27 Lynn M. Serrano and Dan Miulli Although many physicians treat children as “little adults,” a child’s physiological state is different than an adult’s, both metabolically and electrophysiologically. It should also be noted that children are in a constant state of growth that disrupts their equilibrium and necessitates adjustments. For these reasons, as well as because of the variety of disease pathologies, the treatment of children, particularly in the pediatric neurosurgical intensive care unit (NICU), requires extensive training and a degree of familiarity and comfort. Comanagement of the patient with a pediatrician or intensivist is recommended.1 Pediatric neurosurgical procedures, barring an emergency, should preferably be performed with a neurosurgeon well experienced in treating children. There are special neurosurgical considerations when treating the pediatric population in an intensive care situation.2,3 The lack of familiarity with and misunderstanding of necessary medical treatment often frighten children and their families. Any child under the age of 16 years should be placed in the pediatric ward. Special visitation should be allowed by close family members to comfort the child. Early involvement of a child life specialist or social worker is encouraged to help with expectations and transitions, as well as to follow up on concerns. Several studies confirm the benefit of a location within the ward of a “safe haven.” This is usually the playroom or family room. Within this safe haven there should be no medical conversations, patient care checks, or treatments.4–6 Intracellular fluid, as a percentage of total body water, is ~30% at birth and increases to 40% by 1 year of life. Adequate fluid and electrolyte maintenance is needed for general health maintenance, as well as for recovery from neurologic injury (Table 27–1).7 There are two ways to calculate baseline fluid requirements in children.8 The “kg method” is based on the weight of the patient, as follows: An alternative method for determining baseline intravenous (IV) fluids in children is the “meter squared method,” which is as follows: The healthy and ideal fluid and electrolyte status of any patient is normo-volemic with normal chemical balance. Of special consideration is brain injury or parenchymal edema from trauma or disease process. Like adult patients, pediatric patients with brain injury need to stay normal volemic to prevent brain edema. Sodium should stay on the high end of normal and glucose on the low end to decrease the risk of edema in patients with a broken blood–brain barrier. This rule of thumb does not hold true in endocrinological or systemic comorbidities or in spinal shock patients; these cases should treat the underlying pathology directly.9
Unique Pediatric Neurosurgical Intensive Care Unit Issues
 General Care Guidelines for Pediatric NICU Patients
General Care Guidelines for Pediatric NICU Patients
 Intravenous Fluids and Electrolytes
Intravenous Fluids and Electrolytes
| Electrolyte | Requirement |
| Sodium | 3–4 mEq/kg/day |
| Potassium | 2–3 mEq/kg/day |
| Glucose | 100–200 mg/kg/hour |
Source: Data from Gomella LG. Clinician’s Pocket Reference. Stamford, CT: Appleton & Lange; 1997.
| Weight (lb) | Body Surface Area(m2) |
| 3 | 0.1 |
| 6 | 0.2 |
| 12 | 0.3 |
| 18 | 0.4 |
| 24 | 0.5 |
| 30 | 0.6 |
| 36 | 0.7 |
| 42 | 0.8 |
| 48 | 0.9 |
| 60 | 1.0 |
| Each additional 10 lb | Add 0.1 |
| >100 | Treat as adult |
Source: Data from Fuhrman BP. Pediatric Critical Care. St. Louis, MO: CV Mosby; 1998.
 Respiratory Maintenance
Respiratory Maintenance
As with adults, pulmonary function and stability must be maintained in the pediatric NICU patient. Data regarding neurologic injury secondary to hypoxia within children are sparse. In general, adult guidelines should be followed, including oxygen saturation maintenance >95% and a minimum hemoglobin and hematocrit levels of 10.0 and 33.0, respectively, realizing that the normal pediatric values vary with age but are not much higher than these minimums. Children are much more sensitive to hemodynamic shifts than adults.10–13
The indications for endotracheal intubation are vast. The most obvious, of course, is respiratory distress or failure of any etiology. With pediatric NICU patients specifically, damage to the central nervous system (CNS) from infection, hemorrhage, trauma, hydrocephalus, or mass lesions can lead to the need for mechanical ventilation. Also, uncooperative patients, due to age, disease pathology, or closed head injury, may require temporary intubation to assist in ongoing care, including diagnosis, imaging, and treatment. Patients with cervical spine injuries should be intubated via an inline technique to minimize the risk of additional neurologic deficit. Those patients with possible or diagnosed facial trauma or anterior skull fractures should be intubated with direct visualization through the oral or nasal cavity as appropriate to minimize possible brain penetration, additional damage, or misplacement of the tubing.
