INTRODUCTION
Wheezing is a high-pitched sound that occurs when there is an elevation of airway resistance due to an obstructive process. The clinician must differentiate between stridor and wheeze because this determines location of the airway obstruction. Stridor is a sign of upper airway obstruction (above the thoracic inlet) that is more marked during inspiration, whereas wheeze signifies lower airway obstruction distal to the thoracic inlet that is more marked during expiration (see chapter 123, “Stridor and Drooling in Infants and Children”).1,2,3,4 Wheezing implies a generalized obstructive airway disease when diffuse and focal obstruction when localized. However, severe flow limitation may exist without wheezing, for example, the silent chest in a severe asthma exacerbation. Bronchiolitis is the most frequent cause of wheezing in infants, and asthma is the most frequent cause in children and adolescents.
RESPIRATORY PHYSIOLOGY
The nasal passages account for 50% of total airway resistance. Nasal resistance increases in the presence of nasal mucus or edema and may be clinically important in the infant with bronchiolitis. The conducting airways extend from the trachea to the terminal bronchioles and do not participate in gas exchange. The distal transitional and respiratory zones are the gas-exchanging units.
Lung tissue has elastic properties; functional residual capacity is the resting balance of stretch and recoil forces. Normally, at functional residual capacity, the tissue is relaxed at end expiration, and inspiration begins with minimal effort at the onset of inspiratory muscle contraction. Inspiration is an active process generated by the diaphragm and external intercostal muscles. During exertion, inspiration is aided by the use of accessory muscles including scalene and sternocleidomastoid muscles.5 Expiration is normally a passive process, facilitated by elastic recoil of the stretched lung.
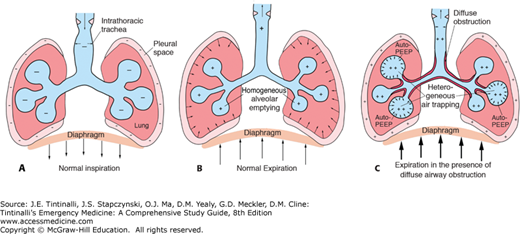
In the presence of diffuse (e.g., asthma, bronchiolitis) or focal (e.g., foreign body) intrathoracic airway obstruction, the normally passive process of expiration becomes active in an attempt to overcome airway resistance. Abdominal and internal intercostal muscles are recruited. Positive intrapleural pressure is generated, and increasing external pressure is applied to the airways. This leads to progressively increasing airway obstruction as expiration proceeds, a phenomenon referred to as dynamic airway compression (Figure 124-1).6
Dynamic airway compression results in prolonged expiratory time. The net result is failure of alveoli and distal airways to fully empty at end expiration, resulting in air trapping and increased functional residual capacity. Before subsequent inspiratory flow can begin, inspiratory muscles must overcome this increased elastic recoil, which substantially increases the work of breathing, a phenomenon referred to as auto–positive end-expiratory pressure. Finally, air trapping and subsequent atelectasis result in areas with ventilation–perfusion mismatch and hypoxemia.
Infants have smaller airways, highly compliant bronchial and bronchiolar cartilage, and more peripheral airway smooth muscle than older children and adults. These factors result in an even greater tendency toward airway collapse during expiration, air trapping, and auto–positive end-expiratory pressure. Thus, infants not only are more likely to experience wheezing illnesses, but are also more likely to suffer the physiologic consequences of airway obstruction.
WHEEZING
Approximately 25% to 30% of infants will have one episode of wheezing, and nearly 50% of children will have a history of wheezing by 6 years of age.2,7,8 Obtain a thorough history for any child with wheezing (Table 124-1). Consider age, family history, onset, pattern, seasonality, positional changes, and associated symptoms.2 Identify possible triggers. A recurrent and episodic pattern, history of cough, association with identifiable triggers, and documented response to bronchodilators are highly suggestive of asthma in a child >2 years old.9,10,11 A prior history of hospitalization, particularly to a critical care unit, and prior endotracheal intubation are important risk factors for severe disease. An exposure to sick contacts during a viral season, nasal congestion, poor feeding, and age <1 year suggest bronchiolitis.2 Choking or gagging indicates possible foreign body aspiration.
| Feature | Significance |
|---|---|
| Age | <1 y: bronchiolitis more common 1–2 y: mixed >2 y: asthma more common |
| Family history | Positive family history of wheeze suggests atopy, making asthma more likely |
| Pattern | Single episode: any etiology possible Recurrent: asthma Chronic illness: asthma, cystic fibrosis, congestive heart failure, anatomic abnormality |
| Onset | Sudden onset: foreign body aspiration, allergic reaction, asthma |
| Identifiable trigger | Concurrent viral illness: bronchiolitis, asthma Pollens, pets, dust, smoke and other irritants: asthma Choking episode: foreign body aspiration |
| Response to bronchodilators | Improvement with β2-agonist treatment is diagnostic for asthma Bronchiolitis may improve with inhaled epinephrine |
| Previous hospitalization | More severe disease, inability to care for child at home |
| Previous critical care unit admission ± intubation | More severe or life-threatening disease |
On physical examination, use the pediatric assessment triangle to assess appearance, work of breathing, and circulation.12 Assess the general appearance of the child using the TICLS mnemonic (tone, interactivity, consolability, look, and speech). Assess work of breathing by observing the child’s position (e.g., sniffing, tripod), accessory muscle use (e.g., nasal flaring, tracheal tug, scalene retraction, intercostal muscle use, abdominal breathing), and presence of stridor or wheeze. Assess circulation rapidly by observing the patient’s color, especially noting cyanosis. Determine respiratory rate (see Table 124-2 for age-related ranges).
Monitor oxygen saturation by either intermittent or continuous pulse oximetry. It is common for some infants and children with asthma or bronchiolitis to develop ventilation–perfusion mismatch, which may result in mild hypoxemia (92% to 94%) that is correctable with minimum supplemental oxygen (1 to 2 L/min). More severe hypoxemia (<91%) suggests moderate to severe disease. Hypoxemia refractory to bronchodilators and supplemental oxygen may suggest alternate diagnoses such as pneumonia, pneumothorax, pulmonary shunt, or congenital cardiac lesion (especially in the hypoxemic neonate). Diaphoresis, confusion, and drowsiness are ominous signs indicating imminent respiratory failure. Check for audibility and symmetry of breath sounds to assess adequacy of ventilation. Inspiratory-to-expiratory ratios of less than the normal 2:1 (e.g., 1:2 or 1:3) reflect the prolonged expiratory times seen with obstructive airway disease. Perhaps more important than the initial physical examination findings are the changes in these findings in response to bronchodilators and other treatments.
Table 124-3 lists the differential diagnosis of wheezing.
| Potential Diagnosis | Typical Age of Onset | Cardinal Symptoms and Signs | Confirmatory Tests |
|---|---|---|---|
| Asthma | >2 y | Recurrent episodes of wheeze and/or nighttime cough, identifiable triggers such as seasonality, allergens, exercise Responsive to bronchodilators | Trial of β-agonist Pulmonary function tests Allergy testing |
| Bronchiolitis | <2 y | URI symptoms, seasonal (winter months), nasal flaring and congestion, wheezes, rales, rhonchi | (Viral antigen testing) |
Gastroesophageal reflux Tracheoesophageal fistula | Present from birth | Cough, gagging, emesis related to feeding | Esophageal pH probe Barium swallow |
Vascular ring, sling, malformation, or airway hemangioma or polyp Laryngomalacia Tracheomalacia | Early infancy Present from birth, improves during first year of life | Stridor that changes with position of the neck, exacerbations with URI | CXR, CT angiography, bronchoscopy, barium swallow Laryngoscopy |
Congenital heart disease with left-to-right shunting and congestive failure Myocarditis | 2–6 mo Any age | Diffuse or basilar rales, tachycardia, hepatomegaly, cardiac murmur/gallop | CXR, ECG, echocardiography ECG, CXR, troponin, echocardiography |
Foreign body aspiration Vocal cord dysfunction (paradoxical vocal cord motion) | Usually >6 mo From birth (paralysis) Late school age/adolescents | History of choking episode with subsequent acute onset of stridor and/or wheezing. Stridor and/or wheezing, poor response to β-agonists | Right and left lateral decubitus CXRs* Flexible fiberoptic laryngoscopy |
| Epiglottitis | School age or adolescent | Stridor and high fever, toxic appearance, drooling and tripod positioning | Soft tissue radiographs of the neck* |
| Pneumonia | Any age | Fever, cough, tachypnea, rales, grunting | CXR |
Cystic fibrosis Ciliary dyskinesia Immunodeficiency | Present from birth | Recurrent lower respiratory tract infections, failure to thrive | Sweat chloride concentration Ciliary biopsy Immunoglobulin assays |
Asthma and bronchiolitis account for the majority of wheezing episodes in children, although a broader differential diagnosis must always be considered and ruled out on history, on physical exam, or with ancillary investigations. This is particularly important when the patient’s history or physical findings are not consistent with a diagnosis of asthma or bronchiolitis or when the illness does not respond to interventions appropriate to these disease processes. Table 124-3 outlines the signs, symptoms, context, and ancillary testing for the different causes of wheezing.
