WHEEZING
DANICA B. LIBERMAN, MD, MPH AND VINCENT J. WANG, MD, MHA
Wheezes are whistling or musical adventitious sounds that are the hallmark of lower airway constriction and/or obstruction. Whereas rales or crackles are discontinuous or intermittent popping noises, wheezes are continuous sounds most frequently heard during expiration. The most common diseases causing wheezing in children are bronchiolitis and asthma, but the differential diagnosis is broad, and the causes are multifactorial. An episode of wheezing may occur at least once in 20% of infants younger than 1 year of age, and in almost 50% of children younger than 6 years of age, but fewer than 15% of children will develop asthma. This chapter presents an organized approach to the diagnosis of conditions associated with wheezing in children beyond the newborn period.
PATHOPHYSIOLOGY
Obstruction to air flow is the common denominator in all conditions that produce wheezing. Wheezing usually results from obstruction of the intrathoracic lower airways (bronchioles) and less commonly by narrowing of the trachea or bronchi. Obstruction of the lower airway passages may be anatomic or physiologic and is the result of intrinsic airway narrowing or extrinsic airway compression. Intrinsic airway narrowing may be caused by bronchial or bronchiolar constriction, inflammation, and/or intraluminal airway blockage. It may also be caused by a combination of these factors simultaneously, as in asthma. When wheezing is audible during the inspiration and expiration phases of respiration, wheezing is more likely to be caused by extrinsic airway compression. In contrast, when wheezing is predominantly expiratory, intrinsic airway narrowing is more likely to be the cause.
DIFFERENTIAL DIAGNOSIS
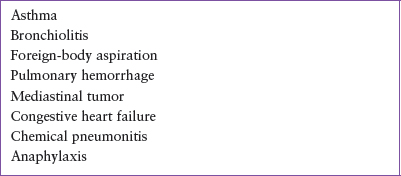
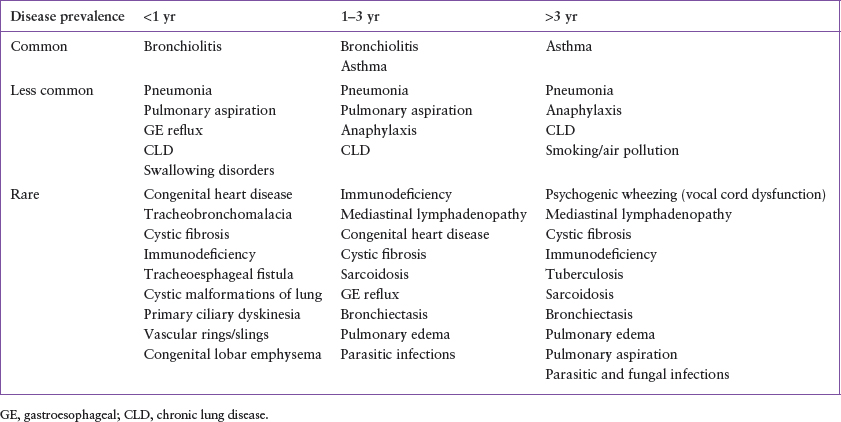
Table 80.1 lists the life-threatening causes of wheezing, and Table 80.2 outlines the relative prevalence of conditions that may present acutely with wheezing, categorized by age.
Common Conditions
Bronchiolitis is an acute viral infection of the lower respiratory tract caused predominantly by respiratory syncytial virus (RSV). Other causes include rhinovirus, parainfluenza virus, adenovirus, influenza virus, coronavirus, and human metapneumovirus. Occurring primarily in epidemics between November and April, bronchiolitis affects children younger than 2 years of age. Proliferation of cells and submucosal edema lead to obstruction of the bronchioles. Rhinorrhea and a low-grade fever typically accompany a prominent staccato-like cough and a variable degree of respiratory distress. The concurrence of respiratory symptoms in other family members is common. Degree of severity is multifactorial, with factors such as parental smoking, prematurity, congenital heart disease, and reactive airway disease contributing to the individual patient’s response to the viral infection.
Asthma is a chronic inflammatory disorder of the airways, characterized clinically by recurrent exacerbations involving symptoms of coughing and/or wheezing. Acute asthma attacks are usually triggered by respiratory infections, allergens, exercise, and irritants, such as cigarette smoke or particulate air pollution. Patients with asthma have a higher incidence of associated atopic diseases, which include allergic rhinitis and conjunctivitis, and atopic dermatitis. Immediate family members are also more likely to be affected by asthma and atopic disease. Although many hesitate to make the diagnosis of asthma in a child younger than 2 years of age, many asthmatics have their first episode of wheezing before this age. However, 60% of those who wheeze before 3 years of age will not wheeze by school age. In addition, it is unknown if bronchiolitis predisposes patients to develop asthma, or if the response to bronchiolitis is different for a patient who is predisposed to developing asthma.