Patients with raised intracranial pressure (ICP) regardless of etiology may benefit from intubation. Care should be taken to intubate these patients, as the procedure itself may increase cerebral blood flow and subsequently ICP. Adequate sedation may help alleviate this problem. Under normal circumstances, cerebral oxygen requirements are coupled with cerebral blood flow, and are increased with temperature, activity, agitation, seizure, and injury. Blood flow will increase as the partial pressure of oxygen in arterial blood (PaO 2) falls below 60 or as the partial pressure of carbon dioxide in arterial blood (PaCO2) increases. NICU patients require higher PaO2 levels and low to normal PaCO2 levels to optimize recovery. In an acute neurologic decline, a temporary period of mild hyperventilation may help minimize edema and provide the necessary time for definitive diagnostic or treatment measures, but it should never be used as maintenance treatment of elevated ICP.10,11
A stepwise approach should be taken when intubating pediatric NICU patients. Of course, adequate sedation and pain management are necessary, as discussed earlier. The equipment should be prepared and set up at the bedside. Vital signs should be recorded every 2 minutes. Provide 100% oxygen prior to starting the procedure (and consider assisted hyperventilation if applicable). Assess the patient for a possible difficult airway and familiarize yourself with the patient’s cricoid and neck curvature. Always consider the possible need for inline or fiberoptic intubation after traumatic injuries or unknown spinal cord status. If there is associated cardiovascular compromise or hypovolemia, use diazepam or midazolam and/or fentanyl, plus lidocaine and vecuronium or another relaxant. Without these associated conditions, you can replace the diazepam/midazolam and fentanyl with thiopental. When adequate medication effect is achieved, the laryngoscopy or endotracheal intubation can be completed.
Arterial lines should be placed on all intubated patients to provide not only reliable, easily attainable blood pressure parameters but also arterial access for blood gas analysis. Arterial blood gas analysis should be performed with every ventilator adjustment, any clinical change, and as a baseline on intubated patients twice daily.
 Intracranial Pressure and Cerebral Blood Flow
Intracranial Pressure and Cerebral Blood Flow
Cerebral perfusion pressure (CPP) is the pressure via which blood and nutrients are delivered to the brain. As ICP increases, or mean arterial pressure (MAP) decreases, the CPP will also decrease, which will ultimately decrease cerebral blood flow. Normal cerebral blood flow in adults is 50 mL/100 g/minute. Gray matter blood flow is ~4 times higher than white matter. Newborn blood flow is ~40 mL/100 g/minute. Cerebral blood flow then increases to accommodate growth and learning. By age 4, the average cerebral blood flow is 108 mL/100 g/minute and can remain as high as twice that of adults until 18 years of age.14–16
In children, it is often difficult to measure ICP. Ventriculostomies can be used as a direct measurement; however, an accurate examination can suggest elevated ICP as well. Papilledema is often a late finding of elevated ICP in children relative to adults, whereas vomiting occurs much more regularly and reliably as a predictive symptom. Assessment of fontanelles can also yield pressure data. Note that when children are lying flat or having a Valsalva’s maneuver, fontanelles can be bulging and firm without abnormality. However, in the sitting position, a calm child should have soft, non-bulging fontanelles; any firmness or bulge is suggestive of elevated ICP. Another useful clinical gauge of ICP is head circumference. Although head circumference abnormalities can stem from a variety of causes, it can be used to suspect intracranial pathology and possibly high ICP, particularly if augmented by other clinical findings. An estimation of ICP is 1.5 to 6.0 mm Hg in children <2 years of age, equal to the child’s age in the 2 to 15 year range, and 8 to 15 mm Hg in children and adults >15 years old.
In the pediatric NICU, ICP and CPP are treated as the fifth and sixth vital signs. Evaluation, early identification of trends, and rapid treatment can prevent additional neurologic decline and improve outcome.
