INTRODUCTION AND EPIDEMIOLOGY
Dizziness is a common complaint in patients >40 years old, leading to roughly 10 million visits to ambulatory care settings and 25% of ED visits.1 Dizziness can lead to falls in elderly patients. The symptoms may persist and be incapacitating. Patients may use various terms for the complaint: dizziness may mean vertigo, syncope, presyncope, weakness, giddiness, anxiety, or a disturbance in mentation.
Vertigo is the perception of movement (rotational or otherwise) where no movement exists. Syncope is a transient loss of consciousness accompanied by loss of postural tone with spontaneous recovery. Near-syncope is light-headedness with concern for an impending loss of consciousness. Psychiatric dizziness is defined as a sensation of dizziness not related to vestibular dysfunction that occurs exclusively in combination with other symptoms as part of a recognized psychiatric symptom cluster.2 Disequilibrium refers to a feeling of unsteadiness, imbalance, or a sensation of “floating” while walking.
Acute vestibular syndrome is a symptom complex consisting of vertigo, nausea and vomiting, intolerance to head motion, spontaneous nystagmus, unsteady gait, and postural instability caused by injury to peripheral or central vestibular structures. To be called acute vestibular syndrome, the associated vertigo must persist for at least 24 hours, thus excluding causes of transient vertigo such as benign paroxysmal positional vertigo (BPPV). Acute vestibular syndrome may be peripheral or central in origin. Clinical findings that distinguish central from peripheral causes include focal neurologic deficits such as hemiparesis, hemisensory loss, or gaze palsy. The most common peripheral cause of acute vestibular syndrome is vestibular neuronitis. The most common central cause is ischemic stroke of the posterior fossa (brainstem or cerebellar), followed by demyelination. There is growing evidence that a significant number of patients with central acute vestibular syndrome are misdiagnosed in the ED. A systematic review estimated that roughly 25% of patients presenting with acute vestibular syndrome have had a stroke.3
The time-honored paradigm of evaluating dizziness is based largely on the patient’s subjective description. More recently, objective bedside physical examination has emerged as a more reliable way of arriving at the correct diagnosis.4
PATHOPHYSIOLOGY
The CNS coordinates and integrates sensory input from the visual, vestibular, and proprioceptive systems. Vertigo arises from a mismatch of information from two or more of the involved senses, caused by dysfunction in the sensory organ or its corresponding pathway.
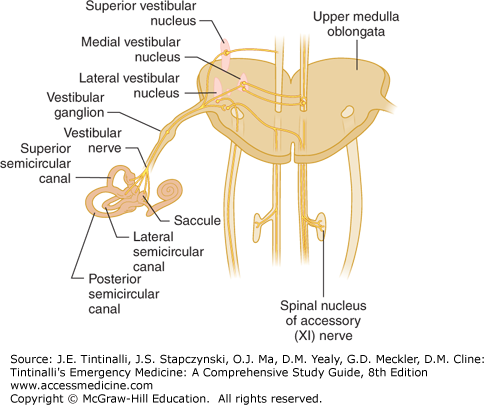
Visual inputs provide spatial orientation. Proprioceptors help relate body movements and indicate the position of the head relative to that of the body. The vestibular system (via the otoliths) establishes the body’s orientation with respect to gravity. The cupulae’s sensors track rotary motion. The three semicircular canals sense orientation to movement and head tilts and are filled with a fluid called endolymph. The endolymphatic sac produces glycoproteins that create an osmotic sink necessary to maintain flow. The movement of fluid in the semicircular canals causes specialized hair cells inside the canals to move, causing afferent vestibular impulses to fire. Sensory input from the vestibular apparatus travels to the nucleus of the eighth cranial nerve (Figure 170-1).
The medial longitudinal fasciculus, the red nuclei, the cerebellum, the parietal lobes, and the superior temporal gyrus of the cerebral cortex integrate the various sensory inputs. Connections between these structures and the oculomotor nuclei that drive the vestibulo-ocular reflex complete the system. The vestibulo-ocular reflex prevents visual blurring from head movements and body sway.
Balanced input from the vestibular apparatus on both sides is the norm. Unilateral lesions of the vestibular apparatus as well as excessive unilateral firing due to abnormal motion of the endolymph produce imbalanced activity and vertigo. Rapid head movements accentuate the imbalance. Symmetric bilateral damage does not usually produce vertigo but may lead to truncal or gait instability.
The most striking clinical sign associated with vertigo is nystagmus, a rhythmic movement of the eyes that has both a fast and a slow component, with direction named by its fast component. The slow component is due to the vestibulo-ocular reflex and is generated by excitation of the semicircular canal, producing eye movement away from that canal. The fast component of nystagmus is caused by the cortex, which exerts a quick corrective movement in the opposite direction. Vestibular disorders produce nystagmus that is provoked when the affected side is in the dependent position, and the characteristic pattern is vertical and rotational or horizontal. Vertical nystagmus by itself usually indicates a brainstem abnormality. However, an atypical pattern of nystagmus in the absence of other signs of CNS disease does not necessarily indicate central pathology.5
The prevalence of dizziness increases with age and is due to decreases in visual acuity, proprioception, and vestibular input, plus an increase in free-floating otoconia within the semicircular canals that cause BPPV. Older patients are also more likely to take medications that cause dizziness.
Physiologic vertigo results from a mismatch of visual, proprioceptive, and vestibular input. This may be the pathogenesis of motion sickness as well as the transient visual vertigo associated with watching a film that captures the visual sensation of motion, by attending complex visual environments, such as shopping malls, and by viewing complex floor or wallpaper patterns.
CLINICAL FEATURES
The conditions that cause acute undifferentiated vertigo are summarized in Table 170-1. Vertigo is usually categorized as “peripheral” or “central,” and making the distinction between the two is the most important part of the evaluation. Peripheral vertigo is caused by disorders affecting the vestibular apparatus and the eighth cranial nerve, whereas central vertigo is caused by disorders affecting central structures, such as the brainstem and the cerebellum. Peripheral vertigo tends to cause distressing symptoms, but is seldom life threatening; the reverse tends to be true for central vertigo. Disorders causing central vertigo often require urgent diagnostic imaging or consultation with a neurologist or neurosurgeon.
| Vestibular/otologic | Benign paroxysmal positional vertigo Traumatic: following head injury Infection: labyrinthitis, vestibular neuronitis, Ramsay Hunt syndrome |
| Systemic conditions with vestibular/otologic effects | Ménière’s syndrome Neoplastic Vascular Otosclerosis Paget’s disease Toxic or drug-induced: aminoglycosides |
| Neurologic | Vertebrobasilar insufficiency or vertebral artery dissection Lateral Wallenberg’s syndrome Anterior inferior cerebellar artery syndrome Neoplastic: cerebellopontine angle tumors Cerebellar disorders: hemorrhage, degeneration Basal ganglion diseases Multiple sclerosis Infections: neurosyphilis, tuberculosis Epilepsy Migraine headaches Cerebrovascular disease |
| General | Hematologic: anemia, polycythemia, hyperviscosity syndrome Toxic: alcohol Chronic renal failure Metabolic: thyroid disease, hypoglycemia |
Some of the features that distinguish peripheral causes from central causes (mainly cerebrovascular disease) are found in Table 170-2. Note that many of the so-called distinguishing features of peripheral acute vestibular syndrome may also be found in some patients with cerebrovascular disease.6
| Peripheral | Central | |
|---|---|---|
| Onset | Sudden or insidious | Sudden |
| Severity of vertigo | Intense spinning | Ill defined, less intense |
| Prodromal dizziness | Occurs in up to 25%; often single episode | Occurs in up to 25%; recurrent episodes suggest transient ischemic attacks |
| Intolerant of head movements/Dix-Hallpike maneuver | Yes | Sometimes |
| Associated nausea/diaphoresis | Frequent | Variable |
| Auditory symptoms | Points to peripheral causes | May be present |
| Proportionality of symptoms | Usually proportional | Often disproportionate |
| Headache or neck pain | Unusual | More likely |
| Nystagmus | Rotatory-vertical, horizontal | Vertical |
| CNS symptoms/signs | Absent | Usually present |
| Head impulse test | Abnormal | Usually normal |
| HINTS examination (combined horizontal head impulse test, nystagmus, and test of skew) | Normal on all three bedside tests | Abnormal on at least one of three bedside tests |
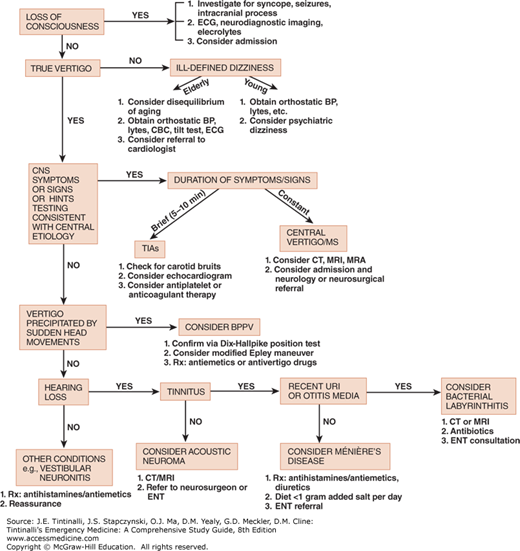
An approach to vertigo is shown in Figure 170-2. Try to obtain an unprompted description of the patient’s “dizziness” and avoid leading questions that bias the patient’s responses. However, the initial description may not be a reliable predictor of underlying pathology.7
FIGURE 170-2.
