Chapter 61
Upper Gastrointestinal Bleeding
Upper gastrointestinal bleeding (UGIB) is defined as bleeding from a source proximal to the ligament of Treitz (Table 61.1), associated with melena, hematemesis, coffee ground emesis, or aspiration of red blood from a nasogastric tube. Severe UGIB results in shock, orthostatic hypotension, decreased hemoglobin concentration (Hgb) by 3 to 4 g/dL, or a transfusion of at least two units of packed red blood cells (pRBCs). Severe UGIB generally necessitates admission to an intensive care unit (ICU) (Box 61.1). Although UGIB occurs more commonly in men, the overall mortality rate of 5% to 10% is similar for both sexes.
TABLE 61.1
Causes of Upper Gastrointestinal Bleeding and Their Frequency
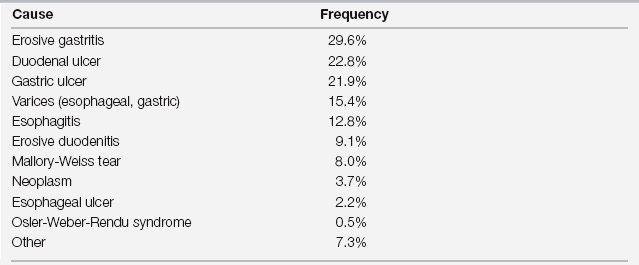
From Silverstein FE, Gilbert DA, Tedesco JF, et al: The national ASGE survey on upper gastrointestinal bleeding. I. Study design and baseline data. Gastrointest Endosc 27:73-79, 1981.
Assessment
When a patient presents with gastrointestinal bleeding (GI) bleeding, regardless of the source (upper or lower; see also Chapter 60), the initial management should focus on two main aspects: (1) volume resuscitation with appropriate intravenous (IV) fluids and blood products and (2) identification of the bleeding source, to allow selective therapy. The rapid initial assessment should include determination of vital signs and postural blood pressure changes, a focused history and physical examination, and gastric lavage.
Focused History
With a clear history of vomiting bright red blood or “coffee grounds” (blood present in the stomach long enough to be acidified by gastric acid turns brown), the localization of UGIB is straightforward. However, occasional bleeding from the posterior pharynx or the lung may be confused with UGIB (see also Chapter 79). Unfortunately, a history of melena, resulting from bacterial degradation of hemoglobin, remains nonspecific. Melena commonly arises from brisk UGIB, as well as from a small bowel source (distal of the ligament of Treitz) or a slow bleeding from the right colon.
Focused Physical Examination and Laboratory Evaluation
Intestinal metabolism of blood raises serum BUN so that a BUN:creatinine ratio > 20 (with both BUN and creatinine expressed in mg/dL) supports the diagnosis of UGIB. However, this nonspecific finding can be seen in hypovolemia alone.
Approach to Management
General Care
Initial management is individualized based on the patient’s hemodynamics, bleeding rate, and comorbidities. General recommendations for the ICU patient start with assuring ample intravenous access (Box 61.2). For hypotensive patients experiencing exsanguination, use short large-bore (7-8 Fr) catheters (often called rapid infusion catheters or trauma lines) in peripheral veins (or longer large-bore catheters in the internal jugular or femoral vein) with corresponding wide-bore tubing and special three-way stopcocks plus a blood warmer. Alternatively, 8 Fr catheter introducer sheaths, routinely used for insertion of pulmonary artery catheters, can also be used (but again without small-bore stopcocks). Initially, give normal saline or Ringer’s lactate solution, titrated to keep the heart rate at less than 100 beats per minute and the systolic blood pressure (BP) higher than 100 mm Hg or the mean BP > 60 to 65 mm Hg, if possible. Once available, preferentially replace lost blood volume by transfusing pRBCs. Transfusions remain critical for cirrhotics, who tend to redistribute crystalloids to the extravascular space and acquire massive total body fluid overload. Transfusion timing and thresholds depend on the patient’s hemodynamic stability, underlying conditions, comorbidities, and risk of further bleeding. As a general rule, early consultation with a gastroenterologist and, as appropriate, with an interventional radiologist and general surgeon is recommended for ICU patients with UGIB.
Endoscopic and Angiographic Interventions
Once the patient is stabilized (and rarely in the unstable patient experiencing exsanguination), urgent endoscopy should be considered. Endoscopy is indicated in resuscitated patients with active hemorrhage, blood product transfusion requirements, persistent hypovolemia, known or suspected portal hypertension, or suspected aortoenteric fistula. Patients who rebleed after initial stabilization should also undergo urgent endoscopy. Endoscopy can be deferred for up to 24 hours in patients with self-limited bleeding and no hemodynamic instability. Esophagogastroduodenoscopy (EGD) correctly identifies the source of bleeding in most cases and also provides valuable prognostic information while allowing the initiation of proper therapy. The accuracy in identifying the bleeding source is highest within the first 12 to 18 hours of hospital admission (approximately 90%) and falls by 30% or more after 24 hours. Accurate identification of endoscopic features can predict the risk of rebleeding (Table 61.2). Because oral radiologic contrast studies offer no therapeutic benefit, and contrast agents may interfere with subsequent endoscopy, they have no role in the initial evaluation of UGIB.
TABLE 61.2
Endoscopic Findings in Peptic Ulcers and Their Risk of Rebleeding
| Endoscopic Finding | Risk of Rebleeding |
| Arterial (pulsatile) bleeding | 85% |
| Nonbleeding visible vessel | 40%–50% |
| Adherent clot | 20%–30% |
| Oozing without visible vessel | 20% |
| Flat blood spot at ulcer base | 10% |
| Clean base | 5% |
From Silverstein FE, Gilbert DA, Tedesco JF, et al: The national ASGE survey on upper gastrointestinal bleeding. I. Study design and baseline data. Gastrointest Endosc 27:73-79, 1981.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