 Nutrition
Nutrition
States of physical and/or psychological stress change the metabolic needs of patients. Nutritional support is vital to the management and outcome of pediatric NICU patients. Most clinical research has been directed toward adult patients; however, most concepts carry over to children. In the 1960s, total parenteral nutrition (TPN) became widely used and helped to relieve the metabolic component of the systemic stress response. However, more recently, natural enteral support has been advocated to facilitate gut motility, mucosal healthiness, and natural flora preservation.8 In particular, neonate patient data have suggested even small amounts of gastrointestinal feedings promote enterohepatic enzyme delivery, reduce mucosal atrophy, and decrease the risk of jaundice.17,18
Regardless of the mode of nutrition, the goal should be to maintain fluids, electrolytes, and vitamins, as well as to provide adequate calorie intake for a metabolically stressed and altered system. Some recent literature has suggested the need for an increased amount of protein, but there are conflicting views on this.8,12 The basal energy expenditures of patients in various states can be estimated by modified normograms based on the Harris-Benedict formula19 or by respirometry and indirect calorimetry.
Tables 27–3, 27–4, and 27–5 are examples of normograms used to determine and apply the basal energy expenditure of patients in critical care settings.8
| Age (in years) | Calories (kcal/kg) |
| <40 weeks’ gestation | 80 |
| 0–1 | 90–120 |
| 1–7 | 75–90 |
| 7–12 | 60–75 |
| 12–18 | 45–60 |
| Percent increase in caloric requirement | Pathological condition |
| 12 | Every degree temperature > 37°C |
| 20–30 | Major surgery |
| 40–50 | Sepsis |
| 50–100 | Failure to thrive |
Source: Data from Farrell MM. Brain death in the pediatric patient: historical, sociological, religious, cultural, legal, and ethical considerations. Crit Care Med 1993;21:1951–1965.
| Age(years) | Males (kcal)m2/hour | Females (kcal)m2/hour |
| 1 | 53 | 53 |
| 2–3 | 52 | 52 |
| 4–5 | 50 | 49 |
| 6–7 | 48 | 46 |
| 8–9 | 46 | 43 |
| 10–11 | 44 | 42 |
| 12–13 | 42 | 41 |
| 14–15 | 42 | 39 |
| 16–17 | 41 | 37 |
| 18–19 | 40 | 36 |
| 20–25 | 38 | 35 |
Source: Data from Farrell MM. Brain death in the pediatric patient: historical, sociological, religious, cultural, legal, and ethical considerations. Crit Care Med 1993;21:1951–1965.
Body Surface Area (m2) = square root of [(height (cm) × weight (kg))/3600]
 Activity Level
Activity Level
The activity level of children in the NICU setting will vary depending on pathology. The general rule is to mobilize, mobilize, mobilize.
Intubated patients are the exception to this rule, as being intubated can be a traumatic state, misinterpreted by children of any age. These patients should be kept under adequate sedation and pain management. Infectious patients can increase activity within their secured environment, and bed rest patients can adjust the head of the bed. Patients with head of bed alteration limitations due to weight-bearing restrictions, drains, or underlying pathology, such as intracranial edema or spinal fluid circulation considerations, should adjust their activity within the parameters set by their condition but try to keep the head of bed greater than 30 degrees above horizontal if safe.
Cervical collars and spinal braces, depending on the injury or baseline etiology causing the need for support, can be worn out of bed, and patients are still encouraged to increase activity. Braces should be worn snuggly and secured adequately to maximize support and minimize slipping or discomfort during activity. Some patients prefer to have a liner of gauze or piece of material such as a shirt under the brace to prevent skin contact and irritation.
Activity can decrease the risk of comorbidities associated with hospitalization, including deep vein thrombosis, pulmonary embolisms, pneumonia, constipation, and pressure sores. Also, depression has been shown to be decreased among patients with out-of-bed activities and environmental changes. Environmental changes can consist of outside visits, hallway walks, wheelchair excursions, or simply a change in the furniture setup within the room.
Patients with indwelling deep tissue drains or open shunt systems should not be allowed into common areas secondary to the risk of contamination. These patients should still increase activity as tolerated, but the security of the drain system should be monitored.
 Pharmacology
Pharmacology
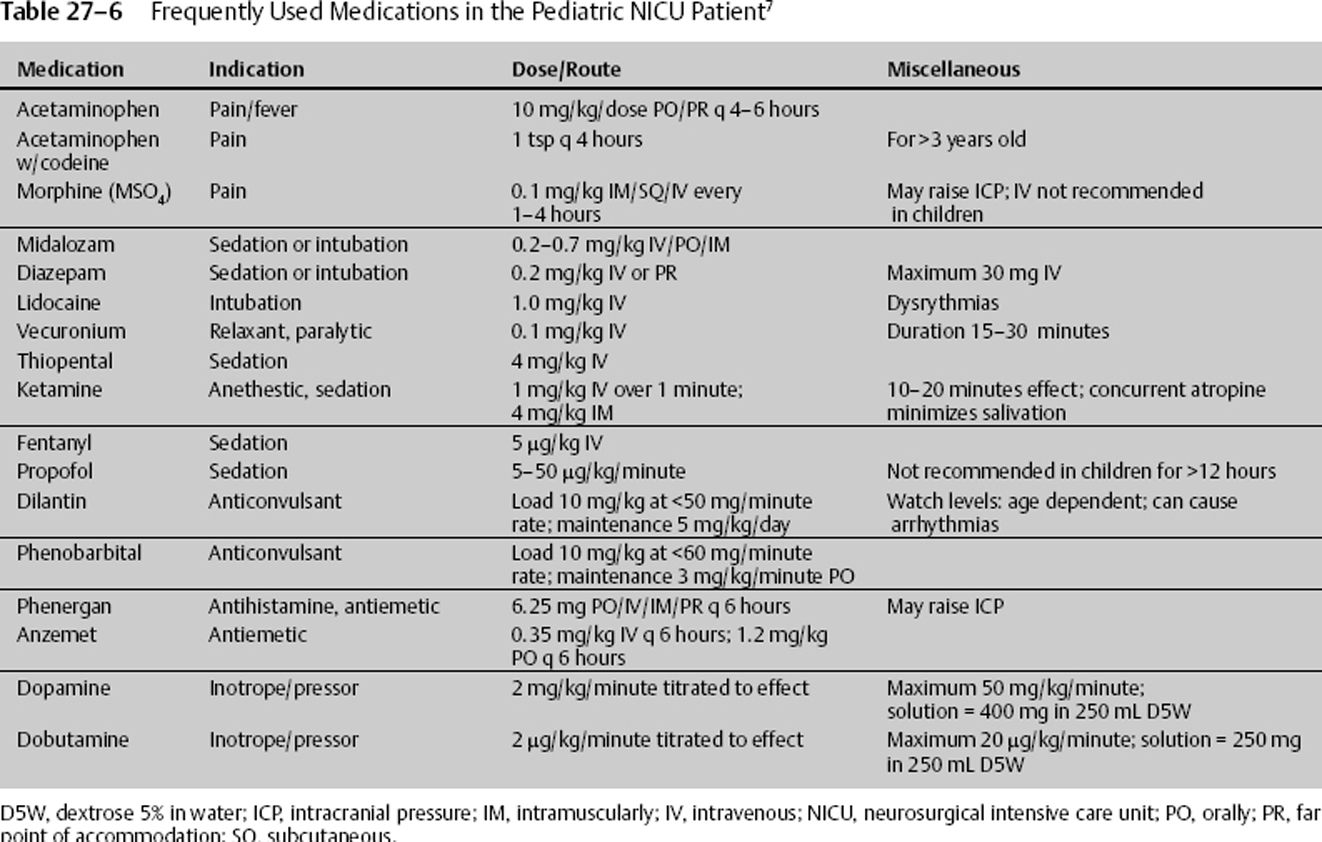
Injectable, oral, rectal, and transdermal medications are all used in children. Special attention is paid to dosing, preparation, delivery, and administration. Due to the lack of judgment expressed in children, IV medications are frequently used in the pediatric NICU setting to facilitate compliance and limit discomfort during administration. Dosing is usually by weight and/or therapeutic level maintenance. Table 27–6 lists several of the medications frequently used in the care of pediatric NICU patients.20,21
If medications require piggybacking, the suggested fluid is 0.9% normal saline. The additional osmolarity and sodium, as well as the lack of sugar, will help with edema. An exception to this is in the setting of electrolyte imbalance or endocrine pathology, whether or not related to the neurosurgical diagnosis. In these cases, a risk-to-benefit ratio as well as ease of treatment of the adverse reaction must be weighed when determining the fluid base in which to mix medication.
When giving IV medications, there are five questions that should be asked by administering staff, in addition to confirming the dose of the drug:
- Is the line large enough to accommodate the drug, and is the line in adequate position?
- Is the patient’s cardiac function strong enough to dilute and circulate the drug effectively?
- Does the infusion require a pump, or can it be administered directly?
- Is there a need for titratable or prn (as circumstances may require) dosing?
- Are there any drug-to-drug interactions or special administration instructions with the drug in question? Can it be given with TPN/tube feeds?
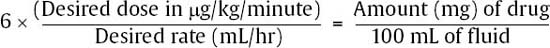
Also, when required to maximally concentrate fluid solutions, the “rule of six” should be applied. The rule of six (not to be confused with the “rule of sixes”; see Table 27–2) states that 6 times the patient’s weight is equal to the amount of drug (mg) that, in 100 mL of fluid, will result in a solution delivering 1 μg/kg/minute when infused at 1 mL/hour. (Note: For two drugs, epinephrine and isoproterenol, 0.6 should be used.) Stated mathematically:
Studies have shown the most common mistake made with drug administration is carelessness in dosing because of a lack of time to recheck dosage instructions, miscalculations, or presumed familiarity with a particular drug. This problem is preventable.
 Medical Imaging
Medical Imaging
There is a significant overlap between adults and children in regard to medical imaging. As a general rule, if a study is needed for diagnosis, treatment, or follow-up, then it must be done. Unnecessary studies are avoided in both subsets of patients to prevent unnecessary cost accumulation and radiation exposure, not to mention discomfort, the risk of transport, and systemic difficulties in obtaining the tests. In particular with children is the concern of radiation exposure on their developing system and bone growth. The average chest x-ray radiation exposure is 1.4 mGy, and the average head computed tomography (CT) scan radiation exposure is 8.0 mGy. Most literature suggests adverse effects do not start occurring until after exposure to 100 mGy.22 Young children also are usually not as cooperative and have difficulty lying still. Frequently, conscious sedation or temporary intubation is required to obtain an adequate study. This then exposes the patient to another set of risks, and the benefit-to-risk ratio needs to be clearly discussed with the legal guardians, as well as with other medical staff involved in the case. Whether sedation is required or not, it should be noted that there are risks to transporting critically ill patients to the radiology department. Risks include environmental exposure, infection, accidental line removal, systemic instability, and positional difficulties. Because of these risks, medically necessary imaging should be portable if possible and of acceptable quality; if transport to the radiology department is pertinent, all necessary studies from all disciplines should be performed during one trip to minimize risks and promote efficiency. This requires effective communication between complex multidisciplinary care plans.
| Response | Score |
| Eye opening | |
| Spontaneous | 4 |
| To speech | 3 |
| To pain | 2 |
| None | 1 |
| Verbal | |
| Coos, babbles | 5 |
| Irritable cry | 4 |
| Cries to pain only | 3 |
| Moans to pain only | 2 |
| None | 1 |
| Motor | |
| Normal spontaneous movements | 6 |
| Withdraws to touch | 5 |
| Withdraws to pain | 4 |
| Abnormal flexion | 3 |
| Abnormal extension | 2 |
| None | 1 |
 The Pediatric Neurologic Exam
The Pediatric Neurologic Exam
Unlike adult examinations, there is no rigid normal baseline in a pediatric neurologic exam. Developmental milestones should be met sequentially and have been well documented; however, minimal timeline variations and personality trends do occur that can affect an exam at any given point.
The examiner should take into account the age of the child. The child should be placed in a comfortable setting with family present if possible. Much of the pediatric exam can be done while observing and interacting with the patient, paying close attention to facial expressions and the eyes, any verbalizations, and motor interactions. The pupils must be examined, even in uncooperative patients: no exceptions. Also, a head circumference and body weight should be documented and trends followed. The remainder of the exam can use a modified Glasgow Coma Scale format. Such standardizations help document exams reliably and reproducibly (Tables 27–7 and 27–8).23
During infancy, children can exhibit flexor activity while sleeping; this is a normal variant. Also, children can have asymmetric blink and dysconju-gate gaze up to 6 months of age without concern. A positive plantar or Babinski’s reflex can occur normally up to 1 year of age, as well as areflexia or hyperreflexia of deep tendon reflexes.
| Response | Score |
| Ocular | |
| Pursuit | 4 |
| EOM intact, reactive pupils | 3 |
| EOM impaired | 2 |
| EOM paralyzed, fixed pupils | 1 |
| Verbal | |
| Cries | 3 |
| Spontaneous respirations | 2 |
| Apneic | 1 |
| Motor | |
| Flexes and extends | 4 |
| Withdraws from painful stimuli | 3 |
| Hypertonic | 2 |
| Flaccid | 1 |
EOM, extraocular muscles.
< div class='tao-gold-member'>