Less Common Conditions
Other infectious causes of wheezing include viral or bacterial pneumonia. Most cases are preceded by several days of upper respiratory tract symptoms and fever. Physical examination will usually reveal tachypnea, retractions, rales, and/or wheezes. Auscultatory findings are often localized rather than diffuse. As with bronchiolitis, the most common causes of pneumonia are viral. Bacterial causes include Streptococcus pneumoniae, Mycoplasma pneumoniae, Chlamydia pneumoniae, group A Streptococcus, and Staphylococcus aureus. S. pneumoniae has been the most common bacterial agent, but the incidence has decreased since the widespread utilization of the conjugate pneumococcal vaccine.
Pulmonary aspiration is a less common cause of wheezing that occurs in several fairly characteristic clinical circumstances. In otherwise healthy children, the abrupt onset of respiratory distress, associated with an episode of coughing, choking, or gagging, suggests the pulmonary aspiration of a foreign object (see Chapter 27 Foreign Body: Ingestion and Aspiration). Foreign-body aspiration is typically seen in toddlers, although older infants may aspirate solid food particles or small objects placed within their reach. Rarely, an older child may also aspirate food particles or other objects. The aspiration of a small object or food substance may not be witnessed, and thus, may go unrecognized for weeks or months until persistent lower respiratory symptoms trigger a search for an underlying cause. In these circumstances, persistent cough, wheezing, and sometimes recurrent fever is associated with an area of consolidation and/or collapse on radiograph. These symptoms fail to resolve despite seemingly appropriate medical therapy.
TABLE 80.1
LIFE-THREATENING CAUSES OF WHEEZING
Recurrent aspiration of food or gastric contents is usually seen in infants younger than 1 year of age, or in older patients with severe intellectual disability or neuromuscular disease. Disordered swallowing and gastroesophageal (GE) reflux typically contribute in varying degrees to the recurrent aspiration that occurs in these patients. Repeated aspiration is also seen in children with tracheostomies and in children with structural anomalies of the tracheolaryngeal complex or an H-type tracheoesophageal fistula, which are rare. Patients with chronic recurrent aspiration may develop wheezing and respiratory distress in the absence of a well-defined episode of choking or severe coughing because many such patients have depressed cough reflexes or experience “microaspiration.” Fever often accompanies pulmonary aspiration, reflecting associated chemical inflammation or infection of the tracheobronchial tree.
Wheezing attributable to anaphylaxis is also of sudden onset and may be accompanied by one or more other clinical findings that include urticaria, angioedema, stridor, hypotension, abdominal pain, vomiting, and diarrhea. When wheezing is the only finding, anaphylaxis may be suspected when the onset of respiratory difficulty is associated with Hymenoptera envenomation, medication or food ingestion, or another allergic precipitant. Wheezing in this context typically responds promptly to epinephrine administration and/or to bronchodilator therapy.
The development of chronic respiratory problems in the neonatal period, due to complications such as prematurity, assisted ventilator support, and oxygen dependence, all lead to a common condition referred to as chronic lung disease (CLD). This condition is the childhood equivalent of chronic obstructive pulmonary disease and represents a pathophysiologic continuum that includes varying degrees of structural damage and airway inflammation. Although gradual improvement in lung function occurs during infancy and early childhood, bronchial hyperactivity and recurrent episodes of wheezing may persist until later in childhood.
Transient wheezing may also occur with smoking and air pollutant exposures. It is important to note, that 90% of cigarette smokers start before the age of 21 years. Wheezing and bronchiolitis have also been associated with passive smoke exposure. Air pollution containing particulate matter less than or equal to 10 microns in diameter, which is small enough to travel into the distal airways, nitrogen dioxide, nitrogen oxide, and carbon monoxide have been associated with wheezing, and can exacerbate other causes of wheezing.
Rare Conditions
Cardiovascular abnormalities are one of many uncommon causes of wheezing in children. Small airway edema in the setting of congestive heart failure or airway impingement by enlarged cardiovascular structures is the usual pathophysiologic mechanism. Most cardiac conditions are associated with other abnormal physical findings, including cyanosis, murmurs, abnormal pulses, poor perfusion, or signs consistent with congestive heart failure. Though abnormal cardiac physical findings are generally absent in patients with a vascular ring or sling, these structural abnormalities may cause wheezing and dysphagia due to esophageal compression; and a right-sided aortic arch is often noted on chest radiograph.
TABLE 80.2
CLINICAL CLASSIFICATION OF WHEEZING: AGE AT DIAGNOSIS AND DISEASE PREVALENCE
While pulmonary disease, including wheezing, is the hallmark of cystic fibrosis (CF), individuals with CF (see Chapter 107 Pulmonary Emergencies) will often also exhibit steatorrhea and failure to thrive because of pancreatic insufficiency and malabsorption. Similar to CF, patients with primary ciliary dyskinesia also develop repeated respiratory tract infections, sinusitis, and otitis media, often in association with situs inversus viscerum and bronchiectasis (Kartagener’s syndrome).
Wheezing may result from pulmonary edema, which may be caused by congenital or acquired heart disease with congestive heart failure. However, pulmonary edema may also be caused by other disease processes, such as pneumonia, acute respiratory distress syndrome, and hypoalbuminemic states, such as nephrotic syndrome and liver failure. Hydrocarbon aspiration, leading to a chemical pneumonitis, may also cause pulmonary edema.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







