Chapter 14
Transcutaneous electrical nerve stimulation and acupuncture
• To overview the use of TENS and acupuncture for pain management, including indications, contraindications and risks.
• To outline the principles underpinning various techniques of TENS and acupuncture.
• To describe the research supporting the analgesic mechanisms of action of TENS and acupuncture.
• To summarize clinical research evidence on clinical effectiveness for TENS and acupuncture.
• To discuss why clinical experience of outcome when using TENS and acupuncture sometimes differs from some of the clinical research findings.
Part 1 Transcutaneous electrical nerve stimulation
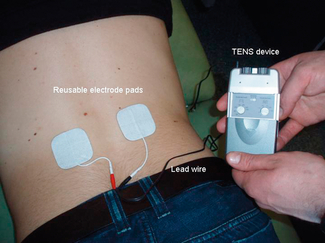
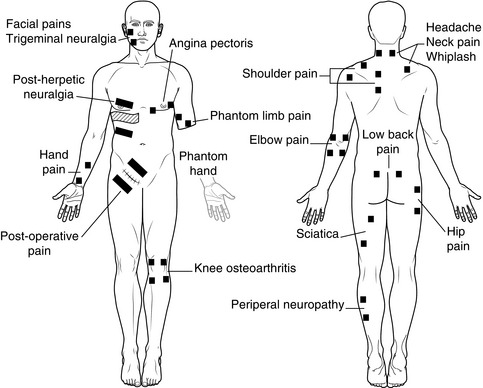
TENS is a non-invasive technique for symptomatic relief of pain (Table 14.1). A portable battery-powered device passes electrical currents transcutaneously across the intact surface of the skin via adhesive electrode pads in order to stimulate non-nociceptive peripheral afferents (Fig. 14.1). TENS is also used for non-painful conditions such as postoperative nausea and vomiting, wound and bone healing, incontinence, constipation and dementia. TENS is popular and devices can be purchased without prescription from retail outlets in many countries or over the internet.
Table 14.1
Painful conditions commonly treated using TENS
| Acute pain | Chronic pain |
| Post-operative pain Procedural pains such as colonoscopy Childbirth pain Dysmenorrhoea Angina pectoris Orofacial pain such as dental procedures Physical trauma, including fractured ribs | Musculoskeletal pains such as osteoarthritis, rheumatoid arthritis, low back pain and myofascial pain Neuropathic pains such as amputee stump and phantom pain, post-herpetic and trigeminal neuralgias, post-stroke pain, complex regional pain syndrome Nociceptive pain such as inflammatory pains and chronic wound pain Cancer pain associated with the disease such as cancer bone pain or with its treatment |
When used to relieve pain TENS is given as a stand-alone treatment or in combination with other types of pain relief. Approximately 50% of chronic pain patients who try TENS gain benefit in the short term, although this declines in the long term (Davies et al 1997). Reasons for discontinuing TENS include effects wearing off over time and a discrepancy between effort and pain relief. Hence, patient evaluation and education is critical for successful TENS therapy.
TENS effects are rapid in onset and can occur within minutes for some patients. This may be useful to manage severe breakthrough or incident pain. TENS does not produce many of the side effects associated with drugs, such as sedation, dizziness, nausea and disorientation. There is no potential for toxicity so it can be used for long periods of time without the fear of overdose. Interactions with drugs are few so TENS is often used in combination with analgesic medication to reduce drug dosage, side effects and costs (Bjordal et al 2003). TENS is most effective when patients administer it as required, following appropriate instruction by a healthcare professional.
DEFINITION
Standard TENS device
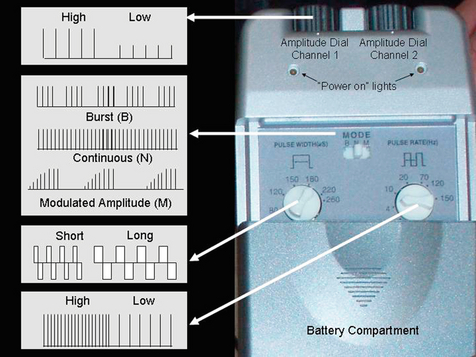
In general, standard TENS devices deliver biphasic pulsed currents at amplitudes between 1 and 60 milliamperes (mA), pulse durations (widths) between 50 and 500 μs and pulse frequencies (rates) between 1 and 250 pulses per second (pps). Pulse patterns include continuous (normal), burst (intermittent trains of pulses) and modulated amplitude, modulated frequency and modulated pulse duration (Table 14.2 and Fig. 14.2). Technical output specifications of standard TENS devices differ between manufacturers with only limited impact on physiological effects.
Table 14.2
The technical specifications of a standard TENS device
| Dimensions | Small device = 6 × 5 × 2 cm Large device = 12 × 9 × 4 cm (50–250 g) |
| Cost | £15–150 |
| Pulse waveform | Symmetrical or asymmetrical biphasic Monophasic |
| Pulse amplitude | Most devices deliver constant current output that is adjustable between 1 and 50 mA into a 1-kΩ load |
| Pulse duration | Adjustable between 50 and 500 μs |
| Pulse frequency (adjustable) | Adjustable between 1 and 200 pps |
| Pulse pattern | Adjustable continuous, burst (random frequency, modulated amplitude, modulated frequency, modulated pulse duration) |
| Channels | One or two |
| Batteries | PP3 (9 V) or AA |
| Additional features | Timer Some devices provide a range of pre-programmed settings |
TENS-like devices
A variety of TENS-like devices are available (Table 14.3). Some deliver microampere (μA) currents, much lower than a standard TENS device, some use pen-like electrodes, some deliver currents trans-cranially or trans-spinally. Critical reviews conclude that manufacturers’ claims about TENS-like devices are over-ambitious and practitioners should use a standard TENS device in the first instance. The remainder of this chapter will focus on a standard TENS device and will use the term ‘TENS’ to refer to a standard TENS device.
Table 14.3
Examples of commonly available TENS-like devices (adapted from Johnson 2008)
| Device | Characteristics |
| Action Potential Simulation (APS) (Odendaal & Joubert 1999) | Monophasic square pulse with exponential decay delivered by two electrodes Pulse amplitude low (< 25 mA), duration long (800 μs to 6.6 ms), frequency fixed at 150 pps |
| Codetron (Herman et al 1994) | Pulsed square wave delivered randomly to one of six electrodes Pulse amplitude low, duration long (1 ms), frequency low (2 pps) |
| H-Wave Stimulation (Blum et al 2008) | ‘Unique’ biphasic wave with exponential decay delivered by two electrodes Pulse amplitude low (< 10 mA), duration long (fixed at 16 ms), frequency low (2–60 pps) |
| Interferential therapy (interference currents) (Palmer & Martin 2008) | Two out-of-phase currents that interfere with each other to generate an amplitude modulated wave Traditionally, delivered by four electrodes; some devices have amplitude modulated waves that are premodulated within the device (two electrodes) Pulse amplitude low, amplitude modulated frequency 1–200 Hz, (carrier wave frequencies approximately 2–4 kHz) |
| Microcurrent, including transcranial stimulation and ‘acupens'(Koopman et al 2009, Tan et al 2006) | Modified square direct current with monophasic or biphasic pulses changing polarity at regular intervals (0.4 s) delivered by two electrodes Pulse amplitude low (1–600 μA with no paraesthesia), frequency depends on manufacturer (1–5000 pps) Many variants exist (e.g. transcranial stimulation for migraine and insomnia, acupens for pain) |
| Transcutaneous Spinal Electroanalgesia (TSE) (Palmer et al 2009) | Differentiated wave delivered by two electrodes positioned on spinal cord at T1 and T12 or straddling C3–C5 Pulse amplitude high yet no paraesthesic sensation generated, duration very short (1.5–4 μs, frequency high (600–10 000 pps) |
| Pain®Gone (Asbjorn 2000, Ivanova-Stoilova & Howells 2002) | Hand-held pen device using piezoelectric elements to deliver a low-ampere high-voltage single monophasic spiked pulse (e.g. 6 μA/15 000 V) Delivered by giving 30–40 individual shocks at the site of pain or on acupuncture points to generate non-noxious to mild noxious pin-prick sensation, repeated whenever pain returns |
| InterX® (Gorodetskyi et al 2007) | High-amplitude, short pulse width, dynamic waveform delivered by closely spaced metal electrodes moved across the surface of the skin Technology claims to identify changes in tissue properties to identify optimal treatment locations |
| Limoge current (Limoge & Dixmerias-Iskandar 2004, Limoge et al 1999) | High-frequency pulses interrupted with repetitive low-frequency cycle delivered by three electrodes (negative electrode between eyebrows and two positive electrodes in retro-mastoid region) Use to potentiate effects of opiates |
Adapted and reprinted by permission from MacMillan publishers Ltd: Nature Reviews Rheumatology. Johnson MI, Walsh DM, Pain: continued uncertainty of TENS’s effectiveness for pain relief; 6(6); copyright 2010.
PRINCIPLES UNDERPINNING TENS
The purpose of TENS is to selectively activate different populations of nerve fibres to initiate physiological responses that lead to pain relief. As the current amplitude of TENS is increased, large diameter myelinated non-nociceptive axons (Aβ) are activated first because they have lower thresholds of excitation (Fig. 14.3). The sensation experienced beneath the electrodes is often described as a ‘tingling’ or ‘pins and needles’ sensation (electrical paraesthesia) with an intensity that is non-painful. If current amplitude is increased further smaller diameter myelinated (Aδ) and unmyelinated (C-fibre) afferents become active and the user experiences a painful sensation, which is not desirable. Activation of low threshold (Aβ) axons without concurrent activation of higher threshold (Aδ and C-fibre) afferents is achieved using currents with small amplitudes (i.e. low intensity) and pulse durations between 50 and 500 μs. More nerve impulses can be generated in the axon by increasing the pulse frequency of TENS, although at higher frequencies this is limited by the absolute and relative refractory periods for the axon. In theory, TENS frequencies below 200 pps should be optimal.
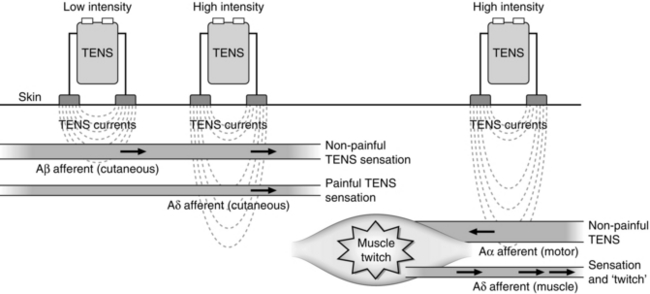
Fig. 14.3 Fibre recruitment by increasing the amplitude of electrical currents administered during conventional TENS.
CLINICAL TECHNIQUE
TENS outcome depends on stimulation technique, including choice of location, number and type of electrodes, and the electrical characteristics of currents. Protocols provided in manufacturers’ materials should be used to guide decisions rather than used as an inflexible regimen. TENS effects are dependent on pulse amplitude, because of its relationship to axon recruitment, and selective recruitment of different nerve fibres is achieved by the user titrating pulse amplitude whilst monitoring TENS intensity. Two commonly used TENS techniques are conventional TENS and acupuncture-like TENS (AL-TENS) (Table 14.4).
Table 14.4
The characteristics of different TENS techniques
| Characteristic | Conventional TENS | AL-TENS |
| Peripheral action | Generally stimulates cutaneous non-noxious afferents | Generally stimulates cutaneous and muscle nerves, leading to activity in small-diameter muscle and cutaneous afferents |
| Patient experience | Non-painful TENS paraesthesiae (minimal muscle activity) | Strong pulsating TENS sensation with simultaneous muscle twitching |
| Electrode location | Straddle site of pain (dermatomal) but if not successful try main nerve bundle, across spinal cord or contralateral positions | Over muscle belly or motor nerves (myotomal) at site of pain but if not successful try contralateral positions, trigger points or acupuncture points |
| Pulse amplitude (intensity) | Low (non-painful) | High (non-painful twitching) |
| Pulse frequency | High (10–200 pps) determined by patient preference | Low (< 5 pulses per second or < 5 bursts per second) |
| Pulse duration | Usually 50–200 μs determined by patient preference | Usually 100–200 μs Lower pulse width will generate a weaker TENS sensation yet still create muscle twitching |
| Pulse pattern | Continuous in first instance but determined by patient preference | Burst in first instance; if not successful or uncomfortable try amplitude modulated |
| Dose | Use as much and as often as needed, but have a break every hour or so | Use for no more than 30 minutes at a time a few times a day as muscle fatigue may develop. Delayed onset muscle soreness may occur the following day |
| Time course of pain relief | Rapid onset and offset of effects Pain relief tends to be spinal | Rapid onset delayed offset of effects Pain relief tends to be a combination of spinal and supraspinal |
Acupuncture-like TENS
AL-TENS was first described in the 1970s as a means to harness the mechanisms of action of TENS and acupuncture (Eriksson & Sjölund 1976). IASP defines AL-TENS as ‘hyperstimulation’ using currents that are low frequency (2–4 Hz), higher intensity (to tolerance threshold) and longer pulse width (100–400 μs). Often, AL-TENS is used to generate non-painful muscle twitching, which subsequently generates impulses in small-diameter peripheral afferents from deeper structures and activates descending pain inhibitory pathways and the release of endogenous opioids in the central nervous system (Johnson 1998).
AL-TENS is achieved using single pulses at frequencies below 10 pps (usually1–4 pps) or intermittent trains or bursts (2–4 Hz) of high-frequency pulses (~ 100 pps) at the painful site, over muscles, motor points, acupuncture points and trigger points. AL-TENS generates prolonged post-stimulation effects and is useful for patients resistant to conventional TENS (Eriksson & Sjölund 1976) and preferential to conventional TENS for radiating neurogenic pain, pain arising from deep structures and pain associated with altered skin sensitivity (for review see Johnson 1998).
CONTRAINDICATIONS, PRECAUTIONS AND ADVERSE EVENTS
Safety guidelines for TENS are available in Australia, the UK and the USA, and an excellent web-based resource is available at http://www.electrotherapy.org. Active implants such as pacemakers and ventricular assist devices (artificial hearts) are absolute contraindications for TENS, although TENS has been used in these situations following approval from the medical specialist. TENS interferes with internal cardiac defibrillators, producing inadvertent shocks (Holmgren et al 2008), and generates artefacts on fetal monitoring equipment (Bundsen & Ericson 1982). TENS should not be administered over the abdomen during pregnancy, on the neck or head for patients with epilepsy, or close to bleeding tissue, malignancy (except in palliative care) or active epiphysis. TENS can be used over metal implants, although care should be taken as there is one case report of skin burn after interferential therapy (Ford et al 2005). TENS appears to be safe when used with stents, percutaneous central catheters or drainage systems, although consideration must be given to mechanical stresses resulting from TENS-induced muscle contractions. TENS should be used with caution for patients on an anticoagulant treatment and not delivered close to transdermal drug-delivery systems because they may iontophoretically drive the drug through the skin, leading to toxicity. TENS should not be used while operating hazardous equipment, including motor vehicles.
Serious adverse events from TENS are rare and include respiratory compromise when using electrodes positioned on the anterior and posterior chest (Mann 1996) and repetitive epileptic seizures in individuals with coexisting psychomotor disturbances (Rosted 2001). There are reports of skin burns whilst using TENS-like devices due to inappropriate technique (Satter 2008). Contact dermatitis with redness and minor skin irritation may also occur. It is important to monitor the extent of this. TENS worsens pain in some individuals and may produce a vasovagal response, leading to nausea, dizziness and even syncope.
Principles of electrode placement
TENS electrodes are made of knitted stainless-steel fibres with adhesive gel, which enables flexibility across body contours. Sizes vary but 5 × 5 cm is most common. There is some evidence to suggest that small electrodes (0.8 × 0.8 cm2) are more comfortable for thin fat layers (0.25 cm) and stimulating superficial nerves, and larger electrodes (4.1 × 4.1 cm2) are more comfortable for thicker fat layers (2 cm) and stimulating deeper nerves (1.1 cm) (Alon et al 1994). Glove, sock and belt electrodes are also available, and more recently array electrodes have been developed in an attempt to target stimulation more precisely.
It is necessary to site electrodes on healthy skin with functional nerves and normal sensation, so a sharp-blunt skin test should be conducted before use. Electrodes can be placed up to ~ 15 cm apart and a dual-channel TENS device with four electrodes used for large areas of pain or for simultaneously treating pains at two body sites. During conventional TENS, electrodes are positioned so that TENS paraesthesiae cover the pain (Fig. 14.4). When this is not possible TENS should be positioned at alternative sites, including:
• over main nerves proximal to the site of pain (this is especially useful to project TENS sensations to distal body parts)
• on skin from an ipsilateral or contralateral dermatome
• paravertebrally at the spinal segment related to the location of the pain.
Electrodes should not be placed over:
• skin with increased sensitivity to touch (i.e. tactile allodynia) or dysaesthesia because it may aggravate the pain, although paradoxically this is not always the case
• an open wound, frail skin due to eczema, radiotherapy or reconstructive surgery
• the abdomen of a pregnant woman
• the anterior neck, because stimulation of baroreceptors at the carotid sinus may cause a hypotensive response and stimulation of laryngeal nerves may cause a laryngeal spasm
• the eyes, because it may increase intraocular pressure
• internally except in specific circumstances and with a specially designed device for dental analgesia or incontinence
• through the chest using electrodes placed on the anterior and posterior thorax as this interferes with intercostal muscle activity, leading to severely compromised breathing.
Principles of choosing electrical characteristics for TENS
Despite much being written about the optimal TENS settings for different conditions, no relationship has been determined. The critical determinant of outcome is pulse amplitude (intensity) and studies using healthy pain-free human volunteers show that strong non-painful TENS is superior to barely perceptible TENS (Lazarou et al 2009). Electrophysiological research suggests that different frequencies of TENS activate different neurophysiological mechanisms at submotor thresholds (see DeSantana et al 2008a for review). A systematic review of studies using pain-free volunteers exposed to experimentally induced pain concluded that hypoalgesia during strong non-painful TENS was not influenced by pulse frequency, although most studies were underpowered (Chen et al 2008). Subsequently, appropriately powered studies have found that strong non-painful TENS at 80 pps was superior to 3 pps at reducing experimental mechanical pain and ischaemic pain in healthy participants (Chen & Johnson 2010), although 3 pps was superior to 80 pps for cold-pressor pain.
Clinical practice and dosage
Electrodes are left in situ and the device attached to a trouser belt so that patients can administer TENS intermittently throughout the day on an as-needed basis. The intensity of TENS fades due to habituation, so users increase amplitude to maintain a strong non-painful TENS. Some patients report that TENS effects wear off with repeated use (i.e. tolerance to TENS) and repeated use of TENS generates opioid tolerance in animals, with cholecystokinin and NMDA receptors being involved. Generating a novel stimuli using modulated (Chen & Johnson 2009) and random (Pomeranz & Niznick 1987) delivery of currents has been shown to reduce habituation and tolerance (Hingne & Sluka 2008). Changing electrode placement or temporarily withdrawing TENS may also help.
New TENS patients should be given a supervised trial of TENS to ensure it does not aggravate pain and to educate them on safe technique and expected therapeutic outcome (Box 14.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree