciding whether to perform primary wound closure. Wounds that are not closed primarily owing to a high risk of infection should be considered for delayed primary closure after 3 to 5 days, when the risk of infection decreases.
Wound Closure
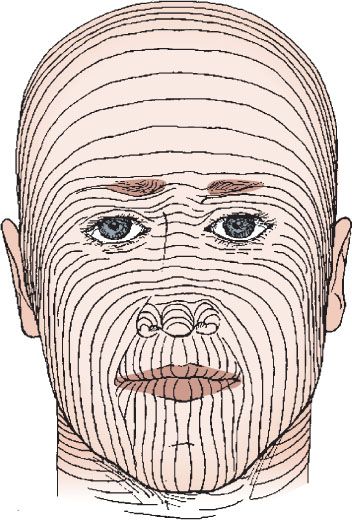
Careful handling of tissues and judicious use of electrocautery are necessary to reduce further trauma that may lead to poor cosmetic outcome (20). The optimal wound-closure technique varies with the clinical situation. Sutures are the most commonly employed wound-closure technique. Tissue adhesives can be used in up to one-third of ED laceration repairs. Staples and surgical tapes can be used in selected situations. The advantages and disadvantages of various wound-closure techniques are summarized in Table 21.4.
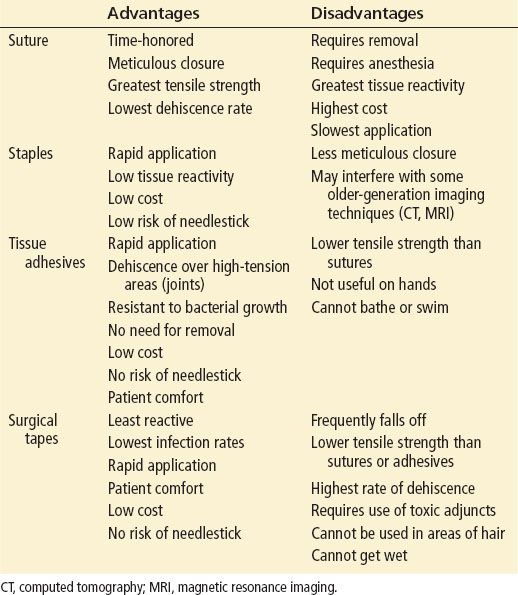
TABLE 21.4
Advantages and Disadvantages of the Various Suture Techniques