Chapter 83 Vasodilators and antihypertensives
Vasodilators are a generic group of drugs that are primarily used in the intensive care unit (ICU) for the management of acute hypertensive states and emergencies. In addition, they have an important role in the management of hypertension and cardiac failure.1
PHYSIOLOGY
Blood pressure is controlled by a complex physiological neurohormonal system involving all components of the cardiovascular system.2,3 Traditionally, clinical practice has focused on the arterial circulation as the major regulator of systemic pressure. The importance of venous circulation in determining mean arterial pressure and cardiac output is discussed in Chapter 82.
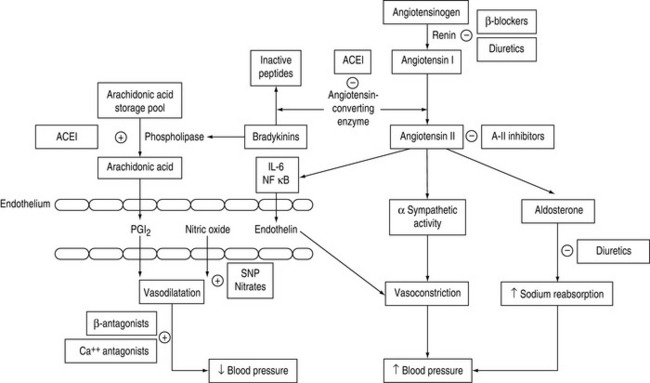
The role of the peripheral vasculature, including both arteriolar and venous systems, in the regulation of blood pressure may be conceptually regarded as a balance between vasodilatation and vasoconstriction3 (Figure 83.1).
CALCIUM FLUX
The concentration of intracellular ionised calcium is the primary determinant of vascular smooth muscle tone: increases lead to smooth muscle contraction, decreases cause relaxation. Control of calcium influx and efflux is determined by adrenergic receptor occupation and changes in membrane potential, mediated through voltage gated channels (see Chapter 82, Figure 82.2).
ENDOTHELIAL SYSTEM
The endothelium has a central role in blood pressure homeostasis by secreting substances such as nitric oxide, prostacyclin and endothelin.3 These substances are continuously released by the endothelium and are integral in regional autoregulation.4
ADRENERGIC SYSTEM
The sympathetic nervous system is integrally involved with all of the above systems, regulating vascular tone at central, ganglionic and local neural levels. Adrenergic stimulation of β-receptors is associated with vasodilatation; α-receptor stimulation results in vasoconstriction. The vascular effects of the catecholamines and vasopressors are discussed in Chapter 82.
Adrenergic stimulation is the predominant system in regulating venous tone.5 This is due to endothelial differences in veins resulting in less production of nitric oxide and reduced responsiveness to angiotensin II.
PATHOPHYSIOLOGY
Hypertensive states develop as a result of impaired or abnormal homeostatic processes, causing an imbalance between vasoconstrictive and vasodilatory effects.
CALCIUM ANTAGONISTS
Calcium antagonists have numerous effects on the cardiovascular system, influencing heart rate conduction, myocardial contractility and vasomotor tone. Entry of calcium through voltage-gated calcium channels is a major determinant of arteriolar, but not venous, tone.6
Magnesium is a physiological calcium antagonist, and is used therapeutically as magnesium sulphate.
NIFEDIPINE
Nifedipine is frequently used to treat angina pectoris, especially that due to coronary artery vasospasm. Peripheral vasodilatation results in decreased systemic blood pressure, often associated with sympathetic stimulation resulting in increased cardiac output and heart rate that may counter the negative inotropic, chronotropic and dromotropic effects of nifedipine. Nevertheless, nifedipine may be associated with profound hypotension in patients with ventricular dysfunction, aortic stenosis and/or concomitant β-blockade. For this reason, the use of sublingual nifedipine as a method of treating hypertensive emergencies is no longer recommended.7
Nifedipine and related drugs may cause diuretic-resistant peripheral oedema that is due to redistribution of extracellular fluid rather than sodium and water retention.
NIMODIPINE
It may be used to attenuate cerebral arterial vasospasm following aneurysmal subarachnoid haemorrhage. Improved outcomes have been demonstrated in patients with Grade 1 and 2 subarachnoid haemorrhage.8 Systemic hypotension may result from peripheral vasodilatation that may compromise cerebral blood flow in susceptible patients. Similarly, cerebral vasodilatation may increase intracranial pressure in patients with reduced intracranial elastance.
It may be given by intravenous infusion or enterally with equal effect.
AMLODOPINE
Amlodipine is an oral preparation that has a similar pharmacodynamic profile to nifedipine. In addition to arteriolar vasodilatory and cardiac effects, amlodipine has been shown to exert specific anti-inflammatory effects in hypertension, diabetic nephropathy and in modulating high-density lipoprotein (HDL) in patients with hypercholesterolaemia.9 These effects have seen amlodipine increasingly being used for treatment of hypertension in high-risk patients, and may have a role in stable critically ill patients with associated comorbidities.
VERAPAMIL
Verapamil is not as active as nifedipine in its effects on smooth muscle and therefore causes less pronounced decrease in systemic blood pressure and reflex sympathetic activity. It has a limited role as a vasodilator.10
MAGNESIUM SULPHATE
Magnesium regulates intracellular calcium and potassium levels by activation of membrane pumps and competition with calcium for transmembrane channels. Physiological effects are widespread, affecting cardiovascular, central and peripheral nervous systems and the musculoskeletal junction.11
Consequently, it has an established role in the treatment of pre-eclampsia and eclampsia,12 perioperative management of phaeochromocytoma13 and treatment of autonomic dysfunction in tetanus.14
DIRECT-ACTING VASODILATORS
These drugs act directly on vascular smooth muscle and exert their effects predominantly by increasing the concentration of endothelial nitric oxide. These drugs are also known as nitrovasodilators.15
SODIUM NITROPRUSSIDE
Sodium nitroprusside produces direct venous and arterial vasodilatation, resulting in a prompt decrease in systemic blood pressure. The effect on cardiac output is variable. Decreases in right atrial pressure reflect pooling of blood in the venous system, which may decrease cardiac output. This may result in reflex tachycardia that may oppose the overall reduction in blood pressure. In patients with left ventricular failure, the effect on cardiac output will depend on initial left ventricular end-diastolic pressure. Sodium nitroprusside has unpredictable effects on calculated systemic vascular resistance. Homeostaticmechanisms in preserving cardiac output may explain tachyphylaxis to prolonged infusions.
The prolonged use of large doses of sodium nitroprusside may be associated with toxicity related to the production and cyanide and, to a lesser extent, methaemoglobin.16
ISOSORBIDE DINITRATE
Isosorbide dinitrate is the most commonly administered oral nitrate for the prophylaxis of angina pectoris. It has a physiological effect that lasts up to 6 hours in doses of 60–120 mg. The mechanism of action is the same as glyceryl trinitrate. Hypotension may follow acute administration, but tolerance to this develops with chronic therapy.17
HYDRALAZINE
Following intravenous administration, hydralazine has a rapid onset of action, usually within 5–10 minutes. It may also be administered intramuscularly or orally. The drug is partially metabolised by acetylation, for which there is marked inter-individual variability (35% population are slow acetylators). Whilst this does not have much clinical significance regarding the antihypertensive effects, it is important with respect to toxicity.17
DIAZOXIDE
Diazoxide is chemically related to the thiazide diuretics and is a potent, non-selective, direct-acting vasodilator. The mechanism of action is unclear, but it is a predominantly arteriolar vasodilator.18 Diazoxide is administered intravenously or intramuscularly. It has a rapid onset (3–5 minutes) and prolonged duration of action (1–2 hours), often with precipitous reductions in blood pressure. Diazoxide has similar cardiovascular effects to hydralazine and is associated with significant reflex sympathetic stimulation, resulting in increased cardiac output and heart rate.
It is associated with metabolic side-effects such as hyperglycaemia and sodium and water retention.
α-ADRENERGIC ANTAGONISTS
Several groups of compounds act as α-adrenergic blockers with variable affinity for populations of α-receptors. Physiology and pathophysiology may influence the responsiveness of the drug receptor–effector relationship. Receptor pathobiology is discussed in Chapter 82. Consequently, there may be marked inter- and intra-individual variability in the patient’s response to these drugs.
PHENTOLAMINE
Phentolamine is a non-selective, competitive antagonist at α1– and α2-receptors. At low doses, phentolamine causes prejunctional inhibition of noradrenaline release (via α2-receptor inhibition). At higher doses, more complete α-receptor blockade is achieved, with enhancement of effects of β-agonists due to increased local concentration of noradrenaline produced by α2-blockade (see Chapter 82, Figure 82.3a).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree