UTI, FEBRILE
KATHY SHAW, MD, MSCE, MERCEDES M. BLACKSTONE, MD, PATRICIA LOPEZ, MSN, CRNP, AND CHRISTINE ROPER, BSN, RN
BACKGROUND (EPIDEMIOLOGY, EVIDENCE)
Acute pyelonephritis is currently the most common serious bacterial infection in childhood yet is difficult to detect on history or physical examination as symptoms are nonspecific. In the nonverbal infant or young child in diapers, fever is the primary finding. Although the risk of sepsis is small outside the neonatal period, it is not zero, with estimates as high as 3% in febrile infants 2 to 24 months. Early detection and treatment with antibiotics relieves symptoms and halts progression of disease as measured by nuclear renal scans done at time of diagnosis and improvement in inflammatory markers. There remains uncertainty in the relationship between childhood UTI and risk of end-stage renal failure based on current data, but there is general agreement that timely diagnosis and treatment of UTI in febrile infants is important.
Clinicians should be selective in screening young febrile children for UTI to avoid the consequences of false-positive tests, unnecessary catheterization, treatment, and imaging. Empiric treatment should be based upon results of the initial urine screen results. An understanding of specific risk factors for UTI in individual young febrile children helps the clinician to reduce unnecessary testing.
The 2011 guidelines from the American Academy of Pediatrics support using predictive models to rationally determine which young febrile children should be tested, using evidence-based predictors including height and duration of fever, sex, race, other potential sources for the infant’s fever, and circumcision status. This clinical pathway uses the predictive model by Gorelick and Shaw to help the clinician determine the pretest probability of UTI for a given child and whether screening is indicated. This selective approach allows one to avoid undesirable extremes—indiscriminately obtaining urine on all febrile children resulting in increased cost at little additional benefit, or the overly restrictive approach of not screening until the child presents with fever for 4 to 5 days.
Screening for UTI can be painful, time-consuming, and costly. This pathway describes a two-step approach to screening febrile children 6 to 24 months of age. Initially, a urine bag is placed to obtain urine for screening. A point-of-care (POC) urine dipstick is performed on children meeting specific criteria. If the urine screen is positive, urethral catheterization is performed to obtain sterile urine for culture. Urine specimens obtained via bag should not be sent for culture due to high contamination rates. Evidence supports the use of the urine dipstick; it performs as well as a standard urinalysis at less cost and yields a more timely result. Using specific values of moderate (2+) or large leukocyte esterase (3+) or presence of nitrites as threshold for obtaining a culture reduces the catheterization and false-positive rates. This two-step screening process allowed for a decrease in catheterization rates from 70% to <30% for screening in febrile children without increasing our ED length of stay.
PATHWAY GOALS AND MEASUREMENT
Goal
The goals of this clinical pathway are to standardize the following:
 Recommendations for screening for UTI in febrile children
Recommendations for screening for UTI in febrile children
 Urine collection and testing methods
Urine collection and testing methods
 Decrease number of unnecessary invasive catheterizations
Decrease number of unnecessary invasive catheterizations
 Ensure bag specimens are not sent for culture
Ensure bag specimens are not sent for culture
 Indications and antibiotic recommendations for empiric treatment
Indications and antibiotic recommendations for empiric treatment
Measurements
 Febrile children <2 years of age are appropriately screened for UTI
Febrile children <2 years of age are appropriately screened for UTI
 POC testing by urine dipstick is performed, not laboratory urinalysis
POC testing by urine dipstick is performed, not laboratory urinalysis
 Urine obtained for culture by correct method per age and toilet-training status
Urine obtained for culture by correct method per age and toilet-training status
 Appropriate empiric treatment based on UA results with correct antibiotic
Appropriate empiric treatment based on UA results with correct antibiotic
Algorithm and Key Hyperlinks
See Figure 92.1 (http://www.chop.edu/clinical-pathway/febrile-uti-clinicalpathway)
Associated Pathways
 Chapter 91 Shock (http://www.chop.edu/clinical-pathway/severe-sepsis-clinicalpathway-infants-28-days-age-and-children)
Chapter 91 Shock (http://www.chop.edu/clinical-pathway/severe-sepsis-clinicalpathway-infants-28-days-age-and-children)
 Chapter 82 Abdominal Pain in Postpubertal Girls (http://www.chop.edu/clinical-pathway/lower-abdominalpain-clinical-pathway-post-pubertal-girls)
Chapter 82 Abdominal Pain in Postpubertal Girls (http://www.chop.edu/clinical-pathway/lower-abdominalpain-clinical-pathway-post-pubertal-girls)
PATIENT POPULATIONS/STRATIFYING PATIENT RISKS
This pathway provides recommendations for the screening of infants >56 days and children through 18 years of age, with fever >38°C for possible UTI. These recommendations should not be used for patients with known urinary tract abnormality, neurogenic bladder, immunodeficiency, or recent GU surgery.
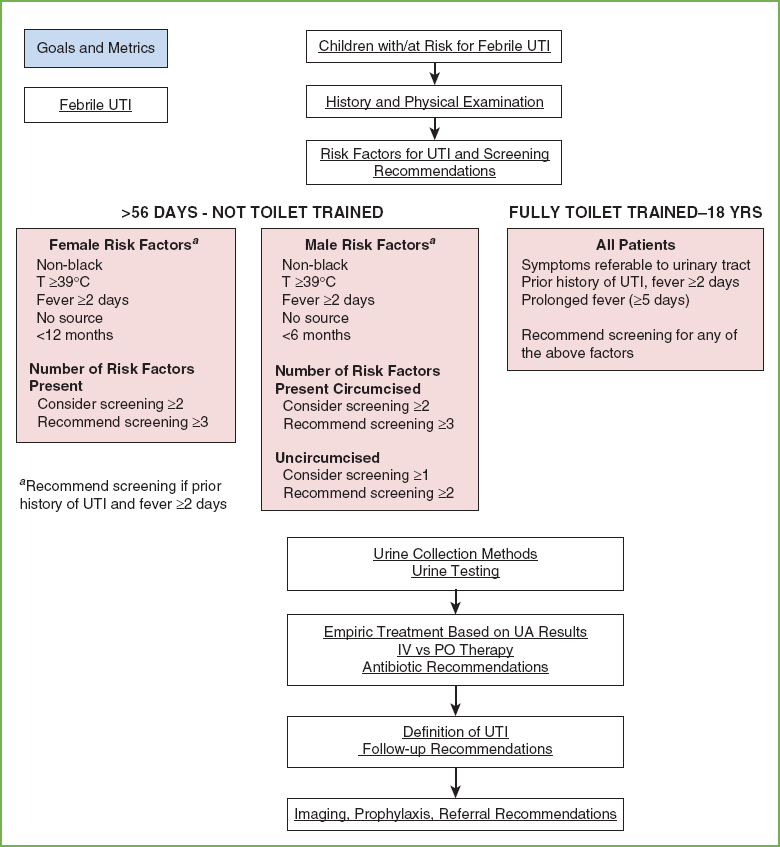
FIGURE 92.1 Pathway for the evaluation and treatment of children with febrile UTI. Pathway Authors: K. Shaw, MD; N. Plachter, CRNP; J. Lavelle, MD; T. Kolon, MD; M. Carr, MD; R. Keren, MD; R. Patel, MD; M. Dunne, MD; J. Kim, MD; J. Gerber, MD; M. Pradhan, MD; K. Ota, MD; C. Jacobstein, MD; K. McGowan, PhD; T. Metjian, PharmD.
Prospective epidemiologic studies have identified risk factors for UTI which can help stratify risk in febrile young children. Consider the following risk factors for young febrile children >56 days of age who are not yet toilet trained:
 White race
White race
 Fever ≥39°C
Fever ≥39°C
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







