Route of needle entry
Site of injury
Interlaminar approach
1. Injury to the spinal cord
2. Injury of spinal nerve, ventral or dorsal ramus with lateral deviation of the needle
Transforaminal approach
1. Injury to spinal nerve
2. Injury to ventral or dorsal ramus
3. Injury to spinal cord
4. Injury to vertebral, ascending or deep cervical arteries
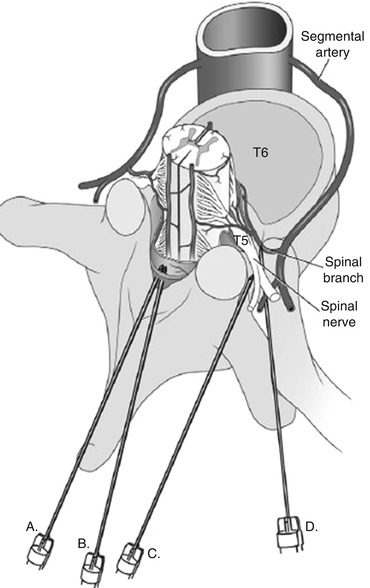
Fig. 11.1
Direct needle trauma from interlaminar and transforaminal approach . Needle A and B demonstrate a midline interlaminar approach which can directly traumatize the spinal cord. Needle C represents lateral deviation of the needle resulting in trauma to the spinal nerve, ventral or dorsal ramus. Needle D illustrates a transforaminal approach resulting in trauma to the spinal nerve, ventral or dorsal ramus, and spinal artery. Reprinted from Complications in Regional Anesthesia and Pain Medicine, Joseph M Neal, James P Rathmell, 2007, with permission Saunders/Elsevier
11.6 Clinical Presentation
Case reports illustrate the variability in the symptoms of direct needle trauma . Classic signs are severe pain, often correlating with the dermatomal pattern of the nerve contacted by the needle and radiating to one or more extremities, along with extremity paresthesia and weakness. Often, the symptoms manifest immediately upon needle penetration. There have been documented cases of fully awake patients, however, who sustained neuraxial injury but experienced no symptoms at the time of needle placement [16, 17]. Several factors influence clinical symptoms: cervical level, structure intruded (i.e., spinal cord or spinal nerve), and volume and type of injectate [18]. A higher cervical entry point may involve cranial nerves. One case report documented facial numbness after a C5–C6 interlaminar injection that was believed to be caused by direct damage to the spinal nucleus of the trigeminal nerve (which extends from the medulla to C3 or below C3) and by cephalad movement of intramedullary injectate [18].
The onset and quality of symptoms are also likely influenced by the structure that has sustained injury. Pain is more likely when extra-axial trauma affects the nerve roots or blood vessels, which are innervated by sensory neurons mediating pain [16]. On the other hand, there are no pain receptors within the spinal cord, which may render intra-axial lesions painless [16]. Pain is rarely reported with dural puncture, and symptoms may appear only after injection or from the sequelae of the needle trauma such as edema or hematoma [16].
11.7 Risk Factors
Risk factors for direct needle trauma are conditions that reduce or obscure the epidural space. Osteoporotic and degenerative processes of the spine, which become more common with advancing age, reduce the epidural space and close the intervertebral foramen [5]. Other pathologies that can compete with spinal cord and nerve roots for space are spinal stenosis, ligamentum flavum hypertrophy, and vertebral disc bulges [9, 18].
11.8 Preventative Measures
Numerous recommendations have been set forth to reduce the risk of direct needle trauma. Pre-procedural MRI or CT imaging is performed to verify adequate epidural space for needle placement at the target site [15]. Axial or sagittal cuts are measured to approximate dermal-to-epidural distance of the target interlaminar injection level, which can then be used to determine needle depth during the procedure [18]. Interlaminar CESI is performed at C7–T1 and preferably not higher than C6–C7 [15]. The cervical epidural space becomes narrower at higher cervical levels, increasing the likelihood of penetration of the dural sac and spinal cord [15]. At the C7–T1 level, medication can reach as high as the C4–C5 epidural space [18]. Low cervical targets reduce the risk of medication reaching the respiratory centers and cranial nerve nuclei in the medulla and upper cervical levels [18].
Radiographic guidance and the use of a test dose of contrast medium are essential for all CESI procedures. Interlaminar CESI should be performed under fluoroscopic guidance with anteroposterior, lateral, or contralateral oblique views to gauge the depth of needle insertion. Transforaminal CESI should be performed under fluoroscopy or digital subtraction angiography to decrease the risk of both direct needle trauma and intravascular injection [15]. The procedure should be stopped if a contrast test dose reveals a myelographic or arterial pattern [18]. A contrast pattern of a central canal stripe without flow to the lateral foramen may indicate cord injection [18].
Finally, the use of sedation during CESI continues to be debated. Those in favor of sedation point to case reports of needle trauma caused by sudden head movement, which would likely be prevented under sedation [19]. Those opposed to sedation argue that sedation could render a patient unable to report any pain or paresthesia caused by spinal cord or nerve trauma [19]. This position, however, is somewhat undermined by case reports, as described earlier, of fully awake patients reporting no unusual symptoms at the moment of traumatic needle penetration. The current consensus is to refrain from moderate-to-heavy sedation, and if light sedation is used, the patient should remain able to communicate pain or other adverse sensations or events [15].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