Guideline approach to vertigo. BP = blood pressure; BPPV = benign paroxysmal positional vertigo; CBC = complete blood count; CNS = central nervous system; ENT = ear, nose, and throat; MRA = magnetic resonance angiography; MS = multiple sclerosis; Rx = treatment; TIAs = transient ischemic attacks; URI = upper respiratory infection.
Patients with acute vestibular syndrome have continuous vertigo or dizziness for more than 24 hours. Thus, the list excludes causes of brief transient episodes such as BPPV, Ménière’s syndrome, and transient ischemic attack. If the patient has experienced true vertigo, determine whether the vertigo is of peripheral or central origin, and determine the temporal pattern and precipitating causes (Table 170-3). Peripheral vertigo is more likely than central vertigo to be intense and to be associated with nausea, vomiting, diaphoresis, tinnitus, hearing loss, and photophobia.
Headache is generally not a feature of peripheral causes of acute vestibular syndrome but is associated with central causes. Dizziness and headache suggest migraine but also occur with vertebral artery dissection or aneurysm.8
Head trauma and medications can precipitate episodes of dizziness or interfere with central adaptation. Recent head or neck trauma is a risk factor for dissection of the vertebral artery. In patients with acute vertigo, a recent history of trauma should spark concern for dissection even if pain is absent.
Evaluate the following groups for central vertigo: older patients, those with hypertension or cardiovascular disease, those with other risk factors for stroke, or those taking warfarin. Patients with acute vestibular syndrome and more than one vascular risk factor appear to be at increased risk of stroke. Although age is a known risk factor for stroke, patients age 50 and older with symptoms of acute vertigo and no neurologic signs are more likely to have vestibular neuronitis than stroke.9 However, age per se does not rule out stroke as the cause of central acute vestibular syndrome. In a study of patients with cerebellar infarctions who were misdiagnosed on initial ED presentation, half of the patients misdiagnosed were younger then 50 years of age who presented with headache and vertigo. All of the patients misdiagnosed had either an incomplete or a poorly documented neurologic examination. Almost all of the patients had a CT scan of the brain that was initially interpreted as normal. The overall mortality was 40%; among survivors, 50% had disabling neurologic sequelae. This study underscores the need for a careful neurologic assessment in all such patients.10
Perform complete ear, neurologic, and vestibular examinations in patients presenting with vertigo or dizziness. Examine the external auditory canal and tympanic membrane for evidence of otitis media, cholesteatoma, and other pathology. Test for hearing, and also perform Webber and Rinne testing. Hearing loss usually points to peripheral causes such as vestibular neuronitis and Ménière’s syndrome. However, auditory symptoms and signs may also be due to ischemia of the inner ear associated with cerebrovascular disease.
When assessing patients with acute vestibular syndrome, keep the possibility of cerebrovascular disease in mind. The presence of focal neurologic deficits indicates a central etiology. However, focal deficits are not uniformly present in central vertigo. A systematic review found focal neurologic deficits in 80% of patients with acute vestibular syndrome caused by stroke.3 In the HINTS study, neurologic (e.g., facial palsy, hemiparesis, limb ataxia) or oculomotor (e.g., internuclear ophthalmoplegia, gaze palsy, vertical nystagmus) abnormalities were reported in 51% of 76 patients with a central cause and none of 25 patients with a peripheral cause.8 The presence of gait unsteadiness and severe truncal ataxia (inability to sit unaided with arms crossed) suggests vertigo due to stroke. A positive Romberg test is rarely found in patients with peripheral vertigo. The absence of focal neurologic deficits in some patients with central acute vestibular syndrome has led to growing interest in other methods of bedside testing.
HINTS testing is an important advance in the rapid assessment of ED patients with acute vestibular syndrome. HINTS is an acronym that stands for horizontal head impulse test, nystagmus, and test of skew—three bedside tests that when taken together reliably help distinguish central (usually stroke) from peripheral acute vestibular syndrome.
The horizontal head impulse test is also known as the Halmagyi head thrust and, by itself, is the most helpful bedside test for distinguishing central from peripheral vertigo. The Halmagyi head thrust assesses the vestibulo-ocular reflex. Ask the patient to fixate on a visual target, while the examiner rotates the patient’s head rapidly first from the center position to 40 degrees left and back again to the center position. Repeat the test on the right side. Carefully watch the patient’s eyes for the response to the maneuver. The intact vestibulo-ocular reflex compensates for the rotational head thrust by rapidly and smoothly moving the eyes in the direction opposite to the head thrust. This is the normal physiologic response to a passive head thrust; an intact vestibulo-ocular reflex maintains fixation of the eyes with respect to the patient’s environment. Thus, the patient will be able to maintain his or her gaze on the visual target throughout the head thrust.
If the vestibulo-ocular reflex is impaired, then the patient will not be able to maintain his or her gaze on the visual target, and the patient will exhibit a rapid simultaneous movement of both eyes (known as a saccade) in order to reacquire fixation upon the visual target. This is an abnormal response to the horizontal head impulse test.11
Thus, in a patient with no symptoms or signs of acute vestibular syndrome, a normal horizontal head impulse test (i.e., no corrective saccade) means that the vestibulo-ocular reflex is normal. In a patient with acute vestibular syndrome, an abnormal response horizontal head impulse test (i.e., a corrective saccade) usually indicates a peripheral vestibular lesion, while no corrective saccade is highly suspicious for a stroke.12 In the HINTS study, the head impulse test had both a sensitivity and specificity comparable to that of MRI.8
The second part of HINTS testing that helps predict central acute vestibular syndrome is direction-changing horizontal nystagmus on lateral gaze. An abnormal response, which consists of right-beating nystagmus on right gaze and left-beating nystagmus on left gaze with or without nystagmus when the patient looks straight ahead, is believed to represent failure of gaze-maintaining structures located in the brainstem and the cerebellum. Direction-changing nystagmus has low sensitivity but high specificity for correctly identifying central causes of acute vestibular syndrome. The third part of HINTS testing is known as skew deviation or skew and refers to vertical ocular misalignment during the alternate cover test. Skew deviation only occurs in the presence of right-left imbalance in sensory inputs from the vestibular system to the oculomotor syndrome. As with direction-changing nystagmus, skew deviation is not sensitive but is highly specific for central acute vestibular syndrome.
All three bedside tests (horizontal head impulse test, nystagmus, and skew) have been combined into the HINTS battery of tests that define a clinical prediction rule for stroke. Just one finding specific for central acute vestibular syndrome on any of the three tests that make up the HINTS battery is considered 100% sensitive and 96% specific for stroke.8 A cross-sectional study of patients with acute vestibular syndrome at high risk for stroke found that HINTS testing substantially outperformed ABCD2 risk scoring for stroke diagnosis in the ED and also outperformed MRI obtained within the first 2 days of symptom onset.13 A current review concluded that with appropriate training in the technique, it is reasonable to use HINTS testing as a tool to distinguish central from peripheral vertigo.14
The diagnosis of BPPV involving the posterior canal is aided by the Dix-Hallpike position test. Do not perform this test on patients with carotid bruits, a history of prior cerebrovascular disease, or risk factors or concern for vertebrobasilar insufficiency, because the Dix-Hallpike maneuver carries a theoretical risk of precipitating a stroke. In addition, use caution in patients with spinal injury or cervical spondylosis. The test may provoke vertigo. Pretreatment with 50 milligrams of dimenhydrinate IM or IV may make the test more tolerable but will not obliterate nystagmus. Have patients keep their eyes open at all times and stare at the examiner’s nose or forehead. Start with the patient seated upright on the examining table. To test the right posterior semicircular canal, rotate the head 30 to 45 degrees to the right. Keeping the head in this position, rapidly bring the patient supine until the head is 20 degrees below the level of the examining table. Rotatory nystagmus following a latency of no more than 30 seconds is considered a positive test; the nystagmus exhibits rapid eye torsions toward the affected ear and lasts for 10 to 40 seconds. Return the patient to the upright sitting position, and repeat the test on the left side. The side exhibiting the positive test is the side of the lesion.15