INTRODUCTION AND EPIDEMIOLOGY
Assaults, motor vehicle crashes, falls, sports, and gunshot wounds account for the majority of facial fractures (in descending order of incidence), with motor vehicle crashes and gunshot wounds resulting in a higher severity of injury.1 The lack of a seat belt or airbag increases the risk of facial fractures and panfacial fracture.2 The most common fractures are to the nasal bone, followed by orbital floor, zygomaticomaxillary, maxillary sinuses, and mandibular ramus.1 Mechanisms and injury patterns vary with geography. In the urban setting, penetrating trauma and assaults result in midface and zygomatic fractures. In the rural setting, motor vehicle crashes and recreational injuries result in fractures of the mandible and nose. Males are more frequently affected than females, but domestic violence and elder and child abuse must always be considered in any patient presenting with facial trauma. The majority of abused women and children will have injuries to the head, face, and neck.3,4
PATHOPHYSIOLOGY
The facial skeleton is designed to create effective mastication. Vertical and horizontal buttresses are formed by bony arches joined at suture lines. Stronger vertical buttresses are formed by the zygomaticomaxillary buttress laterally and the frontal process of the maxilla medially. Weaker horizontal buttresses are formed by the superior orbital rims, orbital floor, and hard palate. The orbit itself is comprised of seven different bones, with the inferior and medial walls being particularly fragile. Therefore, frontal, lateral, and oblique forces often result in facial fractures.
The identification of facial injury and the restoration of normal appearance, sight, mastication, smell, and sensation are all essential tasks,5 but the principal focus should be on protecting the patient’s airway during the primary survey and the other initial considerations described in Table 259-1.
Primary survey
Secondary survey
History
|
Up to 44% of patients with severe maxillofacial trauma require endotracheal intubation due to mechanical disruption or massive hemorrhage into the airway.6 The incidence of associated injury to the brain, orbit, cervical spine, and lungs is directly related to the mechanism of injury and severity of facial fractures.6,7,8 Evaluate facial injuries as part of the secondary survey only after managing life-threatening injuries. Because up to 6% of patients with maxillofacial trauma will develop vision loss, a detailed eye examination is essential, especially in patients with high-energy mechanisms, orbital fractures, significant head injury, and abnormal pupillary findings.8,9
CLINICAL FEATURES
The mechanism of injury helps estimate the extent of injury. Exact details of motor vehicle crashes and assaults are often incomplete due to associated traumatic brain injury, intoxication, or other factors. Always address the possibility of abuse. When reported mechanisms do not match the injury, ask patients, especially women and the elderly, about interpersonal violence. Contact pediatricians and local child protective services when considering child abuse. It is better to report all suspected abuse than allow violence to continue and escalate. Obtain history of allergies, medications (especially cardiovascular and antithrombotic agents), comorbidities, tetanus immunization status, and time of last meal from the trauma patient or other available sources.
The secondary survey begins with three screening questions to help localize injuries while simultaneously examining the patient from the upper to the lower face. Important clinical findings in facial trauma are presented in Table 259-2.
History How is your vision? Do any parts of your face feel numb? Does your bite feel normal? Inspection Lateral view for dish face with Le Fort III fractures. Frontal view for donkey face with Le Fort II or III fractures. Bird’s eye view for exophthalmos with retrobulbar hematoma. Worm’s view for enophthalmos with blow-out fractures or flattening of malar prominence with zygomatic arch fractures. Raccoon eyes (bilateral orbital ecchymosis) and Battle’s sign (mastoid ecchymosis) typically develop over several hours, suggesting basilar skull fracture. Palpation Palpating the entire face will detect the majority of fractures. Intraoral palpation of the zygomatic arch, palpating lateral to posterior maxillary molars to distinguish bony from soft tissue injury. Assess for Le Fort fractures by gently rocking the hard palate with one hand while stabilizing the forehead with the other. Eye Examine early before swelling of lids, or use retractors. Document visual acuity. Systematically examine the eye from front to back. Specifically, check the pupil for teardrop sign pointing to globe rupture; hyphema; and swinging flashlight test for afferent papillary defect. Fat through wound indicates orbital septal perforation. Check intraocular pressure for evidence of orbital compartment syndrome only in absence of globe injury. Nose Crepitus over any facial sinus suggests sinus fracture. Nasal septal hematoma appears as blue, boggy swelling on nasal septum. Cerebrospinal fluid leak. Ears Auricular hematoma. Hemotympanum. Cerebrospinal fluid leak. Oral Jaw deviation due to mandible dislocation or condyle fracture. Malocclusion occurs in mandible, zygomatic, and Le Fort fractures. Missing or injured tooth. Lacerations and mucosal ecchymosis suggest mandible fracture. Place finger in external ear while the patient gently opens and closes jaw to detect condyle fractures. Tongue blade test: Patient without fracture can bite down on a tongue blade enough to break blade twisted by examiner. |
(1) How is your vision? Any patient with visual complaints or evidence of periorbital injury requires a thorough eye examination. (2) Is your face numb? Ask this question while checking for anesthesia of the forehead, lower eyelid, cheek and upper lip, or chin, suggesting injury to the supraorbital, infraorbital, or mental nerves. (3) Do your teeth fit together normally? Malocclusion typically occurs in patients with mandibular or maxillary fractures. Pain and tenderness near the ear indicate mandibular condyle injury. With zygomaticomaxillary complex fractures, patients often report pain over the cheek and trismus from masseter spasm or mechanical impingement of either the temporalis muscle or coronoid process of the mandible.
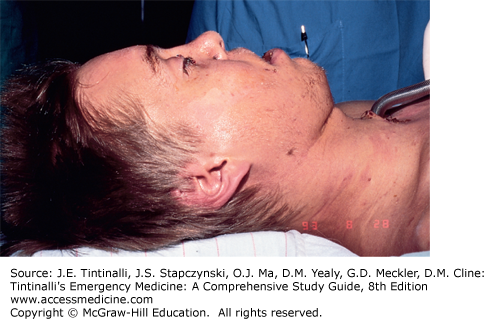
Inspect the face from the front, sides, feet, and above to detect subtle asymmetry in facial structure from zygomatic, orbital, and Le Fort injuries (Figures 259-1, 259-2 and 259-3). Palpate the entire orbital rim for tenderness and step-off deformities, which suggest fracture, and for crepitus, which suggests sinus involvement.
Examine the eyes before significant swelling occurs, or use lid retractors to better inspect the globe. Begin with corrected visual acuity using a wall, pocket, or phone app Snellen eye chart, name tag, or finger counting. In patients with loss of visual acuity, note light perception and color perception. Loss of vision implies injury to the optic nerve or globe. Subconjunctival hemorrhage and bloody chemosis occur with orbital fractures.
Assess extraocular motion and pupils. Binocular double vision suggests entrapment of the extraocular muscles, whereas monocular double vision suggests lens dislocation. Limitation on upward gaze occurs with fractures of the inferior and medial orbital wall from entrapment or injury to the inferior rectus, inferior oblique, or oculomotor nerve (Figure 259-4). Examine the pupils for shape, position, symmetry, and reactivity. Teardrop-shaped pupil indicates globe injury. Note the distance between the medial canthi; normal is the width of the patient’s globe. Telecanthus, widening of this distance with normal interpupillary distance, occurs with naso-orbito-ethmoid injuries. Widening of the interpupillary distance, or hypertelorism, results from a “blow-out” injury to the orbits, often resulting in blindness.
Check the swinging flashlight test for evidence of an afferent papillary defect (Marcus Gunn pupil) (see chapter 241, “Eye Emergencies”). With normal function, the swinging light results in brief dilation during movement followed by constriction when the light is directly over the eye. With injury to the optic nerve or retina, the affected pupil will not constrict until the light is again moved to the unaffected eye. The test is sensitive but not specific for optic nerve injury because an afferent papillary defect may result from pathology anywhere along the visual pathway.
Finish the physical examination of the eye by completing funduscopic, slit-lamp, and fluorescein examinations, as well as checking intraocular pressures when indicated. Flashes of light and floaters may be reported in patients with retinal detachments and vitreous hemorrhage. Foreign-body sensation and photophobia suggest corneal abrasions. Check for hyphema after having the patient sit upright for several minutes. In patients without evidence of globe rupture, check intraocular pressure in patients with significant exophthalmos, afferent nerve defects, or other evidence of retrobulbar hematoma.
Check carefully for globe injury with any penetrating injury to the periorbital area. Consult ophthalmology for suspected hyphema or vitreous hemorrhage. Fat herniating through the wound suggests an injury through the orbital septum. Through-and-through injuries, tarsal plate injuries, and injuries to the medial quadrant involving the lacrimal duct require repair by an ophthalmologist.
