![]() Goals are to optimize wound strength, reduce inflammation, avoid infection, and minimize scar formation
Goals are to optimize wound strength, reduce inflammation, avoid infection, and minimize scar formation
![]() Time to wound cleaning is the most important factor
Time to wound cleaning is the most important factor
![]() To preserve viable tissue and restore continuity and function of tissue
To preserve viable tissue and restore continuity and function of tissue
CONTRAINDICATIONS
![]() Heavily contaminated wounds
Heavily contaminated wounds
![]() Presentation time for primary closure is after 12 hours for standard lacerations
Presentation time for primary closure is after 12 hours for standard lacerations
![]() Presentation time for primary closure is after 24 hours for lacerations of the face, scalp, or other highly vascular areas
Presentation time for primary closure is after 24 hours for lacerations of the face, scalp, or other highly vascular areas
![]() Wounds under high tension should not be closed by skin adhesives alone
Wounds under high tension should not be closed by skin adhesives alone
![]() Animal or human bite and most puncture wounds should not be closed on initial presentation
Animal or human bite and most puncture wounds should not be closed on initial presentation
RISK/CONSENT ISSUES
![]() Cleaning and repair of wounds cause pain
Cleaning and repair of wounds cause pain
![]() Local anesthetics are indicated for all wound repairs in conscious, alert patients
Local anesthetics are indicated for all wound repairs in conscious, alert patients
![]() Infection is always a risk in wound repair
Infection is always a risk in wound repair
![]() Wound repair always results in some scarring and can affect cosmetic appearance permanently
Wound repair always results in some scarring and can affect cosmetic appearance permanently
![]() Tendon, nerve, and vascular injuries can occur at time of initial injury or at time of repair
Tendon, nerve, and vascular injuries can occur at time of initial injury or at time of repair
![]() Risk of retained foreign body exists despite best methods of foreign body identification and removal, such as local exploration, radiographs, ultrasonography, and irrigation
Risk of retained foreign body exists despite best methods of foreign body identification and removal, such as local exploration, radiographs, ultrasonography, and irrigation
![]() Thorough exploration for foreign bodies must be performed and documented
Thorough exploration for foreign bodies must be performed and documented
![]() General Basic Steps
General Basic Steps
![]() Anesthetize wound
Anesthetize wound
![]() Clean wound
Clean wound
![]() Explore wound
Explore wound
![]() Consider radiography
Consider radiography
![]() Repair wound
Repair wound
TECHNIQUE
![]() Patient and Wound Preparation
Patient and Wound Preparation
![]() Position the patient to prevent falling or fainting during wound repair
Position the patient to prevent falling or fainting during wound repair
![]() Practice universal precautions
Practice universal precautions
![]() Prepare the surrounding skin with povidone–iodine solution and cover with sterile drapes before manipulation of any kind
Prepare the surrounding skin with povidone–iodine solution and cover with sterile drapes before manipulation of any kind
![]() Local Anesthesia: Lidocaine (1% or 2%) with or without epinephrine
Local Anesthesia: Lidocaine (1% or 2%) with or without epinephrine
![]() Epinephrine is contraindicated in areas of high risk for ischemia, such as fingers, ears, nose, toes, and penis
Epinephrine is contraindicated in areas of high risk for ischemia, such as fingers, ears, nose, toes, and penis
![]() Use small-gauge needle (25 or 27 gauge) to directly inject into subcutaneous (SQ) tissue within the laceration
Use small-gauge needle (25 or 27 gauge) to directly inject into subcutaneous (SQ) tissue within the laceration
![]() To decrease pain, inject through the wound and not through the skin
To decrease pain, inject through the wound and not through the skin
![]() Use adequate amount for anesthesia but avoid high volumes that will lead to significant tissue distortion, possible cosmetic embarrassment, or systemic toxicity
Use adequate amount for anesthesia but avoid high volumes that will lead to significant tissue distortion, possible cosmetic embarrassment, or systemic toxicity
![]() Maximum dose: 3 to 5 mg/kg 1% lidocaine, 7 mg/kg 1% lidocaine with epinephrine.
Maximum dose: 3 to 5 mg/kg 1% lidocaine, 7 mg/kg 1% lidocaine with epinephrine.
![]() Consider regional blocks for repairs in cosmetically important areas (face, hands, etc.) to avoid distortion of tissue
Consider regional blocks for repairs in cosmetically important areas (face, hands, etc.) to avoid distortion of tissue
![]() Wound Cleansing
Wound Cleansing
![]() Copious amounts of sterile water or sterile saline via high-power irrigation with a large syringe and splatter shield or an 18-gauge catheter. Tap water equally effective.
Copious amounts of sterile water or sterile saline via high-power irrigation with a large syringe and splatter shield or an 18-gauge catheter. Tap water equally effective.
![]() Wound Exploration
Wound Exploration
![]() After cleansing, the true depth of the wound is appreciated
After cleansing, the true depth of the wound is appreciated
![]() Look for deeper tissue involvement and explore the wound
Look for deeper tissue involvement and explore the wound
![]() If tendon or vascular structures are visualized, inspect through full range of motion, test for state of function, and document findings
If tendon or vascular structures are visualized, inspect through full range of motion, test for state of function, and document findings
![]() Radiography and/or Sonography
Radiography and/or Sonography
![]() If the possibility of underlying fracture and/or foreign body exists, image the affected area and document
If the possibility of underlying fracture and/or foreign body exists, image the affected area and document
![]() Select Method of Repair
Select Method of Repair
![]() 2-Octyl cyanoacrylate
2-Octyl cyanoacrylate
![]() Staples
Staples
![]() Sutures
Sutures
DERMABOND (LIQUID ADHESIVE)
![]() Indicated for simple wounds under low tension
Indicated for simple wounds under low tension
![]() Advantages
Advantages
![]() Ease of use, speed, and safety
Ease of use, speed, and safety
![]() No return visit necessary (sloughs off in 5 to 10 days and serves as own dressing)
No return visit necessary (sloughs off in 5 to 10 days and serves as own dressing)
![]() Much less painful
Much less painful
![]() Disadvantages
Disadvantages
![]() Moderate closure strength—cannot be used on joints or areas with high tension
Moderate closure strength—cannot be used on joints or areas with high tension
![]() Cannot be used in areas with excessive hair
Cannot be used in areas with excessive hair
![]() Caution when using around eyes to prevent accidental runoff into eyes
Caution when using around eyes to prevent accidental runoff into eyes
![]() Equivalent tensile strength at 7 days when compared to sutures
Equivalent tensile strength at 7 days when compared to sutures
![]() Procedure
Procedure
![]() Clean the wound
Clean the wound
![]() Approximate wound edges with forceps or fingers
Approximate wound edges with forceps or fingers
![]() Apply three to four layers along the wound length or perpendicularly to it (as strips)
Apply three to four layers along the wound length or perpendicularly to it (as strips)
![]() Maintain manual support for 60 seconds
Maintain manual support for 60 seconds
STAPLES
![]() Indicated for superficial scalp lacerations, linear lacerations on extremities, trunk, and wounds under low tension
Indicated for superficial scalp lacerations, linear lacerations on extremities, trunk, and wounds under low tension
![]() Advantages
Advantages
![]() Ease of use, speed, and safety
Ease of use, speed, and safety
![]() Easily removed and excellent tensile strength
Easily removed and excellent tensile strength
![]() Disadvantages
Disadvantages
![]() Less refined closure
Less refined closure
![]() Possible greater scarring
Possible greater scarring
![]() Uncomfortable removal (TABLE 69.1)
Uncomfortable removal (TABLE 69.1)
![]() No significant differences found with infection, healing, or patient acceptance when compared to suturing
No significant differences found with infection, healing, or patient acceptance when compared to suturing
SUTURE SIZE AND LOCATION |
Size | Superficial (nonabsorbable) | Deep (absorbable) |
2-0 | Suture chest tube |
|
3-0 | Foot | Chest, abdomen, back |
4-0 | Scalp, chest, abdomen, foot, extremity | Scalp, extremity, foot |
5-0 | Scalp, brow, mouth, chest, abdomen, hand | Brow, nose, lip, face, hand |
6-0 | Ear, lid, brow, face, mouth, nose |
|
![]() Procedure
Procedure
![]() Anesthetize, clean, and debride wound as necessary
Anesthetize, clean, and debride wound as necessary
![]() If necessary, close deep fascia with absorbable sutures with a buried knot
If necessary, close deep fascia with absorbable sutures with a buried knot
![]() Evert wound edges before placing staple, if possible utilizing the services of an assistant with forceps. Do not press too hard.
Evert wound edges before placing staple, if possible utilizing the services of an assistant with forceps. Do not press too hard.
![]() Allow the staple crossbar to sit 1 to 2 mm above wound edge
Allow the staple crossbar to sit 1 to 2 mm above wound edge
![]() Place enough staples to adequately appose tissue edges
Place enough staples to adequately appose tissue edges
SUTURES
![]() General Rules
General Rules
![]() Deep stitches require 3-0 or 4-0 absorbable sutures
Deep stitches require 3-0 or 4-0 absorbable sutures
![]() Skin closure requires 4-0 or 5-0 nonabsorbable sutures
Skin closure requires 4-0 or 5-0 nonabsorbable sutures
![]() Face, lips, and eyelid wounds: Consider 6-0 sutures
Face, lips, and eyelid wounds: Consider 6-0 sutures
![]() High skin tension areas: Consider 3-0 or 4-0 sutures
High skin tension areas: Consider 3-0 or 4-0 sutures
![]() Always select the smallest size that will hold the skin edges together
Always select the smallest size that will hold the skin edges together
![]() Nonabsorbable Sutures
Nonabsorbable Sutures
![]() Silk: Has the best knot security, the best tie ability, the least tensile strength, and causes significant tissue reactivity. Used in intraoral mucosa.
Silk: Has the best knot security, the best tie ability, the least tensile strength, and causes significant tissue reactivity. Used in intraoral mucosa.
![]() Ethilon: Has good knot security, good tensile strength, minimal tissue reactivity, and good tie ability. Best suited suture material for typical wound closure.
Ethilon: Has good knot security, good tensile strength, minimal tissue reactivity, and good tie ability. Best suited suture material for typical wound closure.
![]() Prolene: Poorest knot security, best tensile strength, least tissue reactivity, and fair tie ability
Prolene: Poorest knot security, best tensile strength, least tissue reactivity, and fair tie ability
![]() Absorbable Sutures
Absorbable Sutures
![]() Vicryl: Good knot security, good tensile strength, minimal tissue reactivity, best tie ability, and 30-day suture duration. Used for deep repair to reduce wound tension.
Vicryl: Good knot security, good tensile strength, minimal tissue reactivity, best tie ability, and 30-day suture duration. Used for deep repair to reduce wound tension.
![]() Surgical and chromic gut: Fair knot security, fair tensile strength, greatest tissue reactivity, poor tie ability, and 5- to 7-day suture duration. Used for intraoral wounds.
Surgical and chromic gut: Fair knot security, fair tensile strength, greatest tissue reactivity, poor tie ability, and 5- to 7-day suture duration. Used for intraoral wounds.
![]() Procedure
Procedure
![]() Anesthetize, clean, and debride wound as necessary
Anesthetize, clean, and debride wound as necessary
![]() Prepare the skin with povidone–iodine or chlorhexidine solution
Prepare the skin with povidone–iodine or chlorhexidine solution
![]() Minimize trauma by handling skin with toothed forceps and by using small sutures
Minimize trauma by handling skin with toothed forceps and by using small sutures
![]() Relieve tension by undermining with a scissor and by using layered sutures (FIGURE 69.1)
Relieve tension by undermining with a scissor and by using layered sutures (FIGURE 69.1)
![]() Subcutaneous Layer Closure
Subcutaneous Layer Closure
![]() Reapproximate fascia as needed
Reapproximate fascia as needed
![]() Close the SQ layer in sections, starting in the middle and then bisecting adjacent sections until adequate tension has been relieved from the skin edges
Close the SQ layer in sections, starting in the middle and then bisecting adjacent sections until adequate tension has been relieved from the skin edges
![]() Insert the suture at the bottom of the layer and draw it through to just beneath the dermis on the same side of the wound
Insert the suture at the bottom of the layer and draw it through to just beneath the dermis on the same side of the wound
![]() Reenter beneath the dermis on the adjacent side and draw through to the bottom of the SQ layer
Reenter beneath the dermis on the adjacent side and draw through to the bottom of the SQ layer
![]() Tie the knot such that it remains at the bottom of the wound, thereby preventing a palpable knot near the skin surface
Tie the knot such that it remains at the bottom of the wound, thereby preventing a palpable knot near the skin surface
![]() Interrupted Stitch
Interrupted Stitch
![]() Most commonly used stitch. If one fails, the rest will maintain closure.
Most commonly used stitch. If one fails, the rest will maintain closure.
![]() Insert the needle at 90 degrees to the skin surface and include sufficient SQ tissue in the bite and carry the suture through to the opposite side
Insert the needle at 90 degrees to the skin surface and include sufficient SQ tissue in the bite and carry the suture through to the opposite side
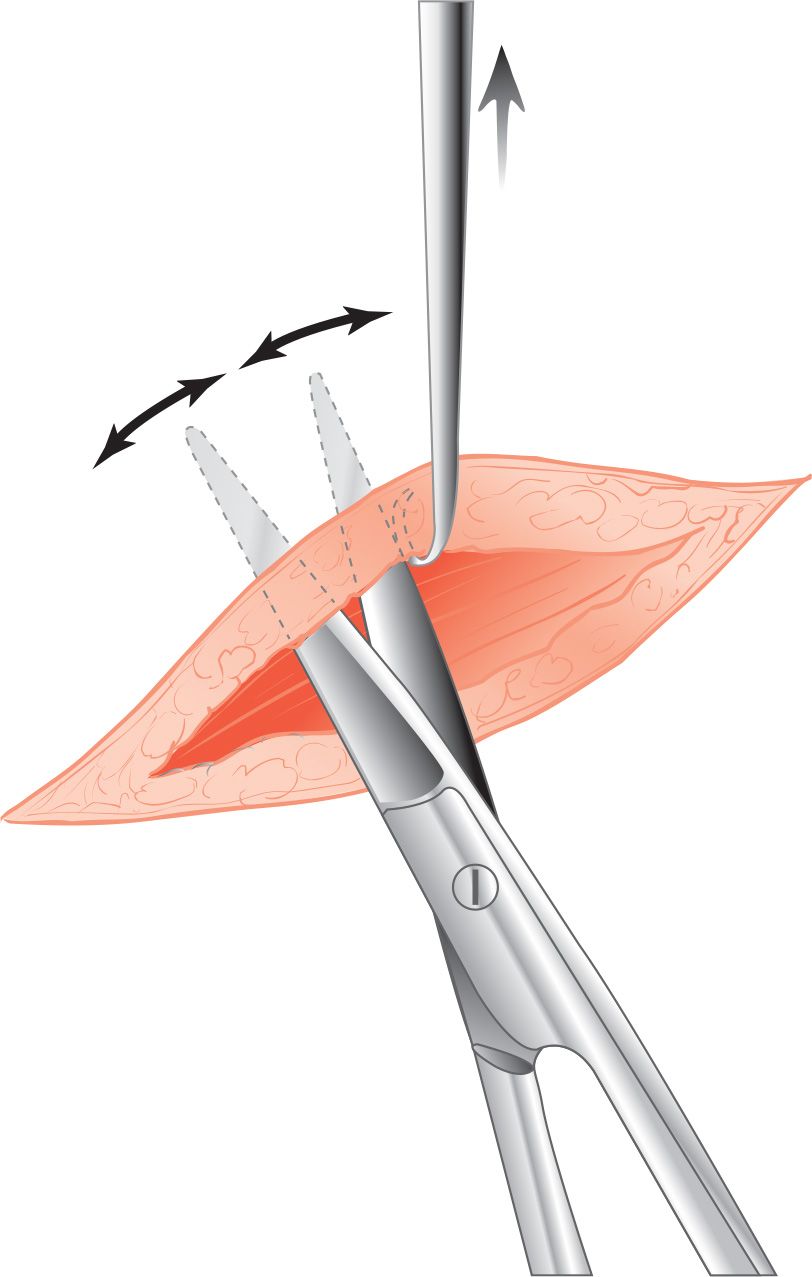
FIGURE 69.1 Undermining a wound reduces the degree of tension present after the repair. (From McNamara R, Loiselle J. Laceration repair. In: Henretig FM, King C, eds. Textbook of Pediatric Emergency Procedures. Philadelphia, PA: Williams & Wilkins; 1997:1152, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


