CHAPTER 11 Use of the Electrocardiogram in Acute Myocardial Infarction
Inferior Myocardial Infarction
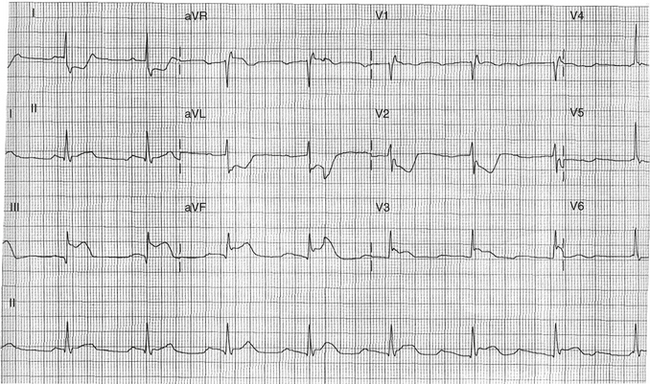
In 80% of cases, the culprit vessel in inferior myocardial infarction (MI) is the right coronary artery. The circumflex artery is the culprit vessel in all other cases, with the rare exception of a distally extending inferoapical “wraparound” left anterior descending artery, which is suggested when there is concomitant ST segment elevation in the precordial leads.1 ST segment elevation in lead III that exceeds the magnitude of elevation in lead II with reciprocating ST segment depressions in I and aVL of greater than 1 mm strongly suggests the right coronary artery as the culprit over the circumflex artery. The ST segment vector is directed toward the right when the right coronary artery is involved, which accounts for the elevation in lead III greater than lead II (Fig. 11-1). The added findings of electrocardiogram (ECG) evidence of right ventricle MI increases the specificity for the right coronary artery, and localizes the occlusion to a proximal location.2
Conversely, the circumflex artery is suggested when ST segment elevation in lead III is not greater than lead II, and by the absence of ST segment depression in leads I and aVL.3–5 An isoelectric or depressed ST segment with a negative T wave in lead V4R is very specific, but insensitive for proximal circumflex artery occlusion.6,7 ST segment depression in leads V1 and V2 has been reported to be specific for the circumflex artery, although a dominant right coronary artery can produce similar findings. The presence of ST depression in leads V1 and V2 with a prominent R wave in lead V2 can be nonspecific and can suggest involvement of the left ventricular posterior wall or concomitant disease in the left anterior descending artery. Performing an ECG with posterior leads (V7-V9) can show a primary posterior wall injury pattern with ST segment elevation. A localization schema for inferior MI is summarized in Table 11-1.
Table 11–1 Inferior Myocardial Infarction: ST Segment Elevation II, III, avF
| Right Coronary Artery | Circumflex Artery |
|---|---|
| ST segment elevation III > II | ST segment elevation II ≥ III |
| ST segment depression >1 mm I, avL | ST segment elevation I, avL, V5-V6 |
| ST segment elevation V4R or V1 | ST segment depression V4R |
Right Ventricle Myocardial Infarction
In the setting of inferior MI, right-sided precordial lead recordings are strongly indicated. The presence of right ventricular involvement portends a worse prognosis and enables the clinician to identify a subgroup of inferior MI with a propensity toward hemodynamic instability and shock leading to increased in-hospital mortality.8 Right ventricle MI is always associated with a proximal occlusion of the right coronary artery, before the takeoff of the right ventricular marginal branches. The most sensitive sign is 1 mm of ST segment elevation in lead V4R.9 This sign is not fully specific for right ventricle MI, however, because this can be seen in acute pulmonary embolus, anteroseptal MI, and pericarditis. ST segment elevation in lead V1 in association with elevation in leads II, III, and aVF is highly correlated with the presence of right ventricular infarction.2,10 Isolated right ventricle infarction, although rare, can be easily confused with anterior wall infarction, owing to the anterior location of the right ventricle, with ST segment elevation manifest only in the early precordial leads (V1-V3).11