
Trauma Airway Management
Timothy J. Fortuna and John H. Burton
Expertise in airway management is an essential skill for the emergency physician (EP), and this is especially true of airway management in patients with multisystem trauma. Many trauma patients benefit from early control of the airway to ensure adequate oxygenation and ventilation and to protect against aspiration.
There are many special considerations to take into account when faced with controlling and maintaining an adequate airway in the trauma patient; some are listed in Table 19.1. The EP should assume the presence of cervical spine injury in most victims of blunt trauma. Owing to the common occurrence of altered mental status and hemodynamic instability, as well as the difficulty of rapidly obtaining adequate cervical spine imaging, cervical spine injury cannot typically be excluded in many trauma patients who require emergent intubation.
TABLE 19.1
Factors Complicating Trauma Airway Management
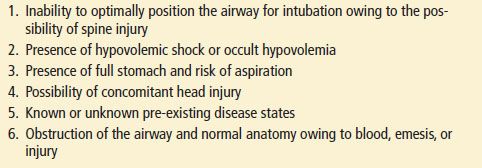
There are many methods for predicting the difficulty of intubation in a patient (see Chapter 1). Though these are helpful as a structured approach to airway management, their application in the trauma patient is frequently limited. Coexisting facial and penetrating neck trauma may exacerbate the challenge of both the assessment and visualization of the airway. The inability to optimally position the airway in the trauma patient can be problematic for adequate laryngeal visualization during intubation.
All trauma patients should be assumed to have hypovolemia or compensated shock. Therefore, caution must be used when choosing medications to facilitate airway management to avoid hemodynamic compromise. Trauma patients should also be presumed to have a full stomach. This places the trauma patient at an elevated risk for aspiration during the initial assessment and airway interventions. Patients immobilized by cervical collar and long spine board are not always able to fully protect their airways.
Concomitant head injury alters the approach to airway management in the trauma patient. Adequate cerebral perfusion pressure should be maintained in these patients and the consequence of potentially increased intracranial pressure (ICP) should be considered for all interventions. Drugs or alcohol, which may cause altered mental status and combative behavior, complicate the determination of the presence of closed head injury and the need for emergent airway management.
INDICATIONS FOR AIRWAY MANAGEMENT IN THE TRAUMA PATIENT
The most common reasons for deciding to perform endotracheal intubation (ETI) in the acutely injured patient are for oxygenation, ventilation, and airway protection. Severe chest and pulmonary injuries, hemorrhage, traumatic brain injury, and airway obstruction may lead to the inability of trauma patients to adequately oxygenate or ventilate. Protective airway reflexes may be impaired due to depressed mental status from traumatic brain injury, severe alcohol intoxication, and upper airway trauma. Trauma patients are often combative and resistant to calming techniques as well as physical and chemical restraints. These patients may benefit from intubation in these circumstances to expedite their evaluation. The increasing frequency of elderly trauma patients, who commonly have comorbidities, may provoke the clinician to consider early airway interventions to facilitate both the assessment and treatment of their traumatic injuries.
TECHNIQUES OF AIRWAY MANAGEMENT
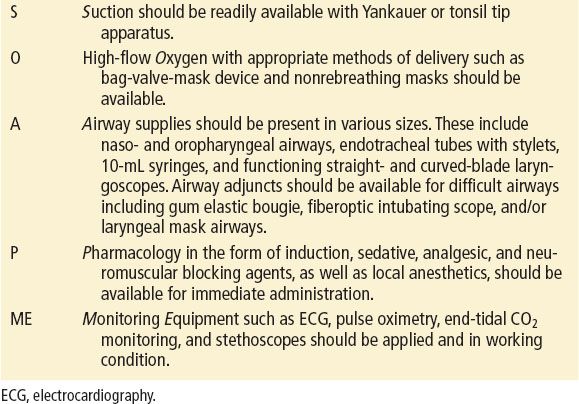
Orotracheal intubation (OTI), video-assisted intubation (VAI), blind nasotracheal intubation (NTI), and surgical cricothyrotomy are choices for definitive airway management in the trauma patient. Proper preparation is essential in the anticipation and execution of all airway interventions. The use of the mnemonic SOAPME may be helpful to ensure readiness (eTable 19.1).
eTABLE 19.1
Preparation for Airway Management: Mnemonic
Orotracheal Intubation and Rapid Sequence Induction
OTI may be performed in several ways, ranging from having the patient totally awake to performing OTI in conjunction with rapid sequence induction (RSI). OTI with RSI is the preferred approach to the airway management of the majority of patients with traumatic injuries. Although different pharmacologic agents may be chosen for neuromuscular blockade and induction, the major components of this intervention include preoxygenation, administration of agents that cause loss of consciousness (induction), administration of paralytics (neuromuscular blockade), and administration of postintubation analgesia and sedation.
Preoxygenation is performed to maintain hemoglobin saturation during airway management. Desaturations below 70% put patients at risk for dysrhythmia, hemodynamic decompensation, hypoxic brain injury, and death. Preoxygenation is achieved either actively or passively. A logistic flow of preoxygenation to prevent desaturation is shown in eFigure 19.1 (7).
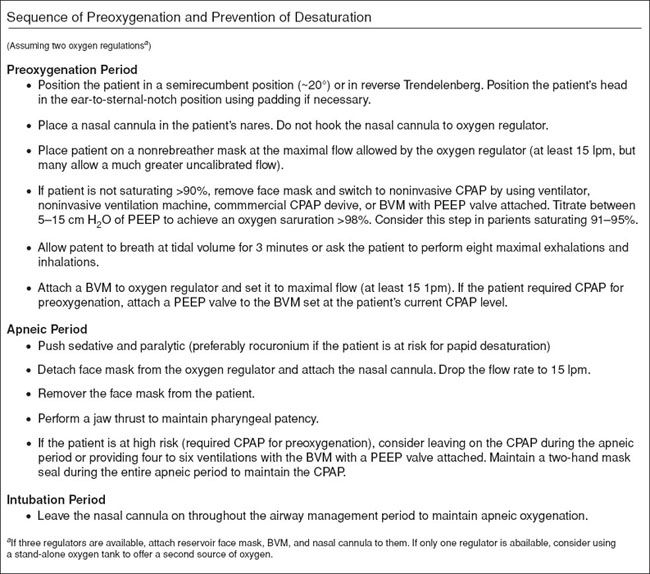
eFIGURE 19.1 Logistic flow of preoxygenation and prevention of desaturation. (From Weingart SD, Levitan MD. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012;59:165–175, with permission.)
A standard reservoir facemask with the oxygen flow rate set as high as possible is the recommended source of high FiO2 in the emergency department (ED). A passive approach will allow for spontaneous respirations through this nonrebreather facemask.
Active preoxygenation techniques should be considered for patients who cannot achieve greater than 95% oxygen saturation even with high FiO2 delivered passively. The risk categorization of patients during preoxygenation and the means by which oxygen should be applied is shown in eTable 19.2 (7). Active techniques for oxygenation include the use of continuous positive airway pressure (CPAP) masks, noninvasive positive-pressure ventilation, or positive end-expiratory pressure (PEEP) valves on a bag-valve mask (BVM). Optimal application of a BVM for the purposes of oxygenation and ventilation in the trauma patient typically requires two medical providers: one to ensure a proper mask-to-patient seal and one to manage bag compression.
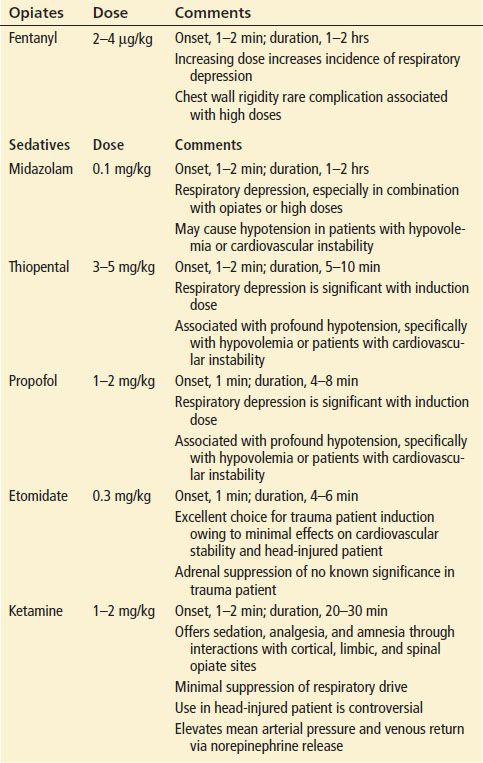
TABLE 19.2
Selected Pharmacologic Agents for Use During Trauma Airway Management
eTABLE 19.2
Risk Categorization of Patients During Preoxygenation
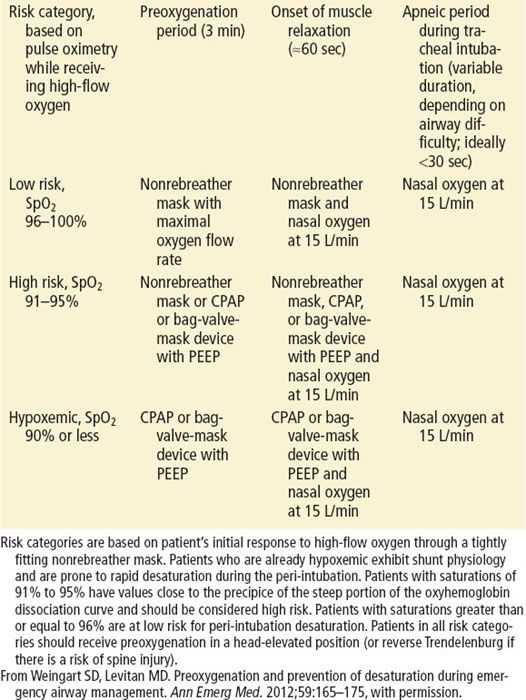
Apneic oxygenation is also a key component of adequate preoxygenation. When high flow oxygen (15 L/min) is delivered through a nasal cannula after induction and during the apneic period patients can maintain oxygen saturations of more than 98% for 18 to 55 minutes (5).
Difficulty in providing maximal preoxygenation may occur in patients with chest trauma or those with bronchospasm from pre-existing reactive airway disease or from smoke inhalation. In cases where pneumothorax is strongly suspected, consideration should be given to delaying intubation and mechanical ventilation until after performance of tube or needle thoracostomy. Artificial ventilation can result in rapid progression of a simple pneumothorax to a tension pneumothorax, even with a brief period of mechanical ventilation.
Neuromuscular blockade is performed during RSI for a number of reasons. Muscular paralysis reduces the aspiration risk by eliminating the gag and cough response to laryngoscopy. Paralysis also effectively relaxes the upper airway musculature to allow for an optimal view of the larynx. It prevents patient movements that might complicate efforts to visualize the airway during intubation. Caution should be exercised in the use of paralytic agents if difficulty ventilating the patient via BVM is anticipated.
Rescue airway adjuncts, as well as cricothyrotomy equipment, must be immediately available at all times during RSI of trauma patients. In cases where a difficult airway is anticipated, a modified approach may be used to provide adequate sedation or anesthesia to allow for airway intervention without the use of neuromuscular blocking agents.
Video-Assisted Intubation
Video-assisted devices are becoming more commonplace in EDs, particularly in the training environment. There have been many studies to date that have shown users obtain better laryngeal visualization and have a higher first-pass success rate in the difficult airway patient (6). There are many commercially available video laryngoscopes and all require some added training. Even in the hands of novice video laryngoscopy improves visualization and visual confirmation of proper tube placement (eFig. 19.2). Intubation can be performed by passing a tube over a flexible fiberoptic scope while visualizing the vocal cords or using a rigid video laryngoscope, such as the Glidescope or Storz video system. The same principles of RSI apply when using a video device.
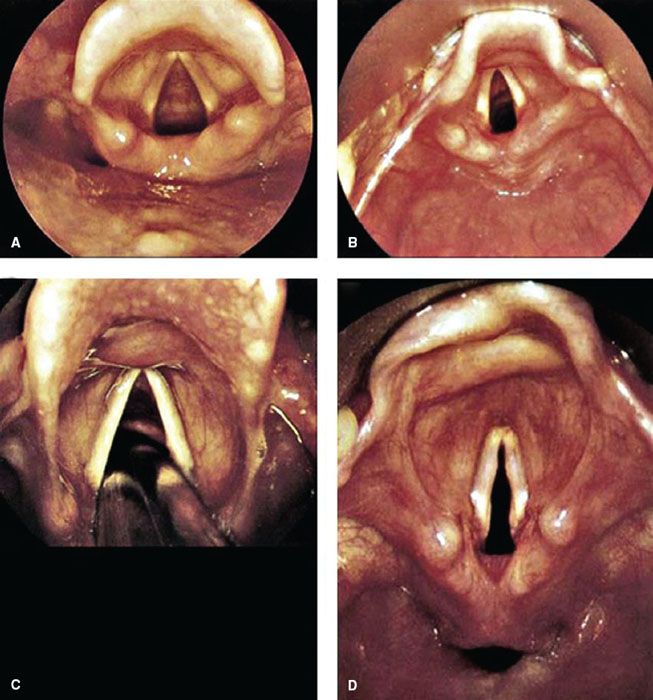
eFIGURE 19.2 Larynx appearance with videolaryngoscope. A: Preintubation view of an adult airway. B: Preintubation view of a pediatric airway. C: ETT passing between the vocal cords. D: The larynx and hypopharynx (note the horizontally oriented space below the laryngeal inlet, which is the esophagus). (From Nagdev A. Airway, breathing, circulation: Normal airway. In: Greenberg MI, Hendrickson RG, Silverberg M, et al., eds. Greenberg’s Text-atlas of Emergency Medicine. Philadelphia, PA: Lippincott Williams & Wilkins; 2004, with permission.)
The utility of the video-assisted device is limited in certain trauma situations particularly when visualization is impaired by blood, vomit, secretions, or direct trauma to the airway. As with any intubation attempt proper preparation should include having backup plans for failed attempts, this includes the ability to perform direct laryngoscopy and the tools for a surgical airway.
Blind Nasotracheal Intubation
NTI has several drawbacks and few advantages when compared to other techniques that are readily available for emergency airway management. Nasotracheal intubation requires a clinician who is experienced in the technique, a cooperative patient who is spontaneously breathing, and proper preparation of the nasal mucosa. This technique has largely fallen out of favor because it is more time consuming, has a larger failure rate, a higher complication rate, and requires a smaller tube size than other techniques. Despite these drawbacks NTI is still an important skill because it may be useful in certain situations such as limited mouth opening or severe oral trauma. The safety of NTI in patients with significant midface trauma has been suggested in clinical experience and the literature (13).
If NTI is attempted, oxygen should be administered by high-flow delivery throughout the procedure to improve oxygenation. The larger nostril should be chosen for placement of the endotracheal tube. The nasal mucosa should be prepared using a topical anesthetic and vasoconstrictive agent such as 4% lidocaine and 1% phenylephrine. Mild or moderate sedation may improve patient cooperation and decrease patient movement. Endotracheal tubes specifically designed for NTI are helpful as well, including tubes in which the tip can be manipulated anteriorly by a proximal trigger, thus enhancing the success of tracheal placement.
Surgical Airway Management
Cricothyrotomy equipment should be immediately available for any trauma patient undergoing emergent airway interventions, including RSI. The major indication for cricothyrotomy is failure of other methods of intubation with the simultaneous inability to ventilate and oxygenate the patient via BVM. Many cricothyrotomies involve patients with significant facial trauma or upper airway hemorrhage.
Patients with anterior neck trauma (penetrating and blunt) deserve particular consideration since they have a relative contraindication to cricothyrotomy. In addition, there will always be a small percentage of patients whose oral anatomy or body habitus renders intubation by any means very difficult and limits the feasibility of using airway adjuncts for more than a very limited amount of time. Perhaps the greatest mistake regarding the use of cricothyrotomy is its timing, as it is frequently used too late in the course of management when the patient is already severely hypoxemic.
Special Maneuvers and Intubation Adjuncts
Displacement of the thyroid cartilage Backward against the cervical vertebrae, Upward or as superiorly as possible, and laterally to the Right (the BURP maneuver) has been described and demonstrated to improve the view of the glottis during laryngoscopy (eFig. 19.3) (22). The mechanism by which BURP improves visibility may lie in the ability to move the glottis into the line of vision given that laryngoscopy tends to push the tongue and possibly the larynx toward the left. Application of the BURP maneuver may require a third provider in addition to the laryngoscopist and individual holding inline stabilization of the neck.
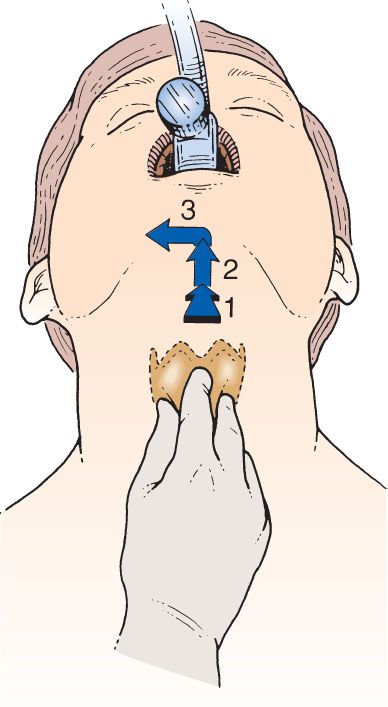
eFIGURE 19.3 Diagram of application of the BURP maneuver to improve the glottic view during laryngoscopy. The thyroid cartilage is moved Backward against the cervical vertebrae, Upward or as superiorly as possible, and laterally to the Right.