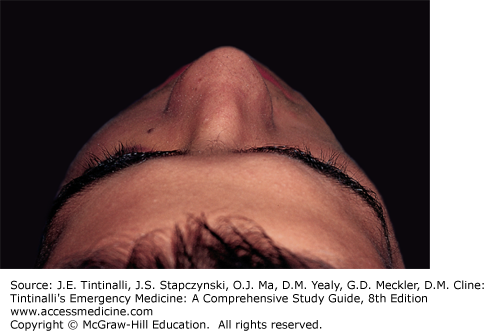
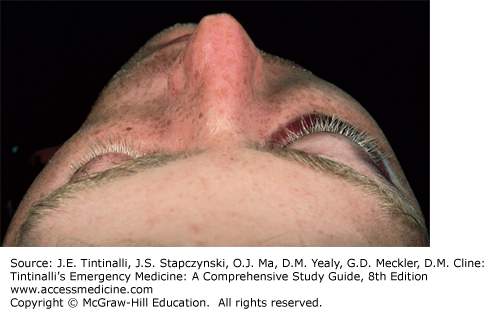
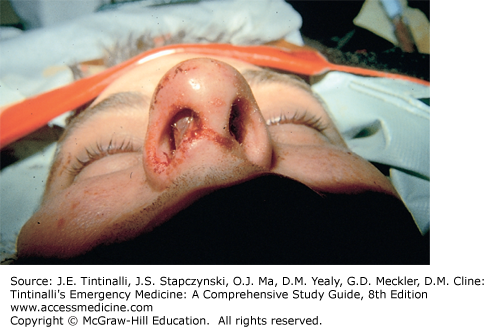
Begin the examination of the nose by checking for deformity from multiple angles while asking the patient about prior nose injury. Check for tenderness, crepitus, septal hematoma, and cerebrospinal fluid rhinorrhea. A septal hematoma appears as a blue, boggy, and tender area of swelling along the nasal septum (Figure 259-5). Incision and evacuation are required to prevent destruction of cartilage resulting in a saddle nose deformity. Ensure that simple nasal fractures are not associated with complex naso-orbito-ethmoid injuries. Perform the bimanual nasal palpation test with tenderness over the medial canthus. Begin by anesthetizing the nose. Then insert a cotton tip applicator inside the nose along the lateral nasal wall to the area behind the medial orbital wall and canthus. Palpate the area of the medial canthus externally with the opposite hand to check for movement from fracture of the medial wall of the orbit. Obtain a CT scan for suspected injury to the medial canthus or when telecanthus is present. Isolated nasal fractures and septal hematoma evacuation are reviewed in chapter 244, “Nose and Sinuses.”
Classic tests for cerebrospinal fluid rhinorrhea are not accurate in distinguishing cerebrospinal fluid from serous nasal discharge in the presence of nasal bleeding. The double ring or halo sign occurs when clear cerebrospinal fluid diffuses past blood when dropped on a paper towel. Trauma-related serous nasal discharge will also diffuse past blood. The glucose test is likewise not reliable. Nasal discharge does not contain glucose, whereas cerebrospinal fluid does. Bleeding may create a false-positive glucose test.
Begin the inspection of the ear by checking the mastoid process for Battle’s sign (suggesting a basilar skull fracture) and the ear for auricular hematoma. Incision and drainage are required to prevent destruction of cartilage resulting in a cauliflower deformity. Traumatic injury to the ear, including auricular hematoma evacuation, is reviewed in chapter 242, “Ear Disorders.” Check the external auditory canal for lacerations, cerebrospinal fluid leak (temporal bone or middle cranial fossa injury), and hematotympanum (a purple and often bulging tympanic membrane). Insert a finger into the external auditory canal and ask the patient to gently open and close the mouth to check for a mandibular condyle fracture.
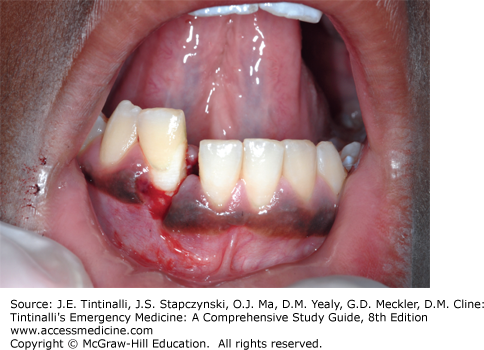
Inspect the jaw for deviation resulting from a fracture or dislocation. Malocclusion occurs in mandibular fractures, Le Fort fractures, and zygomatic fractures. Check the mouth carefully for missing or subluxed teeth, fractures of the alveolar ridge, sublingual hematoma, or breaks in the oral mucosa (Figure 259-6). Be sure to inspect the tongue for lacerations that may result in significant swelling later on. The tongue blade test has been reported to be 96% sensitive in identifying clinically significant mandibular fracture injuries in facial trauma patients.10,11,12 The patient without a mandible fracture bites down forcefully enough on a tongue blade to allow the physician to snap the tongue blade with a twisting motion. Patients who open the mouth and cannot break the blade require further imaging. The tongue blade test is best used in conjunction with other clinical findings because test sensitivity may be as low as 85%.12
DIAGNOSIS
Noncontrast CT is the imaging modality of choice. Plain radiographs remain helpful when CT is not available or to exclude injury in the low-risk patient. Recommendations for imaging based on level of injury and clinical findings are summarized in Table 259-3.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree