CHAPTER 41
Vascular Complications of Spinal Interventions
INTRODUCTION
Minimally invasive procedures/injections are used to diagnose and treat pain emanating from intervertebral joints, spinal nerves, nerve roots, spinal cord, and sympathetic ganglia. These procedures are performed in the lumbosacral, thoracic, and cervical spinal canal. Vascular complications can and do occur in all areas of the spine and are of grave concern to all practitioners secondary to their irreversibility (Figures 41-1 and 41-17).

Figure 41-1. Spinal cord infarction following left L3-4 transforaminal ESI. (Reproduced with permission from Murthy, et al. Mayo Clinic Department of Radiology.)
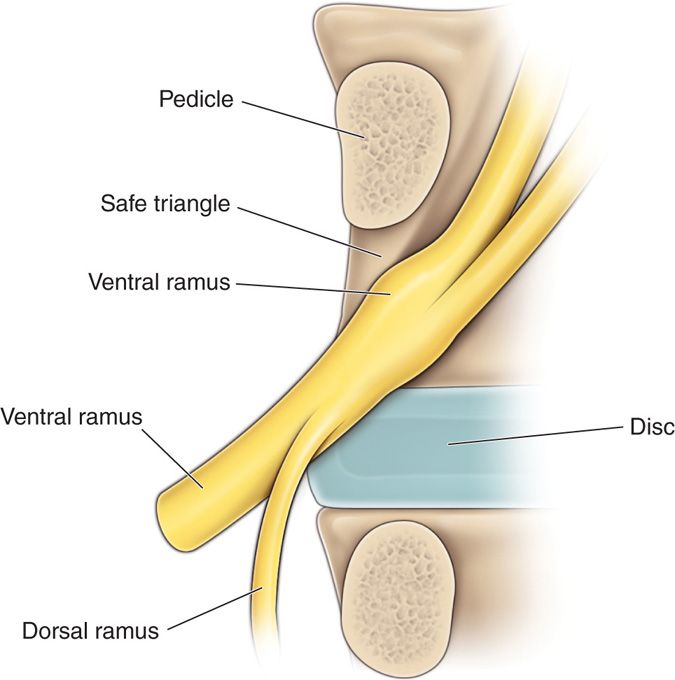
Figure 41-2. Original description of “safe triangle” in the anterior and superior aspect of foramen on an A-P view. Note lack of description of vascular contents.
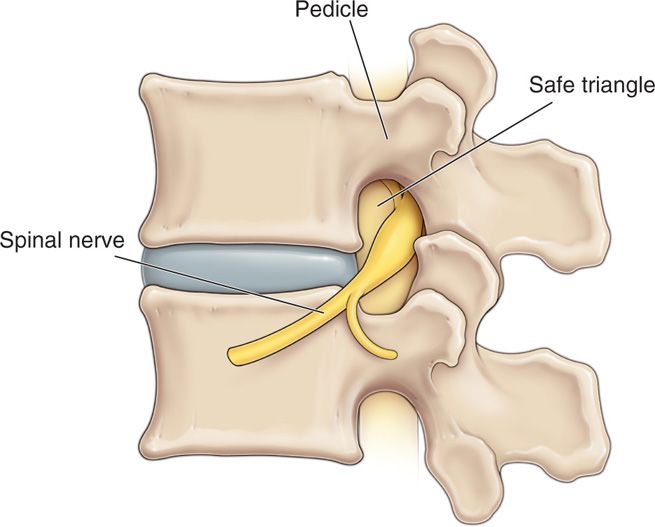
Figure 41-3. Lateral view of “safe triangle” in the anterior and superior aspect of foramen. Again, note lack of acknowledgement of vascular contents.
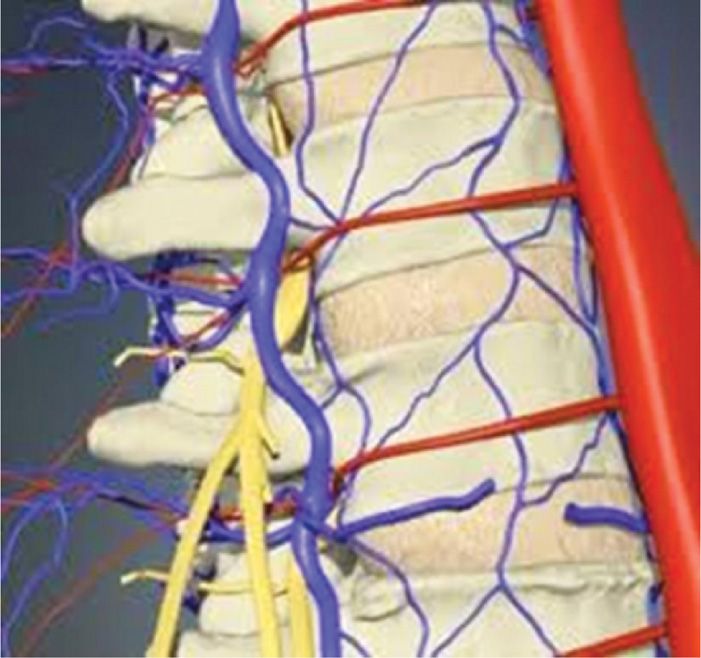
Figure 41-4. Typical course of arterial blood supply to spinal cord around waist of vertebra into the anterior and superior aspect of the intervertebral foramen—the location of the “safe triangle.”
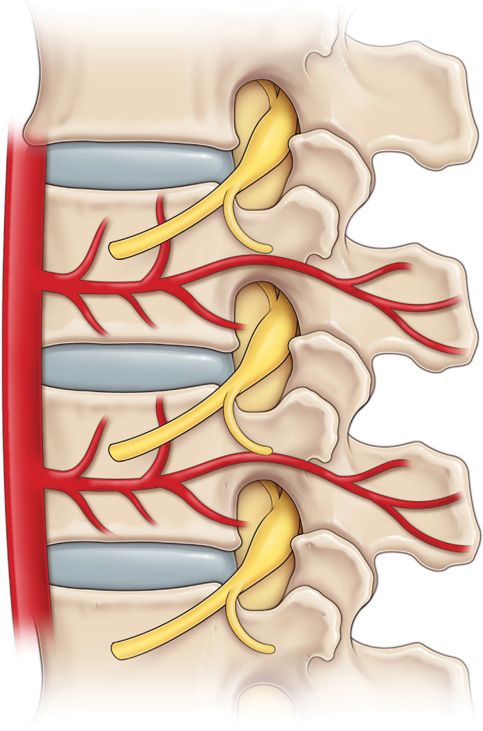
Figure 41-5. Typical segmental artery traversing waist of vertebra with radiculomedullary artery traveling through anterior and superior portion of foramen just under pedicle—the “safe triangle.”
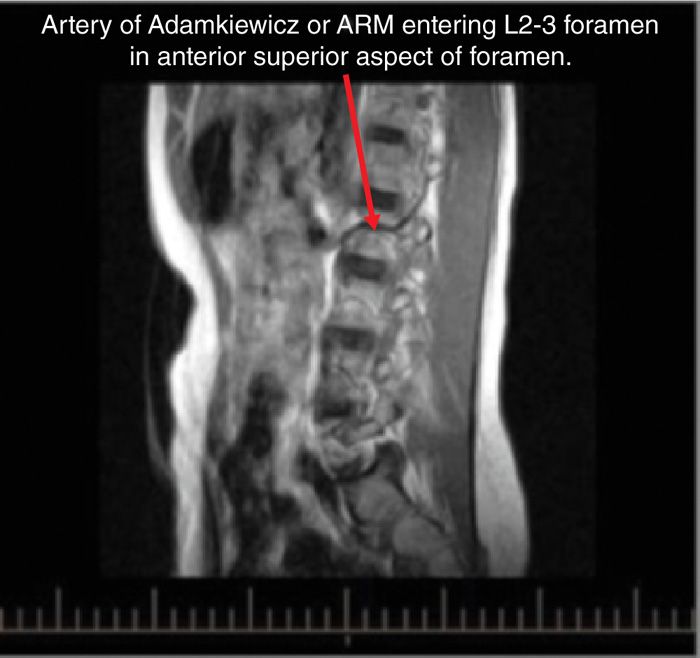
Figure 41-6. Enlarged segmental artery consistent with artery of Adamkiewicz traversing waist of L2 vertebra and entering L2-3 foramen in the anterior and superior aspect.
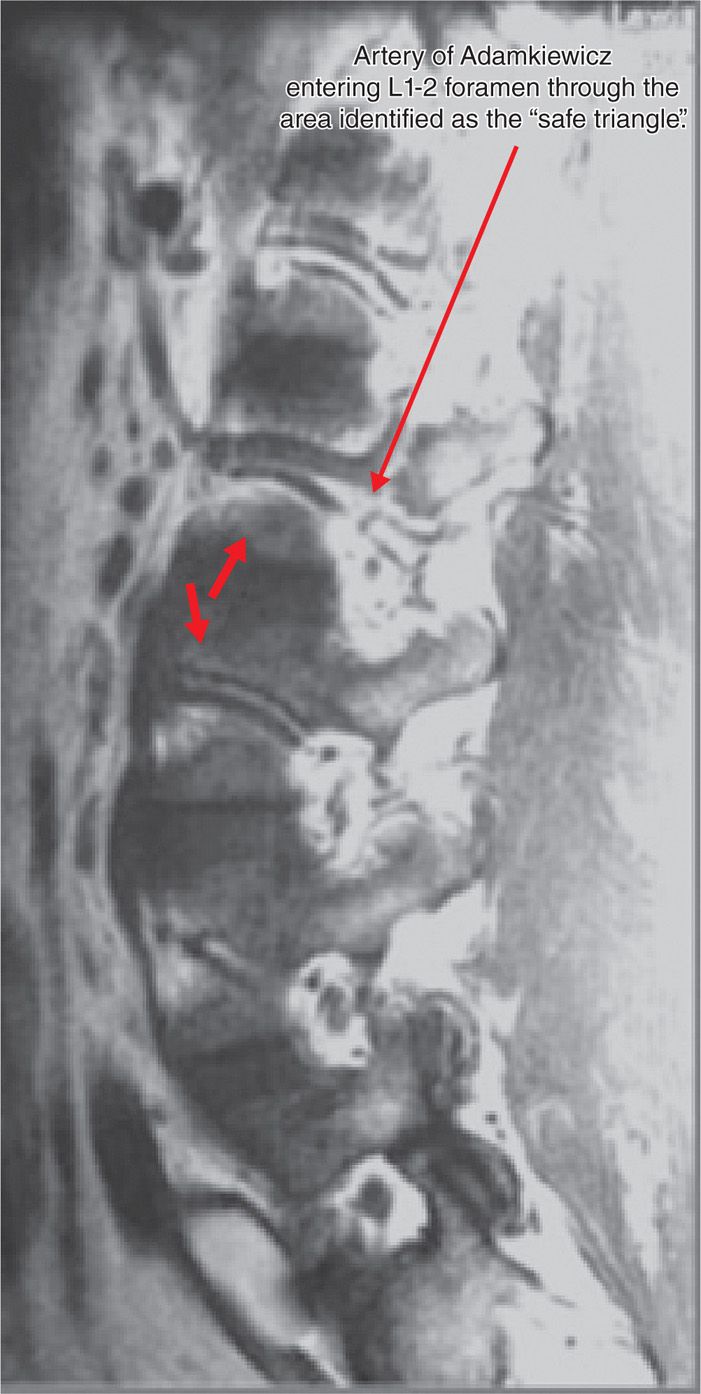
Figure 41-7. Parasagittal MRI slice revealing artery of Adamkiewicz entering anterior and superior aspect of L1-2 foramen just under pedicle after traversing waist of vertebra.
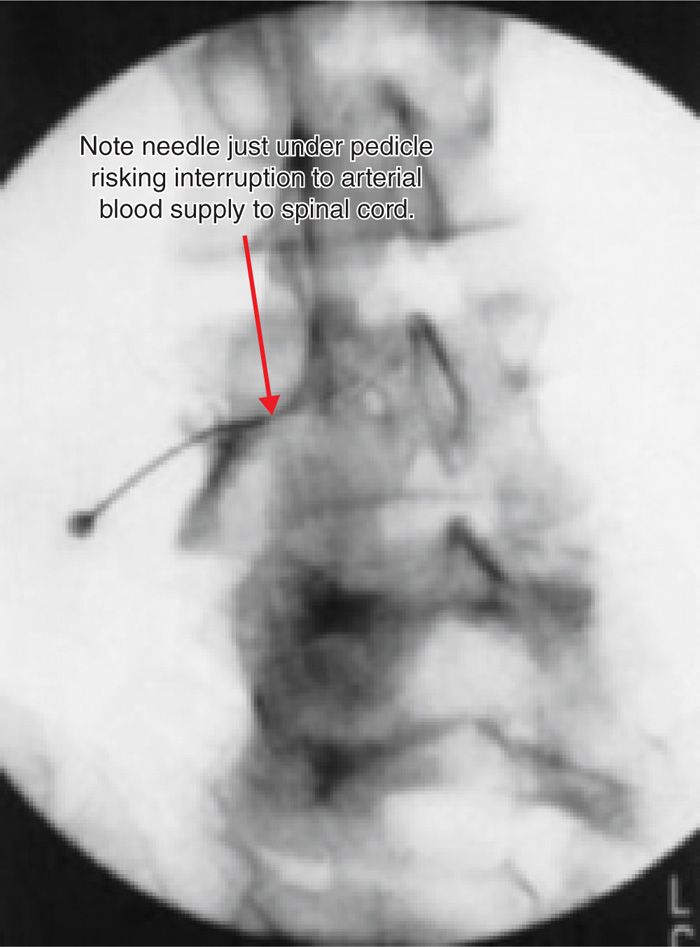
Figure 41-8. Example of dye injection following “safe triangle” approach for transforaminal injection. Presence of typical dye flow appearance is not a guarantee of safety as mechanism of injury may be related to vascular injury and not steroid embolism.
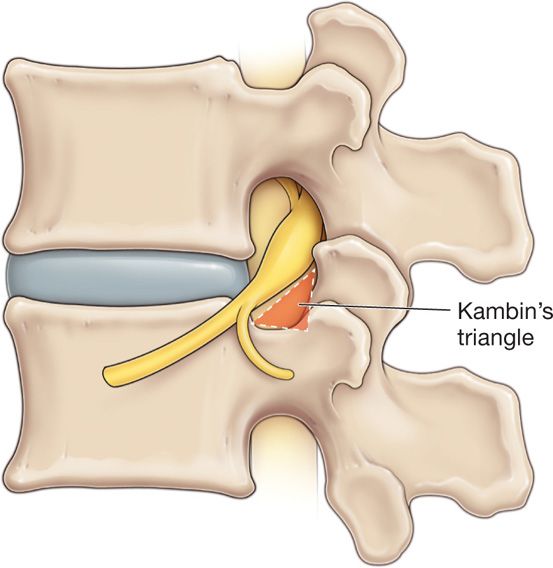
Figure 41-9. Location of the Kambin triangle with hypotenuse formed by exiting nerve root, base of triangle formed by superior endplate of inferior vertebra, and posterior aspect of triangle formed by the anterior facet joint.

Figure 41-10. Oblique approach to L4-5 transforaminal injection with pointer at skin entry site utilized for the Kambin triangle technique. End of pointer identifies skin entry site just lateral to SAP. Angle of obliquity slightly more than “safe triangle’ technique to ensure needle passes by lateral edge of SAP but remains medial enough to obtain adequate distribution of injectate. (Used with permission from Scott E. Glaser, MD.)
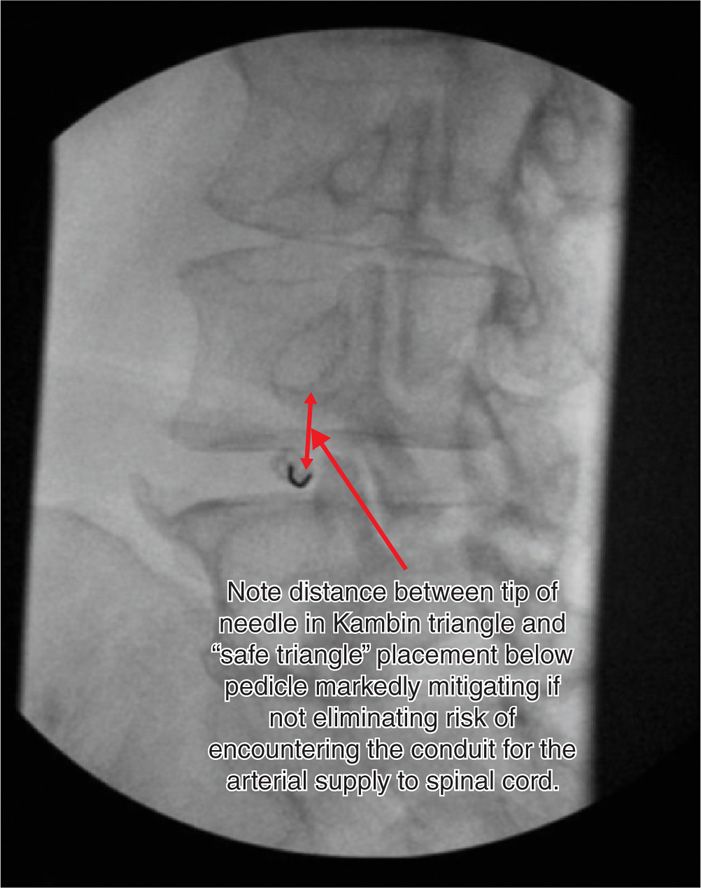
Figure 41-11. Coaxial technique for needle placement in the Kambin triangle. The needle has just been “walked” off the lateral edge of the SAP. (Used with permission from Scott E. Glaser, MD.)

Figure 41-12. Final needle location for transforaminal injection using the Kambin triangle technique. Needle bevel posterior to disc, and inferior in foramen. (Used with permission from Scott E. Glaser, MD.)
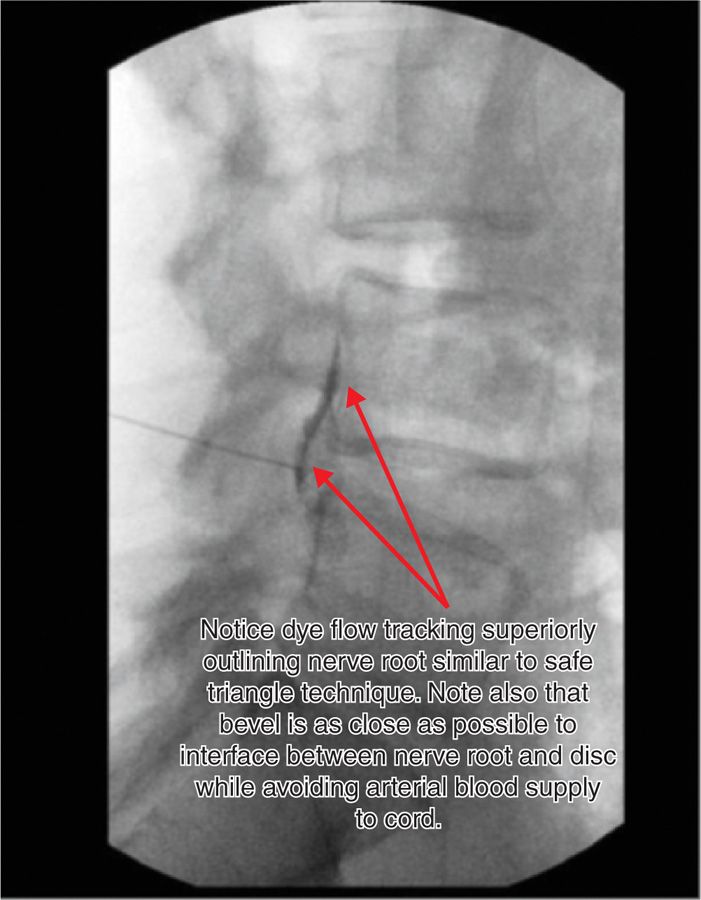
Figure 41-13. Appearance of dye flow on lateral view following the Kambin triangle technique. Note dye in anterior epidural space posterior to disc. (Courtesy of Scott E. Glaser, MD.)
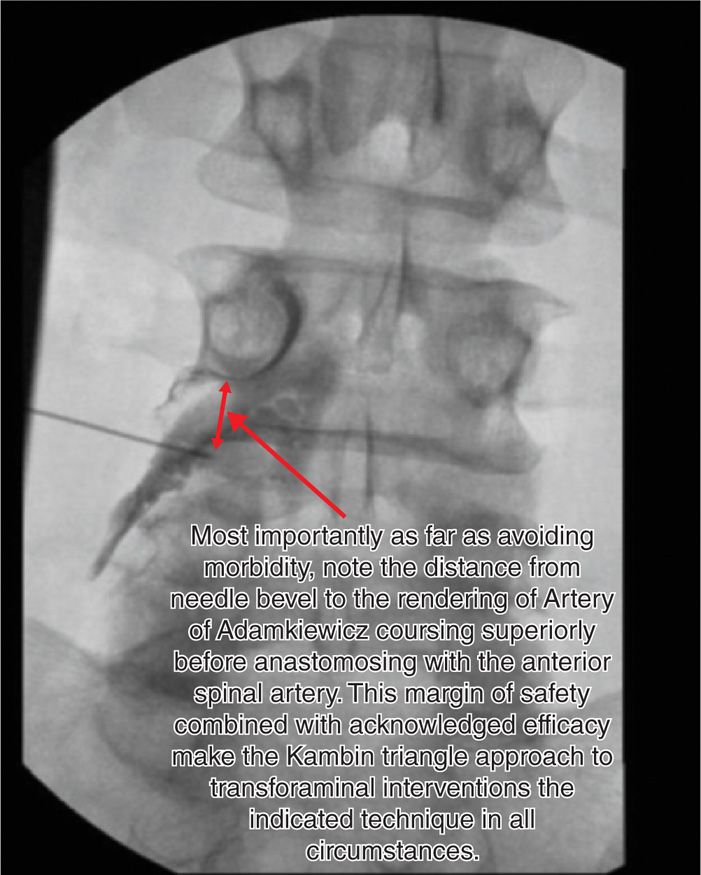
Figure 41-14. AP view following injection of dye using the Kambin triangle technique. Note excellent outline of nerve root and excellent dye flow medially and posterior to disc. (Used with permission from Scott E. Glaser, MD.)
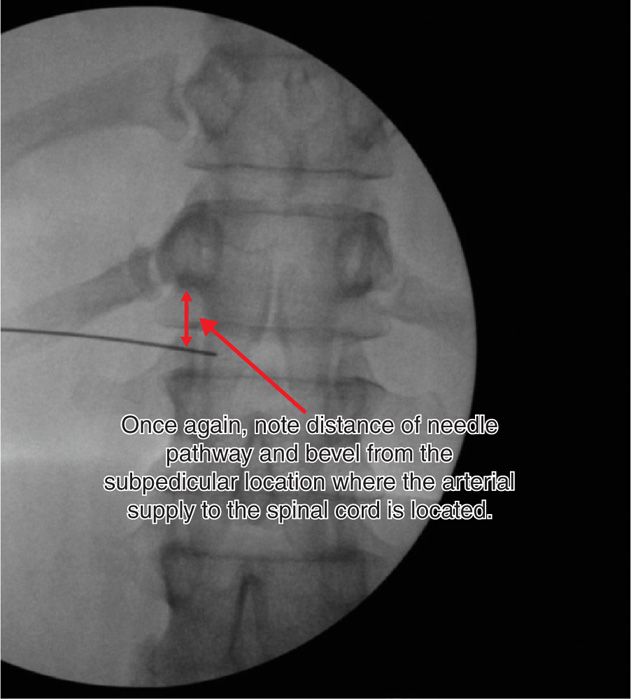
Figure 41-15. AP view of transdiscal celiac plexus block. Skin insertion site and needle trajectory similar to the Kambin triangle technique. (Used with permission from Scott E. Glaser, MD.)

Figure 41-16. Lateral view of transdiscal celiac plexus block. Note dye flow in prevertebral fascial plane. (Used with permission from Scott E. Glaser, MD.)

Figure 41-17. Cervical spinal cord infarction following cervical transforaminal epidural steroid injection. (Used with permission from Timothy Maus, MD.)
Based on the literature and expert opinions, it is clear that these complications occur more commonly following procedures performed in the cervical spine. This is based on a few factors including:
• Lower margin of safety because of the proximity of arteries supplying the brain and the proximity of the spinal cord itself.
• Random nature of the location of the vascular feeder arteries to the spinal cord within the cervical foramen and the lack of a foolproof strategy for avoiding them while performing procedures.
• Complications following cervical procedures appear to be related to the injury or transection of these arteries or embolism from injections into them.
In contradistinction to the cervical spine, the arterial supply to the thoracolumbar spinal cord follows a regular and recurring path along the vertebra and within the thoracic and lumbar foramen. The critical knowledge of vascular contents of the foramen cannot be ignored as the procedures performed in all three areas of the spine, especially transforaminal interventions, carry the risks of disastrous complications. Poor anatomicak knowledge has led to multiple cases of spinal cord damage and death documented in the peer reviewed literature and even more undocumented cases throughout the world.
The incidence of vascular complications following procedures in the thoracolumbar area of the spine clearly can be mitigated based on the knowledge of the location of the arterial blood supply. The following section of this chapter describes the important anatomy and provides a strategy for avoiding these arteries during procedures that put them at risk. Following that is a section on the cervical spine and the increased risks of procedures performed in that area of the spine and the pros and cons of strategies to reduce the risk of vascular complications.
THE RISK OF VASCULAR COMPLICATIONS IN THE THORACOLUMBAR SPINE
Indications for interventional procedures in the thoracolumbar spine include pain that originates from:
• Facet joints (arthropathy, synovitis)
• Intervertebral discs (herniated, degenerative)
• Spinal nerves
• Spinal stenosis
• Vertebral compression fractures
• Sympathetically maintained pain from the abdomen, pelvis, and lower extremities
• Neuropathic lower extremity pain
• Shingles and postherpetic neuralgia
• Coccygodynia
• Intercostal neuralgia
• Metastatic carcinoma
Representative procedures in the thoracolumbar spine include:
• Transforaminal epidural steroid injections
• Interlaminar epidural steroid injections
• Intra-articular facet joint injections
• Sacroiliac injections and neurolysis of medial and lateral branches
• Medial branch nerve blocks and neurolysis
• Sympathetic nerve blocks and neurolytic procedures
![]() Splanchnic nerves
Splanchnic nerves
![]() Celiac plexus
Celiac plexus
![]() Paravertebral sympathetic ganglia
Paravertebral sympathetic ganglia
![]() Superior hypogastric nerves
Superior hypogastric nerves
![]() Ganglion of Impar
Ganglion of Impar
![]() Epidural adhesiolysis
Epidural adhesiolysis
![]() Vertebroplasty, kyphoplasty, and sacroplasty
Vertebroplasty, kyphoplasty, and sacroplasty
![]() Spinal cord stimulation
Spinal cord stimulation
![]() Intrathecal pump
Intrathecal pump
![]() Rami communicans nerve blocks and neurolysis
Rami communicans nerve blocks and neurolysis
![]() Discography
Discography
![]() Intradiscal procedures
Intradiscal procedures
![]() Injections
Injections
![]() Decompressive procedures
Decompressive procedures
![]() Annular ablative procedures
Annular ablative procedures
Complications associated with these procedures include the following:
• Postdural puncture headache
• Nerve damage
• Spinal cord injury
• Paraplegia
• Cauda equina syndrome
• Epidural hematoma
• Epidural abscess
• Intravascular injection
• Pulmonary emboli
• Discitis
• Intrathecal granulomas
• Surgical site infections
• Intracranial hypotension
• Blindness.
• Pneumothorax
SPINAL CORD INJURY
Spinal cord injury and paraplegia, due to vascular ischemia, is one complication of grave concern; this complication has a unique association with thoracolumbar transforaminal epidural steroid injections. At least nineteen cases have been reported in the peer reviewed literature. The actual incidence is known to be much higher and may be increasing. Spinal cord damage has occurred following transforaminal procedures in multiple lumbar foramina including the right side and including the L5-S1 level. Unfortunately, many cases are not reported. The confidential nature of the legal process and physician’s reluctance to report complications limits disclosure.
In the case of lumbar transforaminal epidural steroid injections, the term “safe triangle” was appropriated for the recommended needle placement zone (Figures 41-2 and 41-3). Keeping the controversy of “safe triangle” in mind, authors suggest you make an explicit attempt to understand the vascular anatomy of this “safe” zone. We emphasize that the term “safe” should not be taken at literal value without extreme cautions. The major, if not the only, focus of this technique is to avoid injury to the nerve root and/or spinal cord.
The root cause is vascular injury that interrupts the blood supply to the thoracolumbar spinal cord. Downstream neurological ischemia and spinal cord damage occur.
VASCULAR INJURY
• The vascular injury occurs secondary to direct needle trauma, with or without injectate.
• The underlying pathophysiology is due to an intimal flap, arterial wall muscular spasm, complete transection, arterial dissection, and/or embolization of fresh thrombus after arterial dissection.
• Another theory is the embolization by injected particulate steroids.
• The other salient factor is an injury to the artery of Adamkiewicz—the major vascular supply to the spinal cord.
• For this reason alone, knowledge of spinal cord vascular anatomy is arguably the most important element in the performance of these procedures.
RELEVANT ANATOMY
• Radiculomedullary arteries provide the arterial blood supply to the spinal cord.
• The major source of blood supply to the anterior thoracic and lumbar spinal cord is the artery of Adamkiewicz or arteria radicularis magna (ARM).
• The radiculomedullary arteries including the ARM follow a predictable course from the aorta, around the waist of the vertebrae, and are predictably found in the anterior and superior aspect of the foramen (Figures 41-4 and 41-5).
• The ARM can be found in any thoracic or lumbar foramen.
Complex Vascular Supply of Spinal Cord
• The penultimate arterial supply to the spinal cord is mediated by the radiculomedullary arteries. They travel posteriorly, following a well-established course alongside the vertebral body (Figures 41-4 and 41-5).
• These vessels enter the spinal canal, while passing through a relatively constant position within the thoracic and lumbar foramina (Figure 41-5).
• This foraminal location is just inferolateral to the pedicle and in the upper anterior portion of the foramen (Figure 41-5).
• The radiculomedullary vessels have a constant location within any foramen—the upper anterior portion of the foramen (Figure 41-5).
• Moreover, the major conduit (artery of Adamkiewicz or arteria radicularis magna [ARM]), with a remote anastomosis to the anterior spinal artery, may traverse any foramen (Figure 41-6).
• The vascular anatomical variation carries a high risk of spinal cord injury and is not routinely addressed during the informed consent process and decision making by treating physician.
• The ARM is the major blood supply to the thoracolumbar spinal cord.
• Injury to the ARM carries a very high risk of spinal cord injury.
Radiculomedullary Arteries
• In the thoracic spine, radiculomedullary arteries are formed by posterior intercostal arteries.
• In the lumbar spine, radiculomedullary arteries are formed by paired lumbar arteries.
• At the thoracic levels 6 to 8, posterior intercostal arteries pass laterally and then, posteriorly along the anterolateral margin of the vertebral body towards the intervertebral foramen.
• This is the shortest route between the aorta and spinal cord.
• After the intercostal artery wraps around the lateral vertebral body groove, it passes medially under the pedicle.
• In the lumbar spine, the arteries originate more cephalically as they pass from the aorta en route to the foramen. Hence, they lie close to the superior endplate of the lumbar vertebral body.
• Each artery divides into a series of major branches (abdominal wall, intermediate or spinal canal, and the posterior body wall branches) just outside the level of the intervertebral foramina.
• The spinal canal (intermediate) branches divide into the anterior spinal canal, the nervous system, and the posterior spinal canal branches.
• The nervous system branches are the radiculomedullary arteries and they arise from this segmental artery, located just outside of the spinal canal.
• As the segmental artery courses around the posterior aspect of the vertebra, the arterial branches that comprise the radiculomedullary arteries course upwards toward the pedicle.
• They reach the superior edge of the adjacent nerve root, located just outside or within the foramen; they run along the dural nerve root sleeve for a short distance.
• These arteries supply blood to the spinal cord via direct cord penetration or regional anastomoses with the anterior spinal artery.
Artery of Adamkiewicz
• The unique radiculomedullary vessel, also known as arteria radicularis magna [ARM], is the artery of Adamkiewicz (Figures 41-6 and 41-7).
• This vessel is the major contributor to the anterior spinal artery.
• This artery does not directly supply the spinal cord but remotely anastomoses with the anterior spinal artery to supply the majority of the blood supply to the thoracolumbar spinal cord.
• After passing through the foramen, the ARM turns sharply and travels cephalad for several segments.
• Then this vessel makes a characteristic downward “hairpin” turn to anastomose with the anterior spinal artery.
• The most salient fact is that the ARM may enter the spinal canal at any intervertebral foramen, spanning T5 to L5 (Figures 41-6 and 41-7).
• In one study, in greater than two-thirds of cadavers, the ARM was found along the lumbar nerve roots. This anatomic study highlighted the “remarkable variability of the ARM origin” (Figures 41-6 and 41-7).
• The ARM enters the spinal canal on the left 69% to 85% of the time, based on anatomic and radiologic studies; and it enters the right side 15% to 31% of the time.
• The ARM might be duplicated in some individuals. It has also been shown in some patients to be split ipsilaterally between adjacent foramina or bilaterally between contralateral foramina.
• Like the other radiculomedullary arteries, the ARM will join the nerve root at the foramen.
• The artery then courses medially through the superoanterior part of the foramen, in close juxtaposition to the dorsal root ganglion-ventral root complex underneath the pedicle.
• The artery of Adamkiewicz can potentially be found at the mid vertebral body and the superior anterior foramen at every thoracic or lumbar level, care must be taken to perform procedures in a manner which minimizes the risk of the needle or instrument encountering the artery.
• This strategy is the only foolproof method to avoid vascular complications.
• It is important to detect intravascular injections of particulate steroid through the use of appropriate positioning of the fluoroscope, dye injection during live fluoroscopy, and digital subtraction imaging, to minimize potential embolization complication.
However, these techniques only prevent complications assuming one mechanism of injury, embolism of steroid. Strategies to detect intravascular uptake, although important, will not protect the patient from other mechanisms of injury including transection of the artery, intimal flap, and muscle spasm, local clot formation, and/or embolization of fresh thrombus after arterial dissection.
PROCEDURES WHICH PUT THE ARTERIAL BLOOD SUPPLY TO THE SPINAL CORD AT RISK
These procedures require placement of the bevel of a needle between the aorta and the foramen or in the foramen risk encountering the ARM as it traverses the mid vertebra and enters the foramen. These include:
• Transforaminal injections
• Sympathetic nerve blocks
• Procedures involving the rami communicans
Transforaminal Epidural Steroid Injections
• In the authors’ opinion, the key to safely performing transforaminal epidural steroid injections in the thoracic or lumbar spine is to avoid the superior anterior aspect of the foramen (“safe triangle”) secondary to the presence of the radiculomedullary arteries in this area (Figure 41-8).
• Our preferred technique is alternative locations for the placement of the needle include the inferior foramen, just posterior to the disc (the Kambin triangle) (Figure 41-9).
• Transforaminal epidural steroid injections performed by placing the needle in the Kambin triangle eliminates the risk of interrupting blood supply to the spinal cord as it eliminates the risk of encountering the artery of Adamkiewicz (Figures 41-8 and 41-9).
• The most important difference between the Kambin triangle technique and the “safe triangle” technique is that the needle will be placed in the foramen below the exiting nerve root and that the superior and anterior aspect of the foramen will be avoided (Figures 41-8 and 41-9).
• Performing transforaminal injections in this manner will obviate the risk of placing the needle in the area of the foramen that contains the blood supply to the spinal cord
• This eliminates the risk of encountering the artery of Adamkiewicz thereby minimizing the risk of spinal cord damage and paraplegia.
Our preferred technique utilized for performing transforaminal injections in the Kambin triangle is described below:
• Oblique approach, as with safe triangle approach, is utilized (Figures 41-10 and 41-11).
• Skin entry site is at mid discal level or lower, just lateral to SAP (Figures 41-10 and 41-11).
• Lateral edge of SAP can be used as depth gauge as well as intermittent lateral fluoroscopic views.
• Final needle position is at mid discal line or lower on A-P and lateral view (Figures 41-12 and 41-14).
• Final needle position is in pedicular line on A-P (Figure 41-14).
• Final needle position is in posterior to disc in foramen (Figures 41-12 and 41-13).
Sympathetic Blocks or Neurolytic Procedures
These include thoracic splanchnic, celiac, lumbar paravertebral, and superior hypogastric blocks:
• When performing interventions involving the sympathetic ganglia in the thoracic or lumbar region, care should be taken to avoid the mid portion of the vertebral body secondary to the presence of the radiculomedullary arteries in this area (Figures 41-15 and 41-16).
• Alternative locations for needle or instrument placement include the anterolateral aspect of the vertebral body close to the superior or inferior endplate or anterolateral to the disc.
• Another option is a transdiscal approach to the sympathetic chain (Figures 41-15 and 41-16).
• Oblique approach with lateral edge of transverse process even with lateral aspect of vertebral body is utilized.
• Skin entry site is lined up with lateral edge of vertebral body just inferior to superior endplate or superior to inferior endplate.
• Needle advanced to anterolateral aspect of vertebral body.
• Alternatively, a transdiscal approach may be utilized to obtain excellent needle placement in the prevertebral space while avoiding risk of spinal cord damage.
Clinical Pearls
• Concerns about an increased risk of discitis secondary to increased risk of intradiscal injections using this technique for TFESI may be unfounded.
• Should discitis occur, although serious, this is a complication that responds to appropriate treatment.
• In authors’ opinion, the outcomes using this technique for TFESI appear to be better than utilizing the safe triangle technique. This may be secondary to the fact that a higher concentration of medication is being deposited at the disc/nerve interface rather than tracking above the nerve and superiorly.
• In authors’ opinion, this technique also appears to improve outcomes for patients being treated for spinal stenosis or discogenic pain. This is presumably due to a higher concentration of medication being deposited in the epidural space just posterior to the disc.
THE RISK OF VASCULAR COMPLICATIONS IN THE CERVICAL SPINE
The indications for cervical procedures are included in the list at the start of the chapter. Many of the procedures listed in the start of the chapter are performed in the cervical spine as well. In addition, interventions directed at the sympathetic chain include stellate ganglion procedures such as ganglion blocks and neurolytic procedures. Other procedures performed in the cervical spine include:
• C1-2 joint injections
• Atlanto-occipital joint injections
• Occipital nerve blocks
The complications listed at the start of the chapter also occur following cervical interventions. In addition, other complications that have occurred include:
• Spinal cord infarction (Figure 41-17)
• Quadriplegia
• Seizure
• Coma
• Death
• Locked in syndrome
• Cerebellar herniation
• Brainstem infarction
• Brain infarction
Procedures in the cervical spine carry a greater risk of vascular and neurologic complications for the following reasons:
• One is the presence of the internal carotid artery in the carotid sheath and the vertebral artery which may be encountered by the needle or instrument or injected into during the procedure (Figure 41-19).
• The vertebral artery is especially at risk in the cervical spine based on its proximity to the foramen, pedicle, and vertebral body (Figures 41-18 and 41-19).
• This artery passes through the foramen transversum in the transverse process located in the upper 6 cervical vertebra just anterior to and in close proximity to the foramen (Figures 41-18 and 41-19).
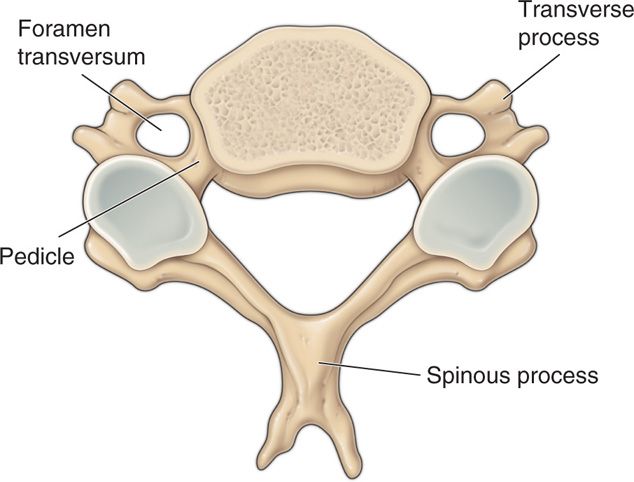
Figure 41-18. Note foramen transversum located immediately anterior to pedicle and foramen.
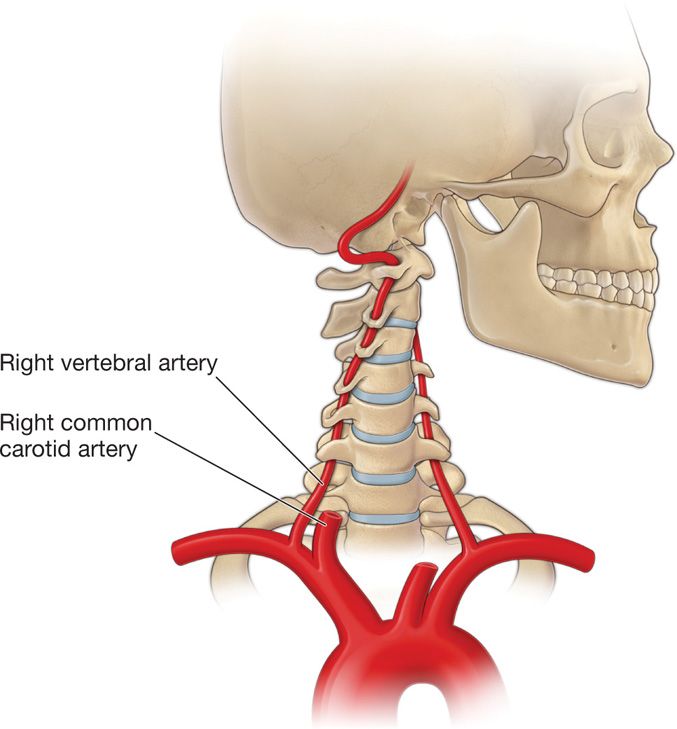
Figure 41-19. The course of the vertebral artery to the cranium. Again, note proximity to foramina, the C1-2 joint, and the atlanto-occipital joint.
• However, in 8% of the cases it passes through a foramen transversum in the seventh cervical vertebra.
Knowledge of this anatomical variation is extremely important especially when performing stellate ganglion blocks. The theories regarding the mechanism of injury leading to vascular complications with involvement of the vertebral artery include:
• Embolism of particulate steroid
• Arterial intimal flaps
• Arterial dissection
• Dislodgement of plaque causing embolism
• Arterial smooth muscle spasm
• Embolism of fresh thrombus following disruption of the intima
In some cases of mortality following a procedure, vertebral artery trauma and in one case dissection was found at post mortem. These complications have occurred following transforaminal injections, facet joint treatments, and stellate ganglion blocks.
BLOOD SUPPLY OF CERVICAL SPINAL CORD
In contradistinction to the vertebral artery which follows a predictable course except at C7 and which can be avoided utilizing appropriate techniques and safeguards, the location of the arterial blood supply to the cervical spinal cord in the foramina is variable (Figure 41-20).
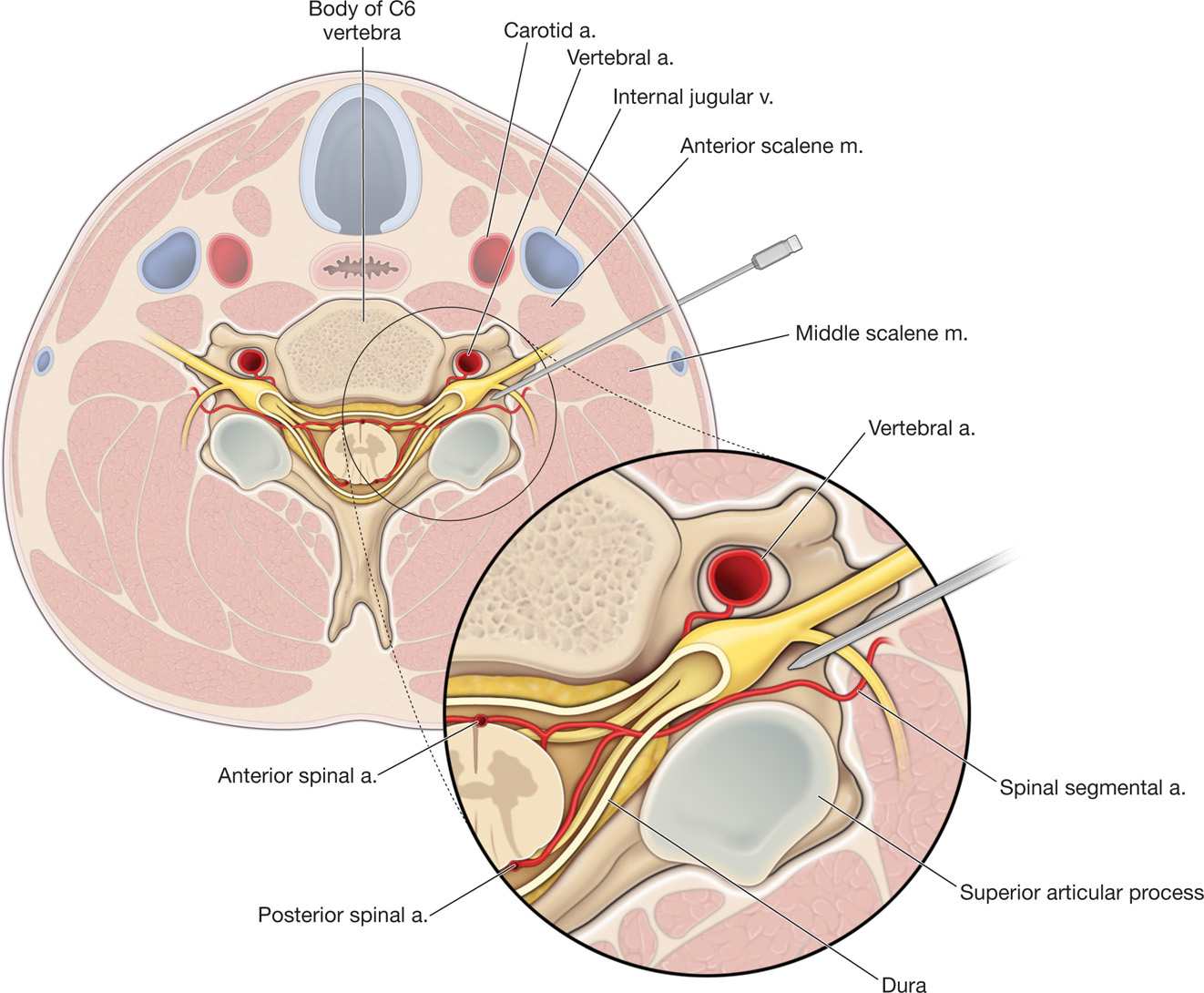
Figure 41-20. Anatomy of cervical intervertebral foramina. Note spinal segmental artery in posterior foramen. (From Atlas of Image Guided Interventions, Rathmell JP.)
• The radicular arteries supplying arterial supply to the spinal cord occur posteriorly and anteriorly and have been found running along both the anterior and posterior nerve roots.
• They supply the spinal cord in addition to the anterior spinal artery and the paired posterior spinal arteries.
• They are branches of the vertebral, costocervical, and thyrocervical trunks of the subclavian artery. More than one branch may enter the foramen at each level although usually only one radicular artery is found anteriorly.
• Most radicular arteries are small and supply only the nerve roots but in the areas of the spinal cord with higher metabolic requirements, the cervical and lumbar enlargement, some radicular arteries may supply the gray matter in the spinal cord.
• In addition, in the cervical spine, segmental medullary arteries, after supplying the dorsal or ventral nerve root, will continue on to reach and anastomose with the spinal arteries providing additional blood supply to the cord.
• There is more than one of these medullary arteries in the cervical spine whereas typically the lumbosacral cord is supplied by one such artery, the artery of Adamkiewicz.
• The fact that these medullary arteries may be found anywhere in the cervical foramen and that makes procedures performed in or near those foramina extremely dangerous (Figure 41-20).
• Additionally, it has been shown that there are variable anastomoses between vertebral and cervical arteries in the foramen leading to further risks of indirect injection into the vertebral artery through an anastomosis.
Unlike the lumbar and thoracic spinal canal where the segmental reinforcing artery, the artery of Adamkiewicz, can be reliably avoided using appropriate landmarks and techniques, the cervical arterial blood supply is always at risk during procedures in this area of the spine. In other words, it is not possible to reliably avoid interaction with these radicular and segmental arteries without a preprocedure angiogram as one cannot predict which foramen they are in or where in that foramen they are traveling. Thus, if one chooses to perform these procedures, one should choose one or more technique modifications to avoid injecting into or injuring the artery. Below are representative fluoroscopic pictures of a cervical transforaminal injection performed utilizing the most common technique in the posterior foramen (Figures 41-21A-C).
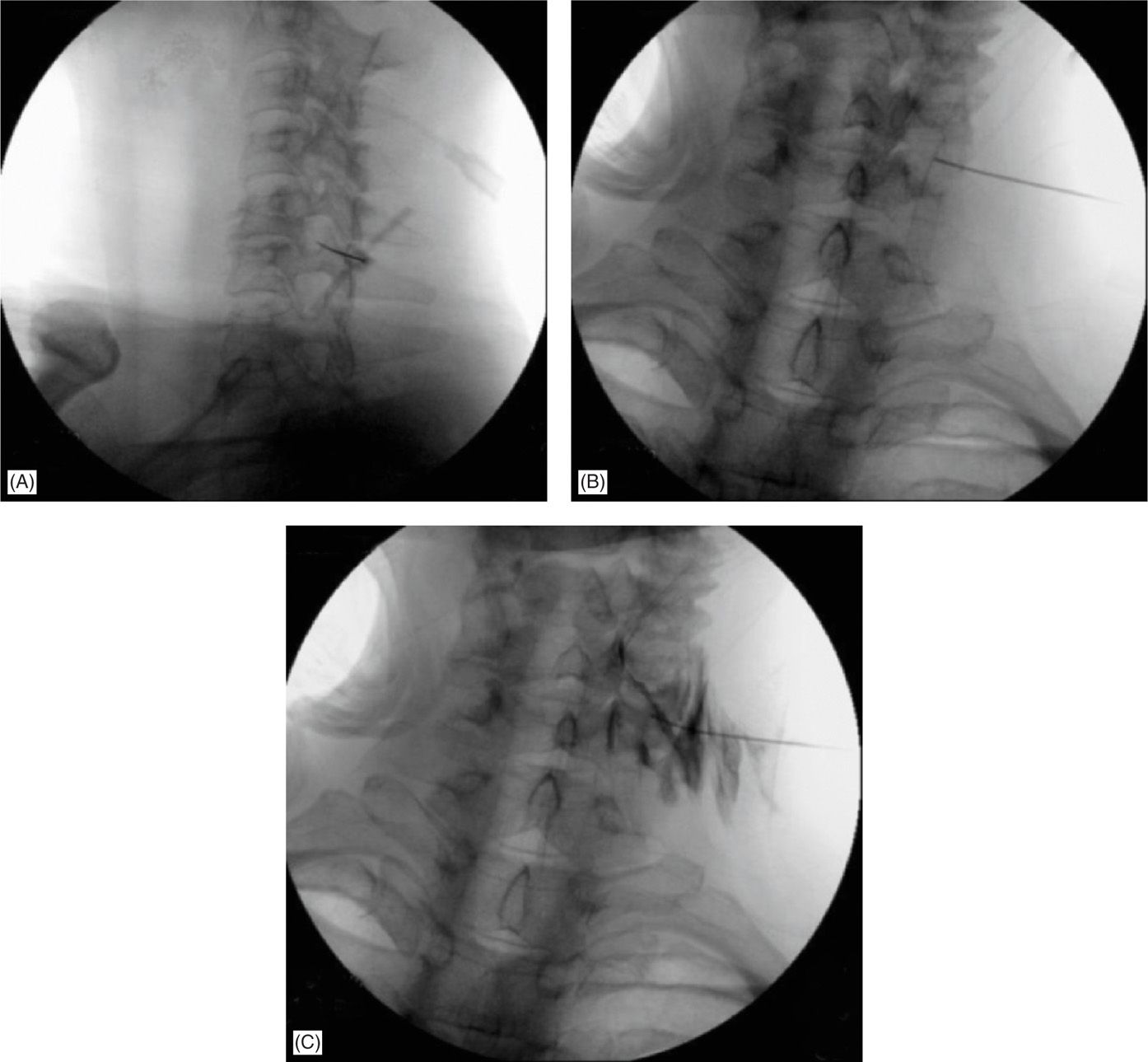
Figure 41-21. Left C5-6 cervical transforaminal approach, “selective nerve root block” with curved blunt needle; note dual contrast outline of exiting C6 spinal nerve, along with epidural and lateral muscular spread (needle orifice is proximal to needle tip—accounting for lateral contrast extravasation). (Used with permission from Rinoo Shah, MD, MBA.)
Many modifications of “traditional” techniques have been proposed and much written about them. The majority of these strategies hinge their success in preventing neurologic complications on the detection of intravascular uptake and the prevention of embolism.
FLAWS WITH “EMBOLISM” THEORIES OF VASCULAR INJURY
The flaws with this theory of injury only by embolism that it is possible to perform the safe and atraumatic cannulation and then decannulation of an artery without the benefit of direct observation. The assumption underlying these theories regarding the protective effect of detecting intravascular uptake rests on the belief that these small arteries can be entered and exited without any sequela as far as damage to that artery, This assumption also defies the fact that anatomic studies reveal that these radicular and medullary arteries are reliably smaller than a 22- or 25-gauge needle in their diameter. These theories also assume that after the cannulation of the artery, the injection of a particulate steroid leads to embolism distally leading to infarction.
The embolism only theory has led to much speculation in the literature. Unfortunately, the exact mechanism of injury is not known and is difficult if not impossible to prove. Also, and perhaps most importantly, there are other more logical mechanisms of injury with substantial support in the literature. As interesting as these theories may be, it is virtually impossible to assess their efficacy in reducing intra-arterial injections. And, once again, it is even more difficult to assess if there is any protective effect since any such effect is based on preventing only one unproven mechanism of injury, embolization of steroid.
The other mechanisms of injury leading to these complications include:
• Transection of the artery
• Creating arterial intimal flaps
• Traumatic arterial dissection
• Arterial smooth muscle spasm
• Embolization of fresh thrombus after arterial dissection
All of these mechanisms of injury or a combination of them may lead to cessation of arterial flow and infarction. These mechanisms also explain multiple cases found in the literature where dye flow appeared normal during the procedure yet catastrophic vascular complications occurred.
Technique modifications to detect intravascular uptake include:
• Minimum injection of dye under live fluoroscopy.
• Use of digital subtraction angiography (DSA) that can be performed with many of the fluoroscopes in use today can increase the ability of the operator to detect intravascular uptake.
• It has also been recommended that local anesthetic test doses should be employed with an appropriate waiting period to monitor the patient for side effects associated with intra-arterial injection of local anesthetic (seizures, loss of consciousness, transient neurologic deficits, etc).
• Another technique modification, the use of nonparticulate steroid, based on the assumption that embolization occurs by injecting particulate steroid intra-arterially during these procedures.
• Use of blunt needles.
• Use a cervical interlaminar approach coupled with a steerable catheter.
The assumption is that the injection of nonparticulate steroid prevents the effects of embolism, ie, infarction secondary to blockage of blood flow. Supporters point to the fact that there are no documented cases of vascular complications following the use of these steroids. Unfortunately, the number of cases known, although increasing, is low and the use of nonparticulate steroid is low as well.
The authors are concerned that the use of nonparticulate steroid may lead to a false sense of confidence for 2 reasons.
• Based on the other possible mechanisms of injury, it is obvious that steroid choice alone will not protect patients from all of the other injurious events that may occur to the artery.
• Secondly, although the nonparticulate steroid may not contain crystals, it is in and of itself a nonred blood cell containing embolus much like an air embolus and this fact may negate its protective value if, in fact, there is any.
Another protective maneuver that has been proposed is the use of blunt needles (Figures 41-21 and 41-22). This was not discussed in the section on thoracolumbar injections because therein risk reduction is afforded by avoiding the “safe triangle” and not by technical modifications. However, in the cervical spine, the lack of a regular anatomical pattern of the radicular and segmental arteries within the foramen makes it impossible to ensure that they can be avoided. With this knowledge and the multiple possible mechanisms of injury, the use of a blunt needle is an option, but the caveat is that the introducer is sharp and the blunt tip may cause discomfort as it passes through tissue planes. Like proponents of nonparticulate steroids, supporters of blunt needles point to the fact that there have been no case reports of vascular catastrophes associated with their use. Although, once again, this may not be dispositive because of the relatively low number of these of complications and the even lower use of blunt needles, it nevertheless is compelling. Proponents suggest that the blunt needles do not have a cutting edge bevel and therefore may protect against arterial injury. Like all other protective maneuvers, proving the protective efficacy of blunt needles at this time is most likely not possible.
Figure 41-22. Epimed blunt tipped needle. (Used with permission from Gabor Racz, MD, Epimed, Int’l.)
Another option is to use a cervical interlaminar approach coupled with a steerable catheter. This may have the combined advantages of the relative safety of the interlaminar approach and the “selectivity” of the transforaminal approach (Figure 41-23).

Figure 41-23. Targeted cervical epidural steroid injection with catheter. (Used with permission from Rinoo Shah, MD, MBA.)
SUMMARY
• Cervical transforaminal epidural steroid injections carry a higher risk than thoracolumbar transforaminal injections.
• Arterial injury causing vascular interruption during a cervical transforaminal is almost always consequential, whereas during a thoracolumbar transforaminal one has to injure the artery of Adamkiewicz.
• Furthermore, practitioners can be reasonably confident about accessing a cervical artery irrespective of needle location within a cervical foramen.
• In contrast, practitioners can be reasonably confident about accessing radiculomedullary vessels in the “safe” triangle and about avoiding them in the Kambin triangle.
• Risk reduction during cervical transforaminals injections may be afforded by technical modifications (nonparticulate steroids, blunt needles, digital substraction angiography, live contrast flow, local anesthetic test doses, slow injection, use of extension tubing to avoid excess needle manipulation, avoidance of heavy sedation, and patient feedback)—but many of these strategies remain unproven and are based on anecdotal evidence.
• Practitioners and patients must have a formal discussion and document that these are higher risk procedures and that this way, patient and practitioner are fully aware of the risks versus benefits.
• Authors’ recommendations in the thoracolumbar spine, avoid the “safe” triangle.
CLINICAL PEARLS
• Because of the increased risk associated with cervical procedures, practitioners should have extensive experience with procedures in the lumbar spine and appropriate training and mentoring before attempting procedures in the cervical spine.
• These procedures should only be performed in cases where failure of previous treatment, the severity of the symptomatology, and the lack of safer alternatives lead the reasonable doctor and patient to the conclusion that the risk is worth the benefit. An example would be a patient on opioids with a low quality of life secondary to the pain whose only other alternative would be surgery. The patient must be completely informed as to the doctor’s rationale and the risks and benefits.
• If these procedures are going to be performed, it is recommended that one or more protective maneuvers as reviewed above be carefully utilized.
• We also recommend the use of low dead space extension tubing to reduce movement of the needle tip during these extremely delicate procedures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