Stridor is not associated with lower airway obstruction and suggests an upper airway obstructive process (see chapter 123). The association of wheezing with feedings suggests gastroesophageal reflux or tracheoesophageal fistula with aspiration. Grunting, a physiologic response to generate positive end-expiratory pressure in an attempt to maintain alveolar inflation, suggests pneumonia, loss of surfactant, or other alveolar disease, although it may also result from extrapulmonary disease including GI emergencies. Inspiratory crackles or rales may result from atelectasis associated with bronchiolitis and asthma, although pneumonia should be considered, especially if these findings persist after initial bronchodilator therapy. Consider the possibility of foreign body aspiration and congestive heart failure because these disorders frequently cause wheezing.
BRONCHIOLITIS
Bronchiolitis is the most common lower respiratory tract infection in infants and children ≤2 years of age and is the leading cause for hospitalization in children <1 year of age.13 The most common cause is respiratory syncytial virus, although bronchiolitis may be caused by other viruses including, but not limited to, human metapneumovirus, adenovirus, influenza, rhinovirus, and parainfluenza viruses.14
The viral infection in bronchiolitis causes inflammation of the lower respiratory tract, with resultant edema, epithelial cell necrosis, bronchospasm, and increased mucus production within the bronchioles.15 These features result in variable degrees of air trapping, atelectasis, and hyperinflation of the lower airways. The increase in airway resistance and development of lower airway obstruction result in increased work of breathing. Because the nasal passages account for 50% of total airway resistance, increased nasal mucus production may cause upper airway obstruction due to the small nasal passages of infants. This in itself can cause modest respiratory distress, particularly in young infants, who are obligate nasal breathers.
Respiratory syncytial virus is transmitted by direct contact with contaminated secretions, including large droplets into the mucosa of the eyes and nose. Infected secretions found on fomites remain contagious for several hours. Because respiratory syncytial virus is highly infectious, self-contamination and nosocomial spread are common. Hand washing and contact precautions are important to limit the spread of disease. The incubation period for respiratory syncytial virus ranges from 2 to 8 days.
Although bronchiolitis can be seen throughout the year, its peak occurrence in North America is from November to March. Typical symptoms are rhinorrhea, tachypnea, wheezing, and coughing. Use of accessory muscles, nasal flaring, and fever may also occur. These symptoms last on average 7 to 21 days and are often the worst in the first week of the illness.16 The peak of symptoms is often between the third and fifth day after onset. Associated symptoms include irritability, cyanosis, and poor feeding.
A subset of infants with bronchiolitis will develop severe disease and apnea. Apneic episodes may be brief and self-limited or progress to more frequent and prolonged episodes that lead to hypoxia and the need for endotracheal intubation. Some infants presenting with apnea have minimal other symptoms. Several factors associated with a greater risk of severe disease and apnea are listed in Table 124-4.15,17 Infants with bronchiolitis and these risk factors may have prolonged hospital stays, greater need for mechanical ventilation, and higher mortality rates. Consider bronchiolitis in infants with apparent life-threatening events and monitor such infants closely (see chapter 115, “Sudden Infant Death Syndrome and Apparent Life-Threatening Event”).
On chest examination, wheezing and crackles are heard diffusely throughout both lung fields. Respiratory rates should be measured for 1 full minute and may vary from normal to profound tachypnea (Table 124-1). Accessory muscle use and intercostal or subcostal retractions develop as respiratory distress worsens. Patients with bronchiolitis are at risk for dehydration as blocked nasal passages inhibit feeding while increased work of breathing and a higher metabolic rate contribute to increased insensible losses. Assess for signs of dehydration including dry mucous membranes, tachycardia, lethargy, delayed capillary refill, inadequate urine output, and a sunken fontanelle.
Bronchiolitis is a clinical diagnosis based on the findings of the history and physical examination, which include typical symptoms of rhinorrhea, tachypnea, crackles, and/or wheezing in a child <2 years of age. There are several published scoring systems for assessing the severity of illness and change over time used for research purposes, although none has been validated or gained wide acceptance in clinical application. Obtain pulse oximetry readings at presentation to detect hypoxemia that may not be readily suspected on physical examination, and repeat readings during the course of the ED visit. Obtain intermittent oxygen saturation monitoring for children with mild disease and continuous monitoring for those with moderate or severe disease.
Rapid viral antigen detection tests may be useful. Sensitivity of the rapid tests generally ranges from 80% to 90% and specificity from 90% to 99%. Test results remain positive as long as virus is being shed. For respiratory syncytial virus, this may be up to 2 weeks after the onset of symptoms. The use of reverse transcriptase polymerase chain reaction testing to detect nucleic acid offers greater sensitivity. Results of viral culture are not available for several days and are not useful for guiding ED treatment.
Ancillary tests, such as blood work and radiographs, are not routinely needed unless other diagnoses need to be excluded.15 The incidence of serious bacterial infections in infants <28 days of age with bronchiolitis and fever is 3% to 10%, similar to that in other neonates with fever, so the standard testing of blood, urine, and cerebrospinal fluid is indicated. In infants >30 days of age, the incidence of serious bacterial infection in association with bronchiolitis remains 3% to 5%, with the most common infection being a urinary tract infection.18 Chest radiographs are not routinely indicated but may be considered when the illness is severe or associated with hypoxia, or when the course is atypical.19 Although the chest radiograph in bronchiolitis may demonstrate atelectasis, bacterial pneumonia is unusual.
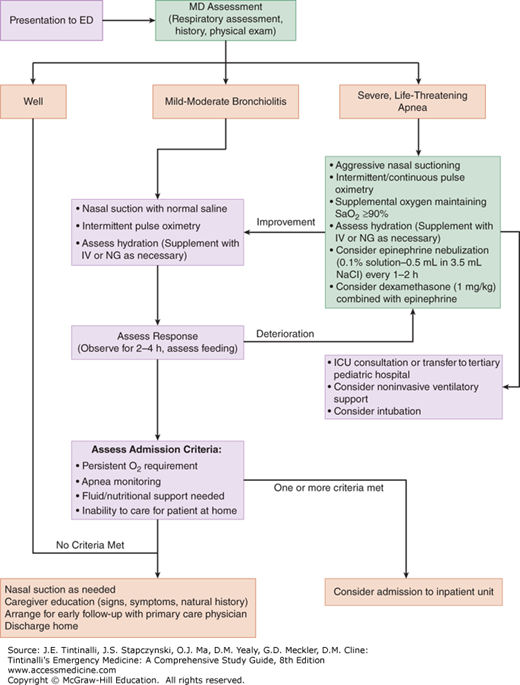
Figure 124-2 outlines an ED algorithm for bronchiolitis treatment based on severity of illness. In 2014, the American Academy of Pediatrics published an updated clinical practice guideline for the treatment of bronchiolitis in children age 1 to 23 months that highlights some of the challenges clinicians encounter in the inpatient and ED settings.15
Infants with bronchiolitis who do not meet criteria for admission can be managed as outpatients, and few need hospital admission. The most important treatment is frequent instillation of saline into the nares followed by suctioning. Support for feeding includes more frequent and smaller feeds and the use of prefeed suctioning. Caretakers should use frequent hand washing to minimize contagion.
No benefits have been shown on oxygen saturation, hospitalization rates, or duration of hospitalization by using β2-agonists (including salbutamol/albuterol, ipratropium bromide, and terbutaline),20,21 and they should not be given routinely. Inhaled epinephrine has not been shown to affect rates of admission from the ED or hospital length of stay among patients admitted for bronchiolitis; however, there may be a role in children with severe or acutely deteriorating bronchiolitis.15,21,22
The combined use of dexamethasone and epinephrine decreased admission rates in a large, multicenter, Canadian study that examined the effects of dexamethasone (1 milligram/kg) given in the ED with or without inhaled epinephrine followed by 5 days of dexamethasone (0.6 milligram/kg/d) at home.23 Infants in the dexamethasone-only and epinephrine-only groups did not show any benefits. Therefore, there is insufficient evidence to support stand-alone use of systemic or inhaled corticosteroids for bronchiolitis. Current guidelines advocate consideration for steroid use in combination with epinephrine in the treatment of bronchiolitis.24
The effect of hypertonic saline in bronchiolitis is mixed. Hypertonic saline may improve mucociliary clearance by loosening mucous plugs through osmotic draw of fluid from submucosal and adventitial spaces. The preponderance of evidence suggests no meaningful clinical benefit from nebulized hypertonic saline (3% or 7%) in the ED, and the 2014 American Academy of Pediatrics clinical practice guideline recommends against its routine use.15,25,26,27,28
The American Academy of Pediatrics recommends maintaining an oxygen saturation of >90%.15
Noninvasive ventilation measures, such as nasal continuous positive airway pressure and bilevel positive airway pressure, may help avoid or delay the need for endotracheal intubation and mechanical ventilation.29,30 However, when other measures do not work, endotracheal intubation with mechanical ventilation may be necessary.
Heliox does not affect the rates of intubation or mechanical ventilation or length of intensive care admission.31 There may be a small benefit on hospital length of stay by using heliox via tight-fitting facemask or nasal continuous positive airway pressure.32
The majority of children with bronchiolitis can be discharged from the ED. Educate caregivers regarding the signs and symptoms of increasing respiratory distress, including an increase in respiratory rate, presence of retractions, and inability to feed, and tell them to bring the child for immediate reevaluation if any of these develop. Demonstrate proper nasal suctioning techniques to caregivers. Counsel parents that symptoms may persist for up to 3 weeks to help avoid unnecessary ED returns for persistent mild symptoms.16
Factors that contribute to the need for admission include prematurity, corrected age <1 month old, persistent tachypnea or work of breathing despite therapy, dehydration, and oxygen requirement (arterial oxygen saturation [SaO2] <90% on room air). Admit infants with witnessed episodes of apnea and those with risk factors for apnea, even when they are clinically well appearing. Factors such as sex, race, duration of symptoms, parental history of asthma, and prior ED visits are not related to safety for discharge.33
More detailed information about bronchiolitis is provided in a practice guideline available at the American Academy of Pediatrics Web site ().
ASTHMA
Asthma is a chronic disease characterized by episodic and reversible airflow obstruction due to bronchial smooth muscle hyperreactivity and inflammation, that is responsive to bronchodilator and corticosteroid treatments.9,10,34
More than 95% of children age 2 to 18 years presenting to the ED with asthma exacerbations exhibit wheezing, shortness of breath, cough, and/or dyspnea secondary to decreased expiratory airflow.35 Milder cases of acute asthma exacerbations may present with only wheezing or mild dyspnea, whereas severe exacerbations present with dyspnea at rest, inability to speak, and marked increased work of breathing and may be associated with peak expiratory flow of <40% of predicted value.10 Severe exacerbations may progress to status asthmaticus and respiratory failure, which may be life-threatening.36,37
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree