Fig. 36.1
Square off end plates of the desired level to be injected (in this case, L3). Fluoroscope is rotated oblique 20–35° to obtain the “foraminal” view. Local anesthetic is injected via a 25 gauge needle as shown in the figure
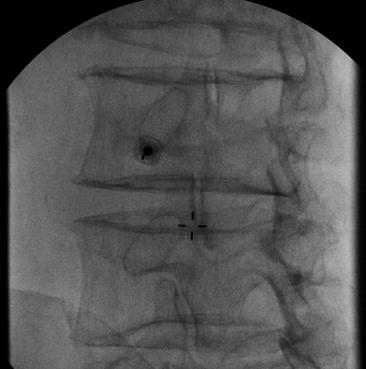
Fig. 36.2
A spinal needle is placed sub-pedicular, outer edge of the pedicle. Note the coaxial view of the needle where the hub is over the tip of the needle in the oblique plane of the fluoroscope

Fig. 36.3
The fluoroscope is rotated back to anteroposterior view and the needle tip is located at the outer edge of the foramen

Fig. 36.4
Reverse oblique view is taken and the needle tip has not yet entered the foramen
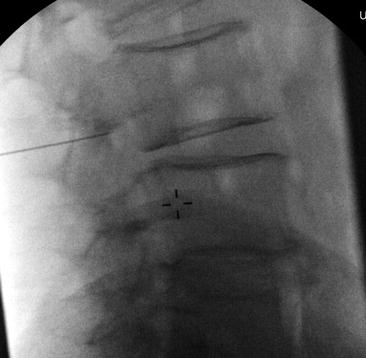
Fig. 36.5
Lateral view with needle seen at the posterior edge of the foramen, just under the pedicle. For more of an epidural injection, the needle would be advance to the anterior portion of the foramen. For the selective nerve root, the final position of the needle tip should be dependent upon the outline of the nerve with the injection of the iodinated contrast

Fig. 36.6
Injection of 2 mL of iodinated contrast outlining the L3 nerve root without any vascular or cerebrospinal fluid uptake. The contrast can be seen proximally in the spine as well as extra foraminally
For the lumbar spine below the L2 level, some experienced practitioners will typically utilize particulate steroids based mostly on anecdotal experience (this writer included). However, above the L2 level, it makes more sense to use water-soluble steroids because of the risk of catastrophic complications, which will be discussed in the next section [19]. To account for the higher risk of injury above the L2 vertebral level, mostly stemming from vascular penetration, the use of digital subtraction angiography can be added to confirm safe needle placement without vascular uptake. If vascular penetration occurs, the needle should be repositioned and repeat angiography should be performed. If vascular uptake is shown twice, especially in the cervical spine, the procedure should be aborted [19].
Complications
Relative to the number of procedures reported, the risk of complications remains very low. Short-term complications include bruising at the injection site, possible site-related pain, numbness in the distribution of the nerve being blocked, and sometimes neuritis, which can cause more pain temporarily after the procedure. Most of these complications are transient.
Catastrophic complications have also been described [20–25]. Therefore, the procedure should only be performed by those who have completed proper training. Complications are often related to the failure to recognize abnormal needle placement, failure to abort a procedure in the setting of patient intolerance, vascular penetration of the needle, and excessive sedation whereby the patient cannot respond. Depending on the location in the spine, vascular penetration has a relatively high incidence (11–19%); thus, recognition is paramount to procedural safety [26]. The use of particulate steroid has also been implicated as the cause of the spinal cord injury in the setting of vascular uptake. Nevertheless, even though vascular penetration occurs frequently, clinical sequelae are uncommon. In many settings, severe central, foraminal, or lateral recess stenosis is present; thereby, it is imperative to have the patient awake and responsive during the procedure as many catastrophic complications such as permanent nerve damage have been reported in this setting, most likely related to severe nerve ischemia.
Evidence
There is a paucity of “level 1” evidence for the use of SNRB/TFESI for both diagnostic and therapeutic purposes. Level 1 implies randomized, prospective, double-blinded, placebo controlled outcome studies. Because pain is such a subjective experience, with a significant amount of patient-to-patient variability, it is a difficult measure to standardize. As such, most studies will include outcomes based on more objective measures such as ODI, quality of life measures, and avoidance of surgery. Since epidural steroid injections are performed so frequently, there are a plethora of opinions regarding their utility and place in the overall management of pain. SNRB/TFESIs frequently get grouped into all spinal interventions when meta-analyses are done, which includes interlaminar and caudal epidural steroid injections.
Recently, Chou et al. published a review in the Annals of Internal Medicine, which essentially concluded that there is no evidence to support the use of epidural steroid injections for the management of pain related to disk herniations [27]. This contradicts many studies published in both pain management and rehabilitation medicine journals [28–32]. Most of the specialty-specific articles agree that these procedures do work for the management of pain related to disk herniation s . There is more uncertainty as to how to perform them (interlaminar, caudal, or transforaminal), when to perform them, and how frequently they can or should be performed. Since the majority of these procedures are performed in the lumbar spine, the majority of the literature is relative to blocks performed in this region. There are retrospective reports of success in the cervical spine, which have been recently published by the Cleveland Clinic [33].
Conclusion
SNRB/TFESIs are a useful adjunct in the diagnosis and treatment of painful spinal conditions as outlined earlier. As with most procedures in medicine, success is related to patient selection as well as the use of a comprehensive management approach. Improvement in ODI, quality of life measures, and participation in a rehabilitation program are methods to monitor progress of patients with pain. A thorough evaluation of the patient should be performed prior to the procedure, ideally including an MRI unless contraindicated.
Image guidance should be utilized for all procedures. While fluoroscopy is the most frequently utilized, recent advances in ultrasound position it as potentially useful as well. The technique has to be adjusted in the setting of severe spine degeneration. Recognition of proper needle placement and more importantly improper needle placement are important to prevent catastrophic complications such as spinal cord injury. The risk of catastrophic complications is extremely low relative to surgery, assuming the patient has a normal coagulation status, there is absence of systemic or local infection, and proper technique is utilized. There is evidence to support the use of this procedure for the management of spine-related pain, and the potential benefit significantly outweighs the potential risk.
References
1.
Manchikanti L. Transforaminal lumbar epidural steroid injections. Pain Physician. 2000;3:374–98.PubMed
2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





