BASICS
![]() Most commonly caused by assault or motor vehicle crash
Most commonly caused by assault or motor vehicle crash
SIGNS AND SYMPTOMS
![]() Malocclusion
Malocclusion
![]() Floor of mouth ecchymosis
Floor of mouth ecchymosis
![]() Lower lip/chin paresthesias
Lower lip/chin paresthesias
DIAGNOSTICS
![]() X-ray two views or Panorex view
X-ray two views or Panorex view
![]() Maxillofacial CT preferred
Maxillofacial CT preferred
TREATMENT
![]() Referral to Oral and Maxillofacial Surgery
Referral to Oral and Maxillofacial Surgery
![]() Prophylactic antibiotics: needed only if oral involvement (penicillin or first-generation cephalosporin, clindamycin)
Prophylactic antibiotics: needed only if oral involvement (penicillin or first-generation cephalosporin, clindamycin)
Maxillary Fracture (Midface Fracture)
BASICS
![]() Look for malocclusion
Look for malocclusion
![]() Nasal intubations and nasogastric tubes are contraindicated
Nasal intubations and nasogastric tubes are contraindicated
![]() Associated with significant traumatic mechanism
Associated with significant traumatic mechanism
DIAGNOSTICS
![]() Maxillofacial CT
Maxillofacial CT
![]() Le Fort fracture classification (Figure 17.1)
Le Fort fracture classification (Figure 17.1)
• Le Fort I: transverse, through the maxilla
• Le Fort II: extends superiorly involving the nasal bridge, maxilla, lacrimal bones, orbital floor, and rim
• Le Fort III: craniofacial dissociation; involves bridge of the nose and extends posteriorly along the medial wall and floor of the orbit, lateral orbital wall, zygomatic arch to the base of the sphenoid. May involve the cribriform plate; check for cerebrospinal fluid (CSF) leak
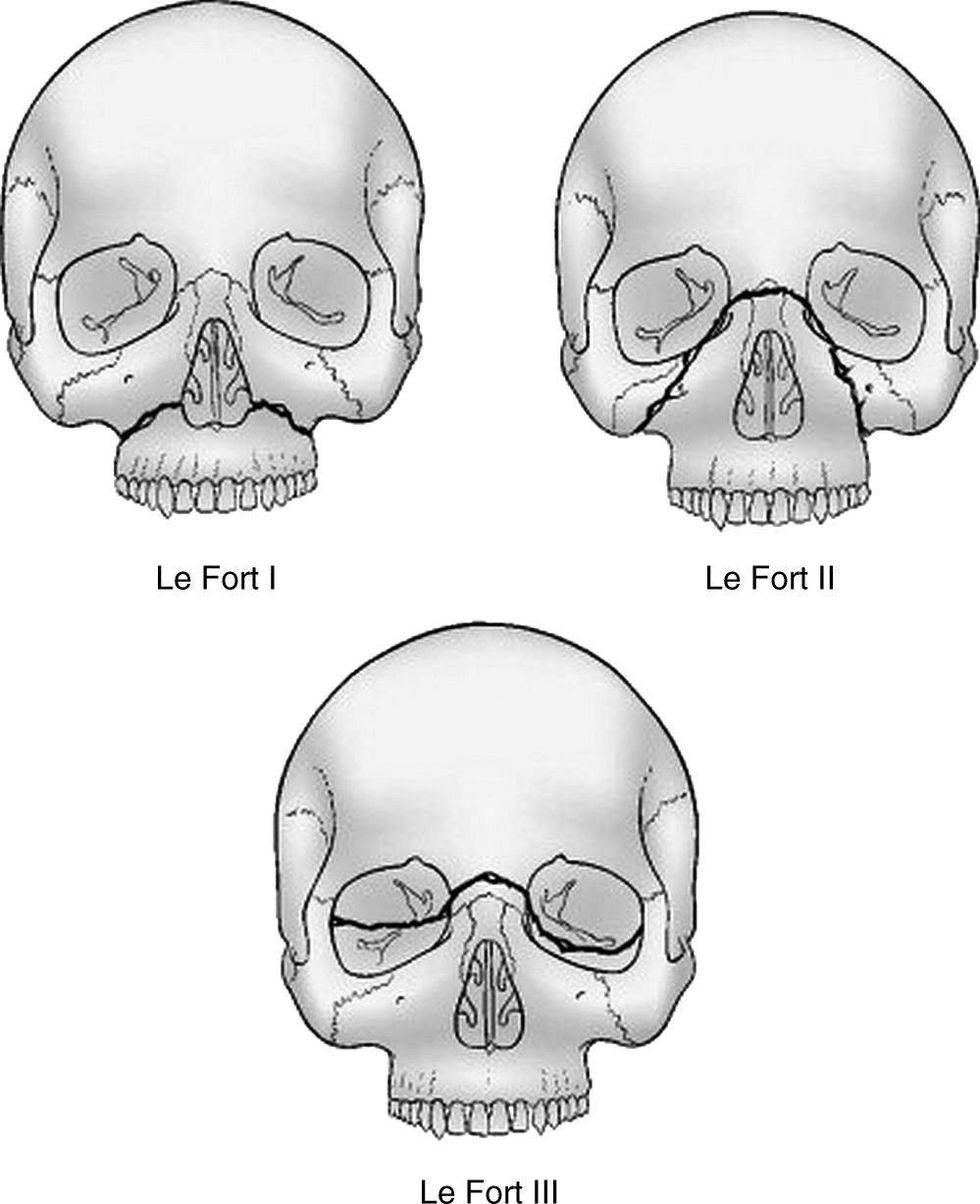
FIGURE 17.1. Le Fort fractures of the midface. (From Auerbach PS, ed. Wilderness Medicine. 6th ed. Philadelphia, PA: Elsevier Mosby; 2011. Figure 31-18 MD Consult. Redrawn from the American Association of Oral and Maxillofacial Surgeons. Oral and Maxillofacial Surgery Services in the Emergency Department. Rosemont, IL: American Association of Oral and Maxillofacial Surgeons; 1992, With permission.)
TREATMENT
![]() ABCs (airway, breathing, circulation), supportive, antibiotics
ABCs (airway, breathing, circulation), supportive, antibiotics
![]() Plastic surgery, Oral and Maxillofacial Surgery consults
Plastic surgery, Oral and Maxillofacial Surgery consults
![]() Neurosurgery consult for Le Fort III
Neurosurgery consult for Le Fort III
![]() Keep head of bed >30 degrees
Keep head of bed >30 degrees
BASICS
![]() Tripod fractures (infraorbital rim, zygomaticofacial and zygomaticotemporal suture lines)
Tripod fractures (infraorbital rim, zygomaticofacial and zygomaticotemporal suture lines)
DIAGNOSTICS
![]() Maxillofacial CT
Maxillofacial CT
TREATMENT
![]() ENT, plastics consult
ENT, plastics consult
![]() Delayed open reduction internal fixation
Delayed open reduction internal fixation
BASICS
![]() Most involve the orbital floor and medial wall
Most involve the orbital floor and medial wall
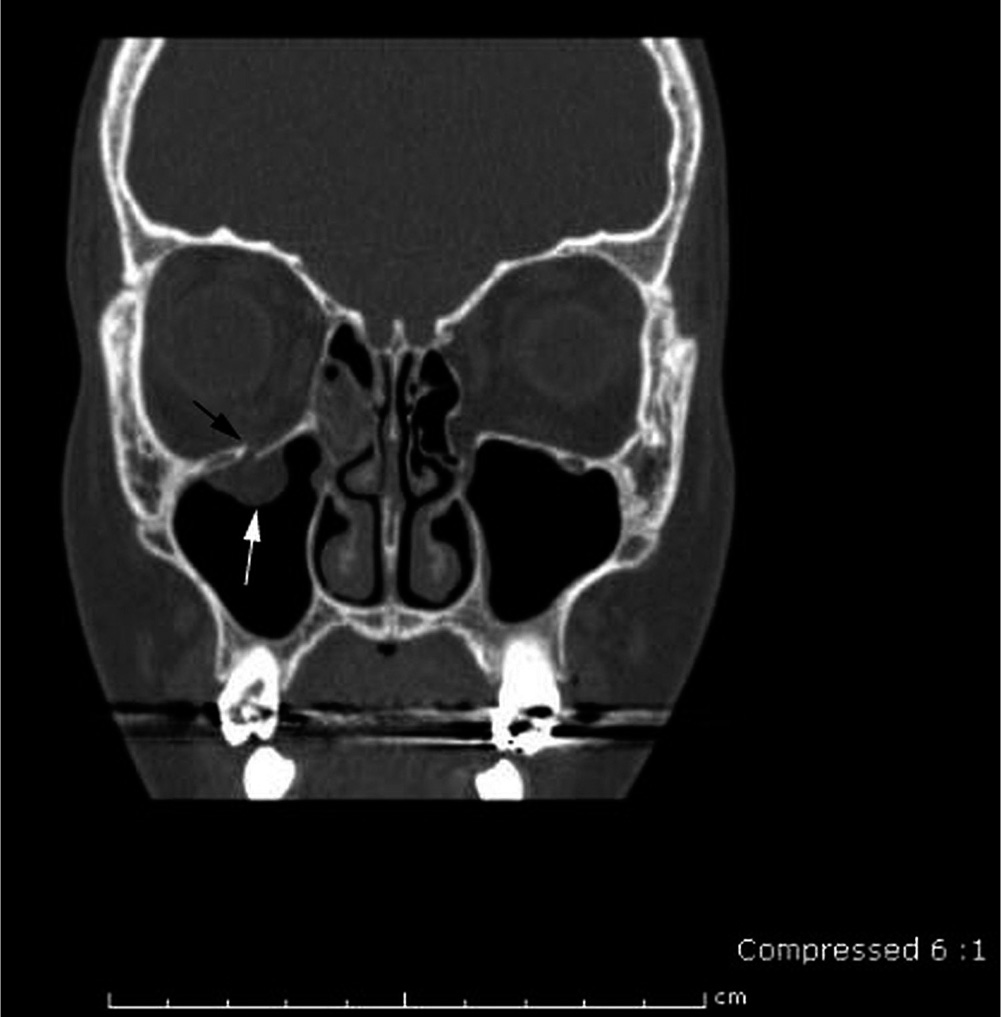
FIGURE 17.2. CT shows a right inferior orbital fracture (blowout fracture). (Neuman ML. Orbital fractures. In: Post TW, ed. UpToDate. Waltham, MA: UpToDate; 2014. Graphic 53238 Version 3.0. Courtesy of Mark Neuman, MD.)
SIGNS AND SYMPTOMS
![]() Periorbital swelling and tenderness
Periorbital swelling and tenderness
![]() Numbness over cheek
Numbness over cheek
![]() Can cause muscle and nerve entrapment
Can cause muscle and nerve entrapment
DIAGNOSTICS
![]() CT with clinical findings
CT with clinical findings
TREATMENT
![]() Surgery within 24 hours, unless there is too much edema, then within 5 to 7 days
Surgery within 24 hours, unless there is too much edema, then within 5 to 7 days
![]() Discharge with sinus precautions and Augmentin for 7 days or azithromycin
Discharge with sinus precautions and Augmentin for 7 days or azithromycin
![]() Blowout fracture (Figure 17.2)
Blowout fracture (Figure 17.2)
BASICS
![]() The most common fracture of the face
The most common fracture of the face
SIGNS AND SYMPTOMS
![]() Pain, history of trauma
Pain, history of trauma
![]() Nasal deformity
Nasal deformity
![]() Assess for septal hematoma: requires immediate evacuation to prevent necrosis
Assess for septal hematoma: requires immediate evacuation to prevent necrosis
DIAGNOSTICS
![]() Mostly clinical, can get x-ray
Mostly clinical, can get x-ray
TREATMENT
![]() Reduction in 5 to 7 days by plastics or ENT
Reduction in 5 to 7 days by plastics or ENT
BASICS
![]() Most fractures can be diagnosed with at least two-view x-rays; however, some need CT or MRI (especially elderly with continued pain)
Most fractures can be diagnosed with at least two-view x-rays; however, some need CT or MRI (especially elderly with continued pain)
![]() The neurovascular exam is essential on initial assessment and after splint placement; always document this
The neurovascular exam is essential on initial assessment and after splint placement; always document this
![]() Orthopedic consult should be considered for fractures that are open, intra-articular, unstable, require surgical repair, or with neurovascular compromise
Orthopedic consult should be considered for fractures that are open, intra-articular, unstable, require surgical repair, or with neurovascular compromise
![]() General treatment: pain control, elevation, immobilization, follow–up, and rehabilitation
General treatment: pain control, elevation, immobilization, follow–up, and rehabilitation
![]() Always examine joint above and below injury
Always examine joint above and below injury
![]() Bone anatomy (Figure 17.3)
Bone anatomy (Figure 17.3)
• Epiphysis: ends of a bone
• Physis: growth plate
• Metaphysis: upper and lower third of a bone
• Diaphysis: middle third of a bone
BASICS
![]() Anterior: most common, arm is externally rotated and slightly abducted
Anterior: most common, arm is externally rotated and slightly abducted
![]() Posterior: 2% to 4%, arm held in adduction and internal rotation
Posterior: 2% to 4%, arm held in adduction and internal rotation
![]() Inferior: 0.5%, arm held above the head, high risk for fracture and nerve damage
Inferior: 0.5%, arm held above the head, high risk for fracture and nerve damage
![]() Complications that need ortho referral
Complications that need ortho referral
• Humerus fracture
![]() Hill–Sachs deformity: humeral head cortical depression
Hill–Sachs deformity: humeral head cortical depression
![]() Bankart lesion: avulsion fracture
Bankart lesion: avulsion fracture
![]() Greater tuberosity fracture
Greater tuberosity fracture
• Axillary nerve: always test on exam for injury
DIAGNOSTICS
![]() X-ray pre- and postreduction
X-ray pre- and postreduction
![]() In some cases, there is no need for x-ray if the patient meets all of these criteria: age <40, atraumatic, and history of multiple shoulder dislocations
In some cases, there is no need for x-ray if the patient meets all of these criteria: age <40, atraumatic, and history of multiple shoulder dislocations
TREATMENT
![]() Reduction (many techniques)
Reduction (many techniques)
• Scapular manipulation, external rotation, traction-countertraction
![]() Immobilization with sling and swath
Immobilization with sling and swath
![]() Occasional surgery
Occasional surgery
Radial Ulna Fractures/Dislocation
BASICS
![]() Colles fracture: radial styloid fracture and distal radius fracture with dorsal displacement of the distal fragment
Colles fracture: radial styloid fracture and distal radius fracture with dorsal displacement of the distal fragment
![]() Smith fracture: distal radial fracture with palmar displacement
Smith fracture: distal radial fracture with palmar displacement
![]() Galeazzi: midshaft radius fracture with dislocation at the distal radioulnar joint
Galeazzi: midshaft radius fracture with dislocation at the distal radioulnar joint
![]() Monteggia: fracture at the junction of the proximal and middle thirds of the ulna, with an anterior dislocation of the radial head
Monteggia: fracture at the junction of the proximal and middle thirds of the ulna, with an anterior dislocation of the radial head
TREATMENT
![]() Reduce displaced fracture
Reduce displaced fracture
![]() Splint, ortho follow-up
Splint, ortho follow-up
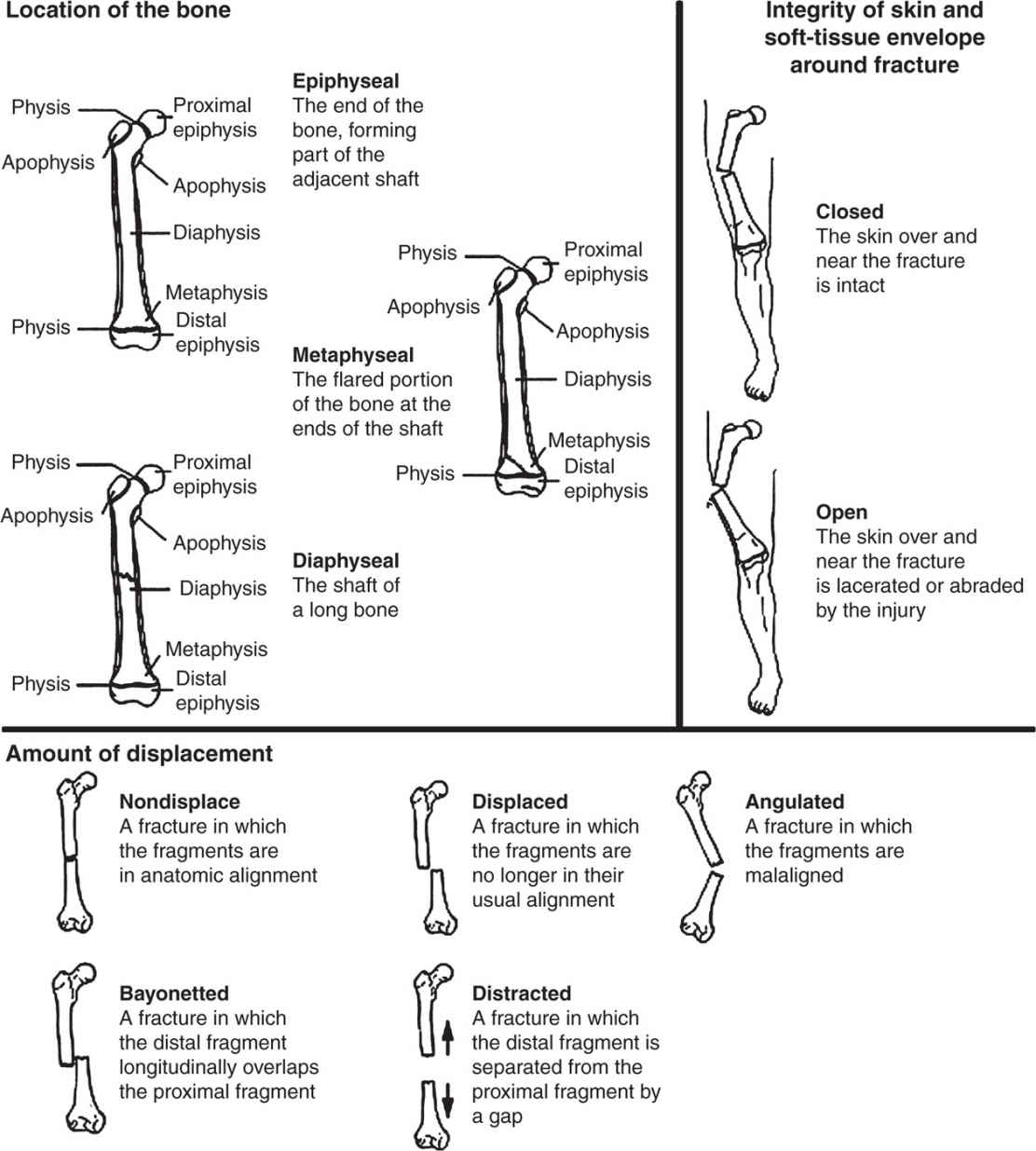
FIGURE 17.3. Bone anatomy and fracture classifications. (From Beutler A, Mark Stephens. General principles of fracture management: bone healing and fracture description. In: Post TW, ed. UpToDate. Waltham, MA: UpToDate; 2014. Graphic 56313 Version 2.0. Reproduced with permisiion from: Johnson TR, Steinback, LS. eds. Essentials of Musculoskeletal Imaging. Rosemonst, IL: Amercan Academy of Orthopedic Surgeons; 2004:40–41. Copyright 2004 American Academy of Orthopaedic Surgeons.)
DIAGNOSTICS
![]() X-ray:
X-ray:
• Anterior fat pad: can be normal, but if sail shape, always indicative of fracture
• Posterior fat pad: never normal, indicative of fracture
![]() In adults:
In adults:
• Assume radial head fracture if anterior sail shape or posterior fat pad (Figure 17.4)
![]() In children:
In children:
• Assume supracondylar fracture if anterior sail shape or posterior fat pad
TREATMENT
![]() Sling and ortho follow-up
Sling and ortho follow-up
BASICS
![]() Fifth metacarpal neck fracture, sometimes involves the fourth metacarpal
Fifth metacarpal neck fracture, sometimes involves the fourth metacarpal
![]() Mechanism is usually direct trauma to a clenched fist such as punching
Mechanism is usually direct trauma to a clenched fist such as punching
![]() Dorsal angulation of the fracture causes metacarpophalangeal joint depression (loss of the knuckle)
Dorsal angulation of the fracture causes metacarpophalangeal joint depression (loss of the knuckle)
DIAGNOSTICS
![]() X-ray
X-ray
TREATMENT
![]() May need reduction with a hematoma block
May need reduction with a hematoma block
![]() Ulnar gutter splint
Ulnar gutter splint
![]() Hand surgery follow-up
Hand surgery follow-up
![]() Complications
Complications
• Open fracture
![]() Antibiotics within 6 hours to prevent osteomyelitis (cefuroxime or fluoroquinolone, consider methicillin-resistant Staphylococcus aureus coverage)
Antibiotics within 6 hours to prevent osteomyelitis (cefuroxime or fluoroquinolone, consider methicillin-resistant Staphylococcus aureus coverage)
• “Fight bite”: skin tear near the metacarpal head from a tooth
![]() Irrigation, must give antibiotic coverage
Irrigation, must give antibiotic coverage
![]() First line: Augmentin
First line: Augmentin
![]() Second line: doxycycline, Bactrim, fluoroquinolone, cefuroxime, or penicillin plus Flagyl or clindamycin
Second line: doxycycline, Bactrim, fluoroquinolone, cefuroxime, or penicillin plus Flagyl or clindamycin
BASICS
![]() Mechanism is usually a fall onto an outstretched hand
Mechanism is usually a fall onto an outstretched hand
![]() Classified as distal, central, or proximal
Classified as distal, central, or proximal
![]() Tenderness at the radial, dorsal aspect of hand, anatomical snuff box
Tenderness at the radial, dorsal aspect of hand, anatomical snuff box
DIAGNOSTICS
![]() X-ray scaphoid views
X-ray scaphoid views
TREATMENT
![]() Thumb spica splint
Thumb spica splint
![]() If suspected, but x-ray is negative, still splint it!
If suspected, but x-ray is negative, still splint it!
BASICS
![]() Ulnar collateral ligament injury of the thumb
Ulnar collateral ligament injury of the thumb
![]() Caused by hyperextension
Caused by hyperextension
![]() Common in skiers, volley ball players, goalies
Common in skiers, volley ball players, goalies
TREATMENT
![]() Thumb spica splint
Thumb spica splint
BASICS
![]() From trauma or exertion, such as, coughing
From trauma or exertion, such as, coughing
![]() Ribs 1 to 3 associated with mediastinal injury (i.e., aorta)
Ribs 1 to 3 associated with mediastinal injury (i.e., aorta)
![]() Ribs 9 to 12 associated with intra-abdominal injury
Ribs 9 to 12 associated with intra-abdominal injury
![]() Flail chest
Flail chest
• Three or more consecutive ribs fractured in two or more places
• “Floating” segment, paradoxical movement on inspiration
![]() Complications
Complications
• Pneumonia
• Pneumothorax
• Hemothorax
• Respiratory failure
![]() More rib fractures = longer ventilation duration and increased mortality
More rib fractures = longer ventilation duration and increased mortality
DIAGNOSTICS
![]() Chest x-ray, ultrasound, CT
Chest x-ray, ultrasound, CT
TREATMENT
![]() Most heal in 6 weeks
Most heal in 6 weeks
![]() Less than three rib fractures: outpatient pain control, incentive spirometry
Less than three rib fractures: outpatient pain control, incentive spirometry
![]() Three or more rib fractures: inpatient, elderly with six or more admit to ICU, pain control, continuous pulse oximetry, multidisciplinary care
Three or more rib fractures: inpatient, elderly with six or more admit to ICU, pain control, continuous pulse oximetry, multidisciplinary care
BASICS
![]() Primary pneumothorax (PTX): occurs without a causing event or an underlying lung disease
Primary pneumothorax (PTX): occurs without a causing event or an underlying lung disease
• Risk factors: smoking, family history, Marfan syndrome
• Usually in early 20s to 30s
![]() Secondary PTX: occurs with an underlying lung disease
Secondary PTX: occurs with an underlying lung disease
• Risk factors: chronic obstructive pulmonary disease, cystic fibrosis, cancer, necrotizing pneumonia
![]() Traumatic PTX: may occur with a hemothorax
Traumatic PTX: may occur with a hemothorax
![]() Tension PTX: hypotension, tracheal deviation, elevated jugular venous pressure, requiring emergent needle decompression, and/or chest tube
Tension PTX: hypotension, tracheal deviation, elevated jugular venous pressure, requiring emergent needle decompression, and/or chest tube
SIGNS AND SYMPTOMS
![]() Shortness of breath, tachypnea, tachycardia, hypoxia, decreased breath sounds, subcutaneous emphysema; tracheal deviation is a late finding
Shortness of breath, tachypnea, tachycardia, hypoxia, decreased breath sounds, subcutaneous emphysema; tracheal deviation is a late finding
![]() Hemodynamic instability may indicate a tension PTX
Hemodynamic instability may indicate a tension PTX
DIAGNOSTICS
![]() Chest x-ray, ultrasound, CT
Chest x-ray, ultrasound, CT
TREATMENT
![]() Small (<15% volume): observation, high-flow O2 with non-rebreather face mask, repeated chest x-ray
Small (<15% volume): observation, high-flow O2 with non-rebreather face mask, repeated chest x-ray
![]() Large (2 cm on upright posterior to anterior chest x-ray equals a 50% PTX)
Large (2 cm on upright posterior to anterior chest x-ray equals a 50% PTX)
• Needle decompression (14G IV catheter into the pleural space at the second intercostal space, midclavicular line)
• Chest tube (see Chapter 18 for procedure details)
![]() VATS (video-assisted thoracoscopic surgery) pleurodesis
VATS (video-assisted thoracoscopic surgery) pleurodesis
![]() ABCs, supportive, smoking cessation education
ABCs, supportive, smoking cessation education
BASICS
![]() Benign to life-threatening
Benign to life-threatening
![]() Examine the genital and rectum for signs of open fracture
Examine the genital and rectum for signs of open fracture
![]() Always perform rectal exam before Foley placement
Always perform rectal exam before Foley placement
SIGNS AND SYMPTOMS
![]() Affected side: shortened, externally rotated, and abducted
Affected side: shortened, externally rotated, and abducted
![]() Presentation is pathognomonic
Presentation is pathognomonic
DIAGNOSTICS
![]() X-ray, CT (gold standard)
X-ray, CT (gold standard)
![]() Complications: urethral, vaginal, or rectal injuries
Complications: urethral, vaginal, or rectal injuries
TREATMENT
![]() ABCs, pain control, resuscitation
ABCs, pain control, resuscitation
![]() Pelvic binder, external fixation
Pelvic binder, external fixation
![]() Orthopedic consult for open reduction internal fixation
Orthopedic consult for open reduction internal fixation
BASICS
![]() Posterior: most common, leg flexed and adducted
Posterior: most common, leg flexed and adducted
![]() Anterior: leg abducted and externally rotated
Anterior: leg abducted and externally rotated
DIAGNOSTICS
![]() X-ray
X-ray
TREATMENT
![]() Reduction with postreduction films
Reduction with postreduction films
BASICS
![]() High-energy trauma
High-energy trauma
![]() High risk for hemorrhage
High risk for hemorrhage
DIAGNOSTICS
![]() X-ray
X-ray
TREATMENT
![]() ABCs, pain control, resuscitation
ABCs, pain control, resuscitation
![]() Immobilization and traction
Immobilization and traction
![]() Ortho consult for surgery
Ortho consult for surgery
BASICS
![]() Most commonly from a direct blow to the lateral knee
Most commonly from a direct blow to the lateral knee
![]() Seen often in pedestrian struck by vehicle
Seen often in pedestrian struck by vehicle
DIAGNOSIS
![]() X-ray
X-ray
TREATMENT
![]() Brace in extension, non-weight-bearing with crutches
Brace in extension, non-weight-bearing with crutches
![]() Ortho follow-up
Ortho follow-up
BASICS
![]() Anterior talofibular ligament is most common ligament injured in sprained ankle, from inversion injury
Anterior talofibular ligament is most common ligament injured in sprained ankle, from inversion injury
![]() Always examine knee looking for Maisonneuve fracture
Always examine knee looking for Maisonneuve fracture
• A spiral fracture of proximal fibula and medial malleolus associated with a tear of the distal tibiofibular syndesmosis
![]() Ottawa ankle rules: x-rays indicated if one of the following:
Ottawa ankle rules: x-rays indicated if one of the following:
• Tenderness over the medial or lateral malleolus
• Tenderness over the midfoot
• Tenderness over the base of the 5th metatarsal
• Unable to weight bear immediately and take four steps in the emergency department
DIAGNOSTICS
![]() X-ray
X-ray
TREATMENT
![]() Short-leg posterior splint or boot
Short-leg posterior splint or boot
![]() Ortho consult and surgery if unstable
Ortho consult and surgery if unstable
BASICS
![]() Jones: transverse fracture of the diaphyseal region of the base of the 5th metatarsal
Jones: transverse fracture of the diaphyseal region of the base of the 5th metatarsal
![]() Lisfranc: fracture/dislocation of the tarsometatarsal joint
Lisfranc: fracture/dislocation of the tarsometatarsal joint
![]() Caution: avulsion fracture of base of 5th metatarsal concerning for malunion given peroneus brevis ligament attachment site
Caution: avulsion fracture of base of 5th metatarsal concerning for malunion given peroneus brevis ligament attachment site
TREATMENT
![]() Most nondisplaced shaft fractures of metatarsal 2 to 5 do not require reduction or casting
Most nondisplaced shaft fractures of metatarsal 2 to 5 do not require reduction or casting
BASICS
![]() Usually caused by force during physical activities that involve sudden pivoting on a foot or rapid acceleration
Usually caused by force during physical activities that involve sudden pivoting on a foot or rapid acceleration
SIGNS AND SYMPTOMS
![]() Patient may describe feeling struck in the back of the ankle or hearing a “pop”
Patient may describe feeling struck in the back of the ankle or hearing a “pop”
![]() Severe acute pain when pushing off with his or her foot, although the absence of pain does not rule out rupture
Severe acute pain when pushing off with his or her foot, although the absence of pain does not rule out rupture
DIAGNOSTICS
![]() Do not assume rupture is absent because the patient can plantar flex or walk; 20% to 30% ruptures are missed because of this assumption
Do not assume rupture is absent because the patient can plantar flex or walk; 20% to 30% ruptures are missed because of this assumption
![]() Thompson test: the patient lies prone with his or her feet hanging off the end of the examination table, or kneels on a chair; clinician squeezes the gastrocnemius muscle belly while watching for plantar flexion; absence of plantar flexion when squeezing the gastrocnemius muscle marks a positive test = rupture
Thompson test: the patient lies prone with his or her feet hanging off the end of the examination table, or kneels on a chair; clinician squeezes the gastrocnemius muscle belly while watching for plantar flexion; absence of plantar flexion when squeezing the gastrocnemius muscle marks a positive test = rupture
![]() Clinical exam diagnosis
Clinical exam diagnosis
TREATMENT
![]() Complete tendon rupture: ice, rest, pain control, plantar flexion splint, crutches, non-weight-bearing
Complete tendon rupture: ice, rest, pain control, plantar flexion splint, crutches, non-weight-bearing
![]() Ortho consultation
Ortho consultation
![]() Partial tendon rupture: RICE (rest, ice, compression, elevation), 3 to 6 months of conservative treatment, if failed then ortho consultation
Partial tendon rupture: RICE (rest, ice, compression, elevation), 3 to 6 months of conservative treatment, if failed then ortho consultation
BASICS
![]() Increased pressure between muscle and fascia layers caused by bleeding or edema usually from trauma or burns
Increased pressure between muscle and fascia layers caused by bleeding or edema usually from trauma or burns
![]() Results in venous congestion and arterial insufficiency
Results in venous congestion and arterial insufficiency
![]() Late findings are associated with irreversible nerve and muscle damage
Late findings are associated with irreversible nerve and muscle damage
SIGNS AND SYMPTOMS
![]() Swelling with tight compartments
Swelling with tight compartments
![]() Pain out of proportion from exam (early)
Pain out of proportion from exam (early)
![]() Early signs: numbness, tingling, and paresthesias
Early signs: numbness, tingling, and paresthesias
![]() Late signs: loss of function, and decreased pulses or pulselessness
Late signs: loss of function, and decreased pulses or pulselessness
![]() 7 Ps:
7 Ps:
• Pain
• Pallor
• Paresthesia
• Paralysis
• Poikilothermia (inability to regulate temperature)
• Pulselessness
• Pressure
DIAGNOSTICS
![]() Handheld manometer (Stryker)
Handheld manometer (Stryker)
• Normal pressure is 0 to 8 mm Hg
TREATMENT
![]() Remove all splints/casts
Remove all splints/casts
![]() Do not elevate or lower the limb; it should be level with the heart
Do not elevate or lower the limb; it should be level with the heart
![]() Pain control, IV fluids, treat hypotension to reduce hypoperfusion
Pain control, IV fluids, treat hypotension to reduce hypoperfusion
![]() Emergent surgery consult for fasciotomy
Emergent surgery consult for fasciotomy
(see also Chapter 10, Nervous System Disorders)
BASICS
![]() Brain ischemia is caused by decrease in cerebral perfusion pressure
Brain ischemia is caused by decrease in cerebral perfusion pressure
![]() If intracranial pressure sharply increases, it can result in herniation
If intracranial pressure sharply increases, it can result in herniation
DIAGNOSTICS
![]() Decision to obtain head CT scan should be based upon Canadian or National Emergency X-Ray Utilization Study (NEXUS) II Head CT rules
Decision to obtain head CT scan should be based upon Canadian or National Emergency X-Ray Utilization Study (NEXUS) II Head CT rules
• Canadian CT Head Rule (consider CT if yes to any of the following):
![]() Glasgow Coma scale (GCS) <15 two hours after injury
Glasgow Coma scale (GCS) <15 two hours after injury
![]() Suspected open skull fracture
Suspected open skull fracture
![]() Sign of a basal skull fracture
Sign of a basal skull fracture
![]() Two or more episodes of vomiting
Two or more episodes of vomiting
![]() Age more than 65
Age more than 65
![]() Thirty minutes of preimpact amnesia
Thirty minutes of preimpact amnesia
![]() Dangerous mechanism
Dangerous mechanism
• NEXUS II CT Head Rule (consider CT if yes to any of the following):
![]() Evidence of skull fracture
Evidence of skull fracture
![]() Scalp hematoma
Scalp hematoma
![]() Neuro deficit
Neuro deficit
![]() Altered level of consciousness
Altered level of consciousness
![]() Abnormal behavior
Abnormal behavior
![]() Coagulopathy
Coagulopathy
![]() Persistent vomiting
Persistent vomiting
![]() Age more than 65
Age more than 65
![]() GCS
GCS
• GCS <8: severe head trauma
• GCS 9 to 13: moderate head trauma
• GCS 14 to 15: minor head trauma
![]() Eye opening
Eye opening
– 4 spontaneous
– 3 to verbal commands
– 2 to pain
– 1 no response
![]() Verbal response
Verbal response
– 5 oriented
– 4 confused
– 3 inappropriate
– 2 incomprehensible sounds
– 1 no response
![]() Motor response
Motor response
– 6 obeys commands
– 5 localizes to pain
– 4 flexion withdrawal
– 3 decorticate posturing
– 2 decerebrate posturing
– 1 no response
TREATMENT
![]() ABCs
ABCs
![]() Neurosurgery consult
Neurosurgery consult
![]() Keppra, Dilantin (seizure prevention)
Keppra, Dilantin (seizure prevention)
![]() Correct coagulopathy as indicated (fresh frozen plasma, platelet, vitamin K, profile 9)
Correct coagulopathy as indicated (fresh frozen plasma, platelet, vitamin K, profile 9)
![]() Goal systolic blood pressure <140
Goal systolic blood pressure <140
![]() Mannitol is sometimes used to decrease cerebral edema
Mannitol is sometimes used to decrease cerebral edema
![]() Uncal herniation
Uncal herniation
• Most common
• Ipsilateral uncus herniation compresses cranial nerve (CN) III
• Dilated ipsilateral pupil, ptosis, nonreactive pupil
![]() Central transtentorial herniation
Central transtentorial herniation
• Central biphasic herniation though tentorium caused by a lesion in the vertex or frontal lobe
• Signs: altered mental status, bilateral motor weakness, pinpoint pupils that eventually become dilated and nonreactive
![]() Cerebellotonsillar herniation
Cerebellotonsillar herniation
• Cerebellar tonsils herniate through the foramen magnum
• Signs: quadriplegia caused by compression of the corticospinal tracts, cardiopulmonary collapse from brainstem compression
![]() Subdural hematoma (SDH)
Subdural hematoma (SDH)
• Tearing of veins between the brain and dura occurring with acceleration-deceleration
• Risk factors: people with brain atrophy (elderly, alcoholics)
• CT: concave density adjacent to the skull, crosses suture lines
![]() Epidural hematoma (EDH)
Epidural hematoma (EDH)
• Bleeding between the dura and skull, usually from the middle meningeal artery
• Usually from direct trauma over the temporoparietal region
• CT: biconvex density adjacent to skull, does not cross suture lines
![]() Subarachnoid hemorrhage (SAH)
Subarachnoid hemorrhage (SAH)
• Most common abnormality seen on CT posttrauma
• CT: hyperdensity within subarachnoid space, prominent in the sulci or cerebral peduncles
• See SAH under Headache for more information
BASICS
![]() Most commonly involves the temporal bone
Most commonly involves the temporal bone
![]() High risk for intracranial hemorrhage
High risk for intracranial hemorrhage
SIGNS AND SYMPTOMS
![]() Battle sign: ecchymosis over the mastoid area
Battle sign: ecchymosis over the mastoid area
![]() Raccoon eyes: periorbital ecchymosis
Raccoon eyes: periorbital ecchymosis
DIAGNOSTICS
![]() Head CT
Head CT
COMPLICATIONS
![]() Temporal bone fracture
Temporal bone fracture
![]() Check for CSF leak, “halo” or “ring” test, risk for meningitis
Check for CSF leak, “halo” or “ring” test, risk for meningitis
![]() Dural tear (intracranial hemorrhage)
Dural tear (intracranial hemorrhage)
![]() CN palsies
CN palsies
TREATMENT
![]() Head of bed 60 degrees if concerned for CSF leak
Head of bed 60 degrees if concerned for CSF leak
![]() Admission for observation and consider neurosurgery consult
Admission for observation and consider neurosurgery consult
BASICS
![]() When in doubt, splint and follow up with orthopedics
When in doubt, splint and follow up with orthopedics
![]() May need sedation, consider ketamine
May need sedation, consider ketamine
![]() Current state and federal laws support the treatment of minors with an emergent medical condition, regardless of consent issues
Current state and federal laws support the treatment of minors with an emergent medical condition, regardless of consent issues
Salter–Harris Fracture Classification (Based on the Growth Plate)
![]() Type I: Separation at the physis
Type I: Separation at the physis
![]() Type II: Above, separation at the physis with partial metaphyseal fracture
Type II: Above, separation at the physis with partial metaphyseal fracture
![]() Type III: Lower, partial separation of the physis with intra-articular epiphyseal fracture
Type III: Lower, partial separation of the physis with intra-articular epiphyseal fracture
![]() Type IV: Through, intra-articular fracture extending across the physis into the metaphysis
Type IV: Through, intra-articular fracture extending across the physis into the metaphysis
![]() Type V: Everything Ruined, crush of the growth plate (Figure 17.5)
Type V: Everything Ruined, crush of the growth plate (Figure 17.5)
BASICS
![]() Most common pediatric fracture
Most common pediatric fracture
![]() Middle-third clavicle fracture: most common (80%), treat with a sling
Middle-third clavicle fracture: most common (80%), treat with a sling
![]() Distal-third clavicle fracture: sling, displaced fracture may require surgery
Distal-third clavicle fracture: sling, displaced fracture may require surgery
![]() Medial-third clavicle fracture: sling, displaced fracture needs ortho referral for reduction, consider intrathoracic injuries
Medial-third clavicle fracture: sling, displaced fracture needs ortho referral for reduction, consider intrathoracic injuries
DIAGNOSTICS
![]() X-ray
X-ray
TREATMENT
![]() Usually comfort measures, sling
Usually comfort measures, sling
![]() Rarely surgery
Rarely surgery
BASICS
![]() Radial head subluxation
Radial head subluxation
![]() Usually age 1 to 4
Usually age 1 to 4
![]() Mechanism is usually someone pulling on the child’s pronated forearm while the elbow is in extension, commonly while he or she is falling or pulling away
Mechanism is usually someone pulling on the child’s pronated forearm while the elbow is in extension, commonly while he or she is falling or pulling away
SIGNS AND SYMPTOMS
![]() Child not using his or her arm and holding it close to the body
Child not using his or her arm and holding it close to the body
![]() Pain with forearm supination
Pain with forearm supination
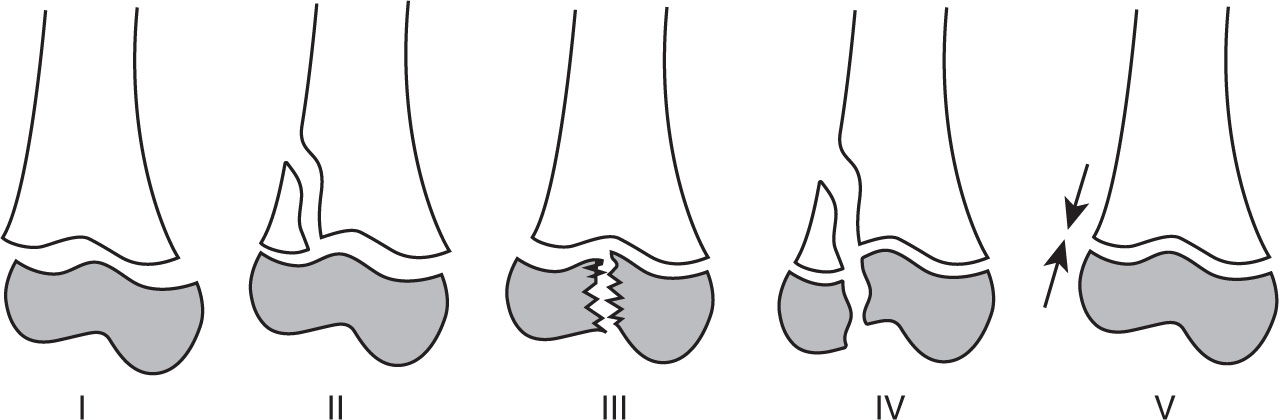
FIGURE 17.5. Salter–Harris fracture classification. (From Young SJ, Barnett PLJ, Oakley EA. Fractures and minor head injuries: minor injuries in children II. Med J Aust. 2005;182(12):644–648.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









