Tracheostomy
Scott E. Kopec
Ciaran J. McNamee
The terms tracheotomy and tracheostomy are interchangeable. Derived from the Greek words tracheia arteria (rough artery) and tome (incision), tracheotomy refers to the operation that opens the trachea, while tracheostomy results in the formation of a tracheostoma, or the opening itself. Although tracheostomy is referred to intermittently from the first century BC [1, 2 and 3], it was not performed regularly until the 1800s when used by Trousseau and Bretonneau in the management of diphtheria. In the early 1900s, Chevalier Jackson [4], describing refinements to the operation, warned against tracheostomy involving the cricothyroid membrane or first tracheal ring because of the risk of injury to the cricoid cartilage and subsequent subglottic stenosis. During this period, the procedure was used to treat difficult cases of respiratory paralysis from poliomyelitis. Largely because of improvements in tubes and advances in clinical care, endotracheal intubation has become the treatment of choice for short-term airway management [3, 5].
Although tracheostomy is occasionally required in critically ill and injured patients who cannot be intubated for various reasons (e.g., cervical spine injury, upper airway obstruction, laryngeal injury, anatomical considerations), the most common use of this procedure today is to provide long-term access to the airway in patients who are dependent on mechanical ventilation. With improvements in critical care medicine over the past 30 years, more patients are surviving initial episodes of acute respiratory failure, trauma, and extensive surgeries and are requiring prolonged periods of mechanical ventilation. It is now common practice to expeditiously convert these patients from translaryngeal intubation to tracheostomy. Tracheostomy is becoming a very common procedure in the intensive care unit (ICU). The prevalence of tracheostomies in ICU patients is at least 10% [6].
In this chapter we will review the indications, contraindications, complications, and techniques associated with tracheostomy. We will also discuss the timing of converting an orally intubated patient to tracheostomy.
Indications
The indications for tracheostomy can be divided into three general categories: to bypass obstruction of the upper airway, to provide an avenue for tracheal toilet and removal of retained secretions, and to provide a means for ventilatory support. These indications are summarized in Table 12-1 [7, 8, 9, 10, 11, 12 and 13].
Anticipated prolonged ventilatory support, especially patients receiving mechanical ventilation via translaryngeal intubation, is the most common indication for placing a tracheostomy in the ICU. There are several advantages and disadvantages of both translaryngeal intubation and tracheostomy in patients requiring prolonged ventilator support, and these are summarized in Table 12-2 [14, 15 and 16]. Most authors feel that when the procedure is performed by a skilled surgical group, the potential benefits of tracheostomy over translaryngeal intubation for most patients justifies the application despite its potential risks. However, there are no detailed clinical trials consistently confirming the advantages of tracheostomy in patients requiring prolonged mechanical ventilation.
Contraindications
There are no absolute contraindications to tracheostomy. Certain conditions, however, warrant special attention before anesthesia and surgery. In patients undergoing conversion from translaryngeal intubation to a tracheostomy for prolonged ventilatory support, the procedure should be viewed as an elective or semielective procedure. Therefore, the patient should be as medically stable as possible, and all attempts should be made to correct existing coagulopathies, including uremia. For obvious reasons, emergent tracheostomies for upper airway obstruction may need to be preformed when the patient is unstable or has a coagulopathy.
Timing of Tracheostomy
When to perform a tracheostomy on an intubated, critically ill patient has been very controversial. Recommendations range from performing a tracheostomy after just 3 days of translaryngeal intubation due to the risk of mucosal damage to the larynx and vocal cords [17], to more than 21 days based on reported high complication rates of open tracheostomies [18]. The reported low morbidity and mortality of bedside percutaneous tracheostomies confirm that it does not appear justified to avoid tracheostomy based solely on the risk of operative complications. The lower morbidity and mortality of the procedure shifts the risk-benefit ratio to more of a benefit in the majority of patients requiring prolonged ventilator support.
A more up-to-date approach regarding the timing of converting an intubated patient to a tracheostomy has been suggested by Heffner [14]. This recommendation takes into account the very low mortality and morbidity associated with placing a tracheostomy, plus the advantages and disadvantages of both translaryngeal intubation and tracheostomy. In summary, if a patient remains ventilator dependent after a week of translaryngeal intubation, a tracheostomy can be considered.
Whether to perform the procedure or not should depend on the anticipated duration of ventilatory support and the benefits of a tracheostomy in that specific patient. If the patient appears to have minimal barriers to weaning, and appears likely to be successfully weaned and extubated within 7 days, tracheostomy should be avoided. In those patients whom it appears unlikely that they will successfully be weaned and extubated in 7 days, tracheostomy should be strongly considered. For those patients whose ability to wean and be extubated is unclear, the patient’s status should be readdressed daily [14].
Whether to perform the procedure or not should depend on the anticipated duration of ventilatory support and the benefits of a tracheostomy in that specific patient. If the patient appears to have minimal barriers to weaning, and appears likely to be successfully weaned and extubated within 7 days, tracheostomy should be avoided. In those patients whom it appears unlikely that they will successfully be weaned and extubated in 7 days, tracheostomy should be strongly considered. For those patients whose ability to wean and be extubated is unclear, the patient’s status should be readdressed daily [14].
TABLE 12-1. Indications for Tracheostomy | ||
|---|---|---|
|
Some studies have suggested that early tracheostomy may be beneficial in some specific instances. Patients with blunt, multiple organ trauma have a shorter duration of mechanical ventilation, fewer episodes of nosocomial pneumonia [19], and a significant reduction in hospital costs [20] when the tracheostomy is performed within 1 week of their injuries. Similar benefits have been reported in patients with head trauma and poor Glasgow Coma Score [21, 22 and 23], and patients with thermal injury [24], if a tracheostomy is performed within a week after the injury.
Several recent studies [25, 26 and 27], coupled with a meta-analysis [28] sought to determine if performing an “early tracheostomy,” that is, within 7 days of translaryngeal intubation, had any advantages over a “late tracheostomy” (greater than 7 days) in critically ill patients requiring mechanical ventilation. The meta-analysis combined five prospective studies and included 406 patients and suggested that early tracheostomy resulted in a decrease length of ICU stay by an average of 15.3 days, and a decrease in duration of mechanical ventilation by an average of 8.5 days [28]. Potential reasons for the decrease in duration of mechanical ventilation include easier weaning due to less dead space, less resistance, and less obstruction due to mucus plugging in patients with tracheostomies. There was no significant increase in hospital mortality or risk of hospital acquired pneumonia. However, there are obvious limitations to the meta-analysis. Currently there are three large randomized trials being performed in Europe addressing the timing of tracheostomy in critical ill patients on mechanical ventilation. Hopefully these studies, when concluded, can result in specific guidelines to the timing of tracheostomy.
| ||||||||||||
Procedures
Emergency Tracheostomy
Emergency tracheostomy is a moderately difficult procedure requiring training and skill, experience, adequate assistance, time, lighting, and proper equipment and instrumentation. When time is short, the patient uncooperative, anatomy distorted, and the aforementioned requirements not met, tracheostomy can be very hazardous. Emergency tracheostomy comprises significant risks to nearby neurovascular structures, particularly in small children in whom the trachea is small and not well defined. The risk of complications from emergency tracheostomy is 2 to 5 times higher than for elective tracheostomy [29, 30]. Nonetheless, there are occasional indications for emergency tracheostomy [31], including transected trachea, anterior neck trauma with crushed larynx [32], severe facial trauma, acute laryngeal obstruction or near impending obstruction, and pediatric (earlier than 12 years) patients requiring an emergency surgical airway in whom an cricothyrotomy is generally not advised. In emergency situations when there is inadequate
time or personnel to perform an emergency tracheostomy, a cricothyrotomy may be a more efficient and expedient manner to provide an airway.
time or personnel to perform an emergency tracheostomy, a cricothyrotomy may be a more efficient and expedient manner to provide an airway.
Cricothyrotomy
Cricothyrotomy (cricothyroidotomy) was condemned in Jackson’s [4] 1921 article on high tracheostomies because of excessive complications, particularly subglottic stenoses [33]. He emphasized the importance of the cricoid cartilage as an encircling support for the larynx and the trachea. However, a favorable report of 655 cricothyrotomies, with complication rates of only 6.1%, and no cases of subglottic stenoses [34], prompted reevaluation of cricothyrotomy for elective and emergency airway access. Further reports emphasized the advantages of cricothyrotomy over tracheostomy. These include technical simplicity, speed of performance, low complication rate [35, 36, 37, 38 and 39], suitability as a bedside procedure, usefulness for isolation of the airway for median sternotomy [38, 40], radical neck dissection [41], lack of need to hyperextend the neck, and formation of a smaller scar. Also, because cricothyrotomy results in less encroachment on the mediastinum, there is less chance of esophageal injury and virtually no chance of pneumothorax or tracheal arterial fistula [35]. Despite these considerations many authorities currently recommend cricothyrotomy should be used as an elective long-term method of airway access only in highly selective patients [33, 35, 41, 42 and 43]. Use of cricothyrotomy in the emergency setting, particularly for managing trauma, is not controversial [44, 45 and 46]. Emergency cricothyrotomy is useful because cricothyrotomy requires a small number of instruments and less training than tracheostomy and can be performed quickly as indicated as a means of controlling the airway in an emergency when oral or nasotracheal intubation is nonsuccessful or contraindicated. In emergency situations, translaryngeal intubations fail because of massive oral or nasal hemorrhage or regurgitation, structural deformities of the upper airway, muscle spasm and clenched teeth, and obstruction by foreign body through the upper airway [44]. Cricothyrotomy finds its greatest use in trauma management, axial or suspected cervical spine injury, alone or in combination with severe facial trauma, where nasotracheal and orotracheal intubation is both difficult and hazardous. Thus cricothyrotomy has an important role in emergency airway management [45].
Use and Contraindications
Cricothyrotomy should not be used to manage airway obstruction that occurred immediately after endotracheal extubation because the obstruction may be found below the larynx [4, 35, 45]; likewise, with primary laryngeal trauma or diseases such as tumor or an infection, cricothyrotomy may prove useless. It is contraindicated in infants and in children younger than 10 to 12 years, under all circumstances [45]. In this age group, percutaneous transtracheal ventilation may be a temporizing procedure until the tracheostomy can be performed.
Anatomy
The cricothyroid space is no larger than 7 to 9 mm in its vertical dimension, smaller than the outside diameter of most tracheostomy tubes (outside diameter 10.0 mm). The cricothyroid artery runs across the midline in the upper portion, and the membrane is vertically in the midline. The anterior superior edge of the thyroid cartilage is the laryngeal prominence. The cricothyroid membrane is approximately 2 to 3 cm below the laryngeal prominence and can be identified as an indentation immediately below the thyroid cartilage. The lower border of the cricothyroid membrane is the cricoid cartilage [38, 39, 43, 46, 47 and 48]. A description of the cricothyrotomy procedure is contained in standard surgical texts.
Complications
The report of incidents of short- and long-term complications of cricothyrotomy ranges from 6.1% [34] with procedures performed in an elective, well-controlled, carefully selected cases, to greater than 50% [44, 46, 49] for procedures performed under emergency or other suboptimal conditions. The incidence of subglottic stenosis after cricothyrotomy is 2% to 3% [33, 35]. This major complication occurs at the tracheostomy or cricothyrotomy site but not at the cuff site [50]. Necrosis of cartilage due to iatrogenic injury to the cricoid cartilage or pressure from the tube on the cartilage may play a role [45]. Possible reasons that subglottic stenoses may occur more commonly with cricothyrotomy than with tracheostomy are as follows: the larynx is the narrowest part of the laryngotracheal airway; subglottic tissues, especially in children, are intolerant of contact; and division of the cricothyroid membrane and the cricoid cartilage destroy the only complete rings supporting the airway [3, 33]. Furthermore, the range of tube sizes is limited due to the rigidity of the surrounding structures (cricoid and thyroid cartilage), and the curvature of the tracheostomy tube at this level may obstruct the airway due to potential posterior membrane impingement [51]. Prior laryngotracheal injury, as with prolonged translaryngeal intubation, is a major risk factor for the development of subglottic stenosis after cricothyrotomy [33, 35].
The association of cricothyrotomy with these possible complications leads most authorities to consider replacing a cricothyrotomy within 48 to 72 hours with a standardized tracheostomy procedure. This is commonly done by an open surgical tracheostomy (OST), which occurs between the second and third tracheal ring as compared to a percutaneous dilational tracheostomy (PDT), which usually occurs between the cricoid cartilage and the first ring or the first and second ring [51].
Tracheostomy Procedures in the Intensive Care Unit
Tracheostomy is one of the most common surgical ICU procedures and it is commonly performed for weaning purposes and for airway protection for patients requiring prolonged ventilation. There are two major techniques for tracheostomy with various modifications that are described below. The different surgical tracheostomy techniques are well described in the references for this chapter and are briefly described below [52, 53, 54].
Open Surgical Tracheostomy
In OST the patient’s neck is extended and the surgical field is exposed from the chin to several inches below the clavicle. This area is prepped and draped and prophylactic antibiotics are administered at the discretion of the surgeon. A vertical or horizontal incision may be used; however, a horizontal incision will provide a better cosmetic result. The platysma muscle is divided in line with the incision and the strap muscles are separated in
the midline. The thyroid isthmus is then mobilized superiorly or is divided as needed to access the trachea. In the event of a low-lying cricoid cartilage, dissection on the anterior wall of the trachea helps to mobilize the trachea out of the mediastinum, and also the use of a cricoid hook will elevate the trachea to expose the second or third tracheal ring. Following identification of the second or third tracheal ring, a vertical tracheostomy is created or a tracheal flap (Bjork flap) is fashioned to create a fistulous tract by suturing the tracheal mucosal flap to the skin in the incision.
the midline. The thyroid isthmus is then mobilized superiorly or is divided as needed to access the trachea. In the event of a low-lying cricoid cartilage, dissection on the anterior wall of the trachea helps to mobilize the trachea out of the mediastinum, and also the use of a cricoid hook will elevate the trachea to expose the second or third tracheal ring. Following identification of the second or third tracheal ring, a vertical tracheostomy is created or a tracheal flap (Bjork flap) is fashioned to create a fistulous tract by suturing the tracheal mucosal flap to the skin in the incision.
Variations on this technique include the use of retention sutures through the lateral aspect of the tracheal walls for retraction purposes during tracheostomy tube insertion and for expeditious reinsertion of a tracheostomy tube in the event of accidental tube decannulation [54, 55].
Percutaneous Dilation Techniques
The PDT are divided into several techniques; however, all are alike in that they depend on the basic technique of guidewire placement through the anterior tracheal wall, followed by dilation over this guidewire to create a tracheal stoma. This is all accomplished with provision of adequate monitoring of O2 saturations as well as adequate monitoring of cardiac rhythm and blood pressure. To achieve early successful tracheal cannulation within the operating room use end-tidal CO2 monitoring via the fresh tracheostomy tube and in the ICU by capnography [56]. There are several different modifications from the original technique that was described by Ciaglia et al. [57] in 1988.
In the original technique, following the perforation of the first or second tracheal membrane, a tracheal stoma is created by the passage of several progressive larger dilators. The tracheostomy tube is carried into the stoma on an appropriately sized dilator once a sufficient stoma has been created.
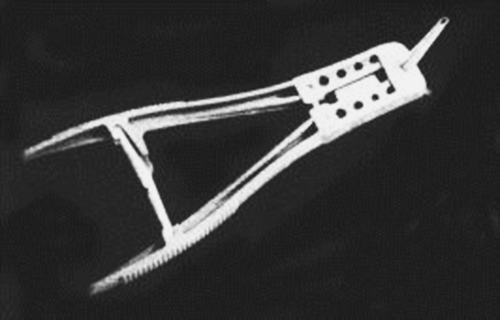
A simple modification of this technique was first developed in 1989 by Schachner et al. [58] (Rapitrach instrument) (Fig. 12-1), which is a forceps device with a cutting edge on a cone that is introduced over the guidewire. Following tracheal penetration an adequate tract is created by pressure on the handles, which open the jaws of the cone to create a stoma. This instrument is not available in the US market because of posterior tracheal wall tears and lacerations of the balloon cuff of the new tracheostomy tube.
Griggs [59] in 1990 described a similar apparatus to the Rapitrach but with reduced tendency for tracheal or cuff lacerations. This device again accommodates a central guidewire in a tracheal spreader but lacks the sharp cutting edge. However, there is a potential with this instrument to damage contiguous structures or the posterior wall of the trachea.
In 1999, Ciaglia modified the original sequential dilating instrument to use only a single dilator covered with a hydrophilic membrane, which is progressively tapered to open the tracheal stoma with one smooth passage. The advantage of this technique in comparison to the original Ciaglia technique is the rapidity with which this can be performed and the prevention of the loss of tidal volume, which occurs with each progressive dilatation when the dilator is removed from the airway [60, 61]. However, concern has been expressed about the potential for anterior cartilage fractures or posterior tracheal wall damage due to the excessive force used to make tracheal stoma formation with this technique.
The Perc Twist (Fig. 12-2) has been recently introduced, which consists of a screwlike dilator that follows the guidewire into the tracheal lumen and is designed to lift upward and thereby theoretically prevent posterior tracheal wall damage. However, studies have not clearly shown the value of the Perc Twist device in comparison to the single dilator technique [62].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree