73 Traumatic Brain Injury (Adult)
• Emergency treatment of traumatic brain injury is aimed at rapidly identifying surgically correctable lesions and preventing secondary insults such as hypoxemia and hypotension.
• Triage to a neurosurgical trauma center is recommended for patients with intracerebral hemorrhage or persistent altered mental status.
• Early computed tomography is used to identify intracranial hemorrhage in patients with a significant mechanism of injury, history of altered mental status, or risk factors such as anticoagulant therapy.
• Osmotic agents such as mannitol or hypertonic saline are important first-line therapies for patients with elevated intracranial pressure.
• Hyperventilation should be avoided except as a temporizing measure in patients with impending herniation.
• A significant proportion of patients with mild head injury will have persistent postconcussive symptoms. All head-injured patients should be counseled about this possibility and be given appropriate outpatient referral.
• Athletes suffering from concussion should return to play only after completing a supervised stepwise rehabilitation program.
Pathophysiology
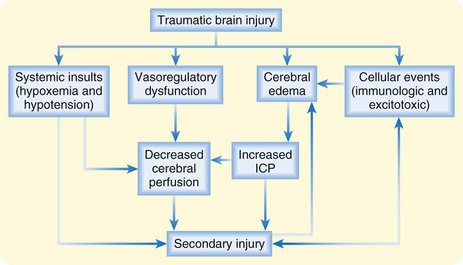
Hemorrhage or edema following TBI leads to rapid increases in intracranial pressure (ICP). Initially, cerebrospinal fluid (CSF) can be shunted out of the skull via the ventricles and cisterns. However, after severe TBI, this capacity is quickly overcome, and a rapid rise in ICP with compromised cerebral blood flow and cerebral ischemia ensues. Ultimately, the brain tissue itself may be forced downward across the rigid tentorium or out of the base of the skull itself, thereby resulting in a herniation syndrome and rapid death. Systemic hypoxia and hypotension occur with high frequency in patients with TBI and are associated with increased mortality (Fig. 73.1).
Differential Diagnosis and Medical Decision Making
Imaging
Non–contrast-enhanced computed tomography (CT) is the initial imaging study of choice in the evaluation of patients with TBI. Plain radiographs are neither sensitive nor specific in identifying intracranial lesions or skull fracture and are therefore not recommended as a diagnostic study. CT has excellent sensitivity in detecting the presence of intracranial hemorrhage, a mass effect such as ventricular compression or midline shift, and the presence of significant cerebral edema. CT also has the advantage of being widely available and rapid. See Box 73.1 for examples of CT findings in patients with TBI.
Box 73.1 Findings on Computed Tomography in Individuals with Traumatic Brain Injury
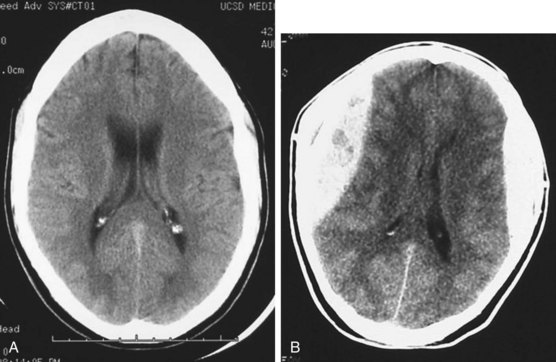
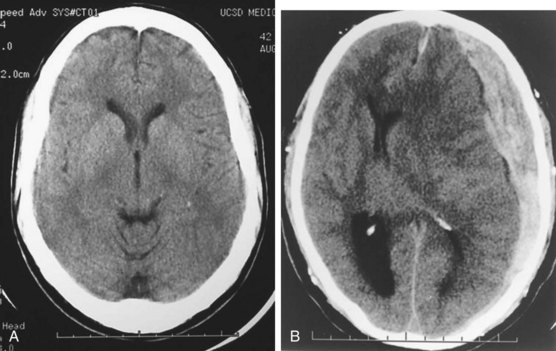
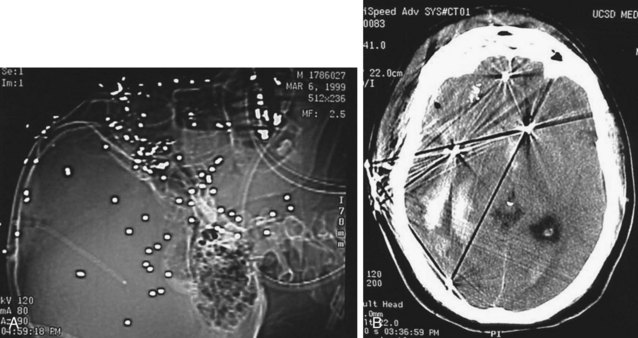
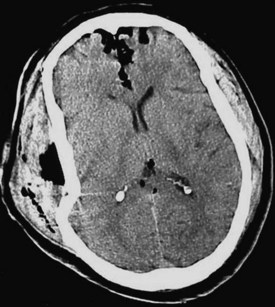
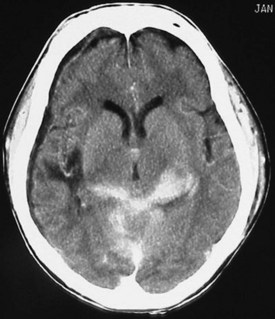
Acute hemorrhage appears hyperdense on computed tomography (CT) scans, with the shape and location of hemorrhage suggesting the underlying pathology. Epidural hematomas are classically lentiform (lens shaped) because of their relationship to arterial injury, with the higher pressure compressing the brain parenchyma (Fig. 73.2). Subdural hematomas are more commonly crescent shaped, with blood from torn veins tracking along the surface of the brain beneath the dura mater (Fig. 73.3). Intraparenchymal hemorrhage can exist as a discrete hematoma or as multiple smaller foci throughout a contused area of brain (Fig. 73.4). In addition to focal areas of hemorrhage, cerebral contusions typically involve cerebral edema, which may progress markedly over a period of several days. Skull fractures may be seen on plain radiographs, but more important is the potential for injury to the underlying brain parenchyma or the existence of intracranial hemorrhage (Fig. 73.5). Subarachnoid hemorrhage appears as hyperdensities within the ventricles, along the falx and tentorium, and around the circle of Willis (Fig. 73.6). One of the most elusive diagnoses is diffuse axonal injury, in which the findings on CT are often much less impressive than the degree of obtundation. Small, punctate hemorrhages along the gray-white interface at the cortical periphery suggest this diagnosis, although the initial scan may be completely normal.
Treatment
Prehospital Management
Half of all patients who die of TBI do so within the first few hours after their injury.
Prehospital assessment of patients with TBI should include rapid airway evaluation, continuous pulse oxygen saturation monitoring, frequent measurement of blood pressure, determination of GCS scores, and pupillary evaluation.1 Prehospital intubation should be avoided in patients who are spontaneously breathing and maintaining greater than 90% oxygen saturation.2 Prehospital airway management may be necessary in patients with a GCS score lower than 9 or those unable to maintain oxygen saturation greater than 90% with supplemental oxygen. If prehospital endotracheal intubation is performed, confirmation of placement should be done with auscultation and end-tidal capnography. Even mild hyperventilation should be avoided in all cases with the exception of patients who have evidence of herniation or acute neurologic deterioration. Hypotension should be treated with isotonic fluids, although protocols involving prehospital hypertonic saline administration are reasonable for patients with GCS scores lower than 9. Rapid transport is a priority, ideally to a facility with immediately available imaging and neurosurgical care